- Submissions

Full Text
Advancements in Case Studies
Peripheral Facial Nerve Paralysis After Real-Time Ultrasound-Guided Percutaneous Biopsy: A Case Report and Literature Review
Yanling Zheng1, Yingying Qi2, Di Li2, Xinyu Liu3 and Cun Liu1*
1University of Jinan, Jinan, China
1Central Hospital Affiliated to Shandong First Medical University, Jinan, China
1Zhengzhou University, Zhengzhou, China
*Corresponding author: Cun Liu, Central Hospital Affiliated to Shandong First Medical University, Jinan, 250013, Shandong Province, China
Submission:February 13, 2023;Published: February 20, 2023

ISSN 2639-0531Volume3 Issue5
Abstract
We report a case of a 65-year-old man who developed peripheral facial nerve paralysis after perioperative infiltration of lidocaine and successful biopsy. He was then observed by his daughter to have a crooked smile and slurred speech after going back to in-patients department. The clinical signs of facial paralysis started to regress 1 hour later, and then, the facial nerve paralysis was resolved completely with no neurological sequelae after another 2 hours. We assumed this to be caused by the direct action of the local anesthetic agent on the facial nerve.
Keywords:Ultrasound-guided percutaneous biopsy; lidocaine; Facial nerve; Facial paralysis
Introduction
Ultrasound-guided percutaneous biopsy as a well-established means with safety and confers minimal risk of complications is frequently used in the diagnosis, prognosis and management of patients with focal or diffuse disease in solid organs. Reduction of pain is an important part of the management of ultrasound-guided percutaneous biopsy. Lidocaine used as a local anesthetic for minor surgery is characterized by a rapid onset of action and intermediate duration of efficacy. We are describing a case of temporary facial nerve paralysis encountered during ultrasound-guided percutaneous biopsy and review the literature on this rare complication.
Case Presentation
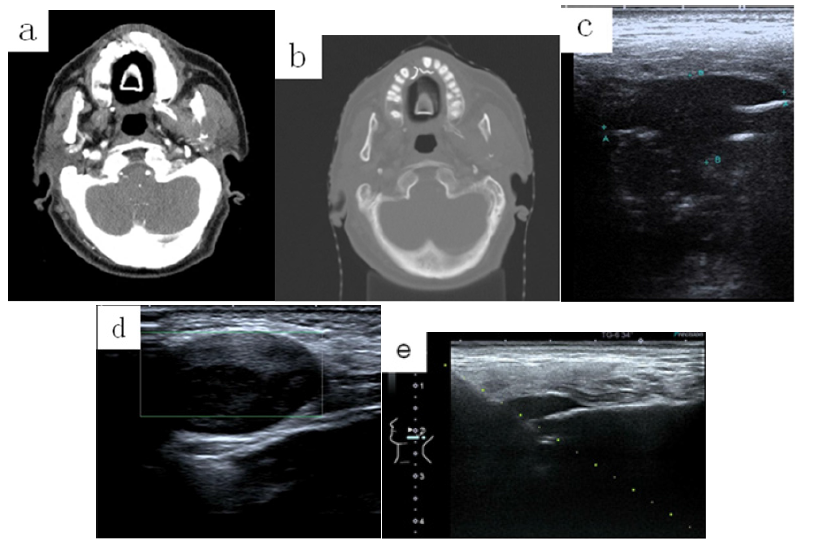
A 65-year-old man, who had lung adenocarcinoma diagnosed two years previously and treated with surgery and chemotherapy, was referred to our hospital with a paresthesia on left side of the chin and a lump in the right wrist. Physical examination findings were a 2cm subcutaneous mass in the right wrist on palpation. The lump was of hard texture, with a certain degree of pain. A computed tomography (CT) scan of the head revealed an oral soft tissues masse (2.4×2.9cm) in left temporomandibular joint region involving both the inner and outer cortices with mixed linear radiolucent and radiopaque areas forming a sunburst (Figure 1a,1b), suggesting a mandible bone metastases secondary to pulmonary adenocarcinoma.
Ultrasound-guided percutaneous biopsy was recommended for the soft tissues masse on left side of the chin (Figure 1c) and the lump in the right wrist (Figure 1d). The potential risks, benefits and alternatives of paracentesis were discussed with the patient, including possible complications of bleeding, infection and damage to adjacent structures. After all of his questions were answered, written informed consent was obtained. After sterile preparation of the skin and infiltration of the skin puncture site with 1% lidocaine, 5mL, an 18-gauge core biopsy needle was advanced to the lump in the right wrist and the soft tissues masse on left side of the chin utilizing continuous real-time sonographic guidance (Figure 1e).
Figure 1: Representative computed tomography (CT) and ultrasound scan images of the soft tissues masses on left side of the chin and the lump in the right wrist. (a) CT scan image of the soft tissues masse (2.4×2.9cm) in left temporomandibular joint region in transverse plane. (b) CT scan image revealed the soft mass involving both the inner and outer cortices with mixed linear radiolucent and radiopaque areas forming a sunburst. (c) Ultrasound measurement the soft tissues masse on left side of the chin in transverse plane. (d) Ultrasound image of the lump in the right wrist in sagittal plane. (e) Ultrasound-guided percutaneous biopsy for the soft tissues masse on left side of the chin utilizing continuous real-time sonographic guidance.
Tissue cores were obtained through the target. The tissue cores were submitted to surgical pathology in formalin for histological analysis. Sterile bandages were applied. The patient tolerated the procedure well and there was no evidence of significant immediate complication. He was then observed by his daughter to have a crooked smile and slurred speech after going back to inpatients department. Physical examination disclosed a distraught because of the facial palsy. His general examination was normal. Neurologic examination revealed a dense, right-sided facial paralysis that included the left frontalis muscle. Efferent portion of the corneal reflex was diminished on the left side. The patient did not complain of any hyperacusis, and tearing and taste were intact. Sensory examination was normal. The remainder of the neurologic examination was unremarkable. According to the short administration of local anerthesia, this phenomenon might be attributed to direct local infiltration of the facial nerve and explains the acute onset, a diagnosis of immediate facial nerve paralysis was made. The diagnosis was discussed with the patient and his daughter. The clinical signs of facial paralysis started to regress 1 hour later, and then, the facial nerve paralysis was resolved completely with no neurologic sequelae after another 2 hours. Pathology report indicates the soft tissues mass on left side of the chin was mandible bone metastases secondary to pulmonary adenocarcinoma and the soft tissues mass in the right wrist was a soft tissue neurilemmoma. The patient’s case was discussed at our multidisciplinary committee: the radiotherapist and oncologist recommended chemotherapy and radiation therapy (RT) on the bone metastasis. He received systemic chemotherapy and symptomatic and palliative RT on the left mandible bone lesion.
Discussion
Lung cancer is the most frequently diagnosed cancer and the leading cause of cancer-related mortality in economically developed and developing countries [1]. Lung cancer frequently metastasizes to bone, with 36% of patients presenting with bone lesions at autopsy [2]. However, mandible metastasis from lung cancer is a rare condition, major symptoms are painful swelling, paresthesia, bleeding and increasing tooth mobility [3]. The patient in our case has similar symptoms with paresthesia on the left side of the chin and a lump in the right wrist. The diagnosis of a metastatic lesion in the mandible and in the right wrist is challenging [4].
Ultrasound-guided percutaneous biopsy is a feasible and safe, minimally invasive surgical technique that provides reliable clinical results. The mandible is an interesting site because of the various and different tissues that may be involved in the ultrasound-guided percutaneous biopsy procedures. The facial nerve passes through the parotid gland and mandible. It controls the muscles of facial expression, and functions in the conveyance of taste sensations from the anterior two-thirds of the tongue and oral cavity [5]. There may be a number of reasons that may result in facial nerve paralysis. The paralysis of the facial nerve in our case may be explained by the diffusion of lidocaine to the facial nerve because of deep local anesthesia about the biopsy site. The phenomenon that the patient suddenly experiences a crooked smile and slurred speech but recovers spontaneously within hours has been attributed to direct local infiltration of the facial nerve and explains the acute onset. Adverse effects related to local anesthetics have not undergone a systematic study in clinical trials. There are a few reported cases of facial nerve paralysis after local anesthetics. Perekrest and Rakotoarinivo [6] had reported one case of facial nerve paralysis after local anesthesia administration in the Russian literature [6]. In their report, peripheral facial nerve paralysis appeared immediately after eritonsillar infiltration with a local anesthetic in a young male patient. The surgery was discontinued and facial nerve function resolved completely after 4 hours. The following week, the patient underwent bilateral tonsillectomy under local anesthesia and facial nerve paralysis appeared again, resolving after a few hours. Shlizerman [7] had reported a case of a 4-year-old boy who developed peripheral facial nerve paralysis after perioperative infiltration of bupivacaine and uneventful tonsillectomy. The paralysis was noticed a few minutes after extubation and resolved completely after 8 hours. Shlizerman [7] assumed this to be caused by the direct action of the local anesthetic agent on the facial nerve [7]. Weksler [8] had reported one case of recurrent nerve anesthesia after the same procedure [8]. The occurrence of facial nerve paralysis during dental surgeries under local anesthesia offers further support for our assumption that deep peritonsillar infiltration with bupivacaine can result in facial paralysis [9,10]. Kuo-Sheng Lee [11] reported two cases who developed unilateral peripheral facial palsy immediately after adenotonsillectomy in children, The facial palsy in both cases completely recovered in 6 and 3h respectively without any treatment. They assumed the possible mechanism was deep infiltration of the local anesthetics into parapharyngeal space and then the direct action on the facial nerve [11]. Michał Lubszczyk [12] reported one case of a 5-yearold patient who suffered from unilateral peripheral facial nerve palsy and laryngeal spasm following adenotonsillectomy. Paresis was observed immediately after the transfer of the patient to the postoperative room. The activity of facial muscles was restored within 2 hours from the beginning of the surgery. They assumed that this was the direct effect of an anesthetic on the extracranial processes of the facial nerve [12].
Facial paralysis may occur due to the biopsy procedure or the edema and the bleeding of the tumor after the biopsy. In this case the facial paralysis may follow immediately the biopsy procedure due to direct damage to the facial nerve. Stay [13] believe that it is difficult to injure the facial nerve directly in the absence of either an aberrant nerve or a congenital anomaly of the parotid gland [13]. Patients with facial nerve paralysis resulting from edema and the bleeding of the tumor after the biopsy usually present with a progressive, twitching paralysis, other neurological signs, or a recurrent Bell’s palsy-type presentation. In this situation, the patient suddenly experiences a crooked smile and slurred speech but recovers spontaneously within hours, therefore, the biopsy procedure or the edema and the bleeding of the tumor after the biopsy was not the cause of the facial paralysis.
Conclusion
In conclusion, ultrasound-guided percutaneous biopsy is a safe method for the diagnosis, prognosis and management of patients with focal or diffuse disease in solid organs and major complications are rare. Temporary facial nerve paralysis should be considered as a rare complication of ultrasound-guided percutaneous biopsy. Although the prognosis is usually favorable, but the knowledge of the rare complications may be helpful in the management of ultrasound-guided percutaneous biopsy.
Conflict of Interest
There are no financial or other relations that could lead to a conflict of interest.
References
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, et al. (2011) Global cancer statistics. CA Cancer J Clin 61(2): 69-90.
- Dirican N, Gunes S, Karakaya Y, Kaya V, Cerci S, et al. (2014) Mandible bone metastases secondary to pulmonary adenocarcinoma. Med Arch 68(5): 356-368.
- Lim SY, Kim SA, Ahn SG, Kim SG, Hwang HK, et al. (2006) Metastatic tumors to the jaws and oral soft tissues: A retrospective analysis of 41 Korean patients. Int J Oral Maxillofac Surg 35(5): 412-415.
- Hirshberg A, Shnaiderman-Shapiro A, Kaplan I, Berger R (2008) Metastatic tumors to the oral cavity-pathogenesis and analysis of 673 cases. Oral Oncol 44(8): 743-752.
- Gupta S, Mends F, Hagiwara M, Fatterpekar G, Roehm PC (2013) Imaging the facial nerve: A contemporary review. Radiol Res Pract 2013: 248039.
- Perekrest AI, Rakotoarinivo ZM (1983) Neuritis of the facial nerve as a complication of local anesthesia and tonsillectomy. Vestn Otorinolaringol 3: 77-78.
- Shlizerman L, Ashkenazi D (2005) Peripheral facial nerve paralysis after peritonsillar infiltration of bupivacaine: A case report. Am J Otolaryngol 26(6): 406-407.
- Weksler N, Nash M, Rozentsveig V, Schwartz JA, Schily M, et al. (2001) Vocal cord paralysis as a consequence of peritonsillar infiltration with bupivacaine. Acta Anaesthesiol Scand 45(8): 1042-1044.
- Tiwari IB, Keane T (1970) Hemifacial palsy after inferior dental block for dental treatment. Br Med J 1(5699): 798.
- Bernsen PL (1993) Peripheral facial nerve paralysis after local upper dental anaesthesia. Eur Neurol 33(1): 90-91.
- Kuo-Sheng Lee, Kuan-Ling Lin, Yu-Chun Chen (2012) Peripheral facial palsy after adenotonsillectomy in children. International Journal of Pediatric Otorhinolaryngology 76(9): 1379-1381.
- Michał Lubszczyk, Anna Łuczyńska-Sopel, Dariusz Polaczkiewicz (2018) Facial nerve palsy and laryngospasm as a complication of local anaesthesia during adenotonsillectomy. Auris Nasus Larynx 45(5): 1113-1115.
- Stay PI, Gregg G (1951) Bell’s palsy following local anaesthesia. Br Dent J 91: 292-293.
© 2023 Cun Liu. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






