- Submissions

Full Text
Advancements in Case Studies
Basal Cell Carcinoma in a Filipino with Oculocutaneous Albinism:A Case Report
Marianne Isabel A Sayo MD, DPDS* and Arunee Siripunvarapon MD, FPDS
East Avenue Medical Center, Department of Dermatology, Metro Manila, Philippines
*Corresponding author: Marianne Isabel A Sayo, MD, DPDS, East Avenue Medical Center, Department of Dermatology, Quezon City, Metro Manila, Philippines, E-mail: mariel.sayo@yahoo. com
Submission:October 03, 2022;Published: October 31, 2022

ISSN 2639-0531Volume3 Issue4
Abstract
Background: Oculocutaneous albinism (OCA) is an autosomal recessive disorder characterized by defects
in melanin synthesis that affect the skin, eyes, and hair. This melanin deficiency causes albino patients to
be at a higher risk for sun-induced skin cancers. Herein, this report highlights the rare occurrence of basal
cell carcinoma (BCC) in a Filipino with oculocutaneous albinism.
Case: A 25-year-old Filipino female presented with a 1-year history of a keratotic plaque on the neck.
She had milky-white skin, silvery hair, and blue eyes at birth that gradually darkened with age with
progressive photosensitivity and photophobia. No family history of albinism nor consanguineous
marriage was noted. Physical examination revealed a fair-skinned patient with brown hair, gray-tinted
irises, marked nystagmus, and decreased visual acuity. Clinical and genetic counseling was done leading
to the diagnosis of OCA IB. In addition to this, an erythematous keratotic plaque on the left side of the
neck was noted and upon dermoscopy, short fine telangiectasias, ulceration and yellow crusts were seen.
Skin biopsy was done that showed tumor islands with atypical basaloid cells and a retraction artifact
diagnostic of nodular BCC. She underwent Mohs micrographic surgery for her BCC, was recommended to
follow-up regularly for screening, and was advised strict sun protection.
Conclusion: The hypopigmented skin of this patient with oculocutaneous albinism predisposed her to
severe skin damage that led to the development of basal cell carcinoma. Due to melanin deficiency, it is
recommended to closely observe, regularly follow-up, and advise strict sun protection as early as possible
to prevent skin cancer in this population.
Keywords:Oculocutaneous albinism, basal cell carcinoma, squamous cell carcinoma, melanin, Nonmelanoma skin cancer, Mohs micrographic surgery, ultraviolet
Abbreviations:OCA: Oculocutaneous Albinism; BCC: Basal Cell Carcinoma; UV: Ultraviolet; NMSC: Nonmelanoma Skin Cancer; H&E: Hematoxylin & Eosin
Introduction
Oculocutaneous albinism (OCA) is an autosomal recessive genetic disorder associated with reduced melanin biosynthesis. Clinical manifestations include hypopigmented skin, eyes, and hair, with visual disturbances such as impaired visual acuity, nystagmus, and photophobia [1]. Globally, OCA has an overall prevalence rate of approximately 1 in 17,000 with eight subtypes. Of these, the OCA1 subtype is the most common with milder mutations that allow residual tyrosinase activity. This makes affected individuals gain some pigment over time with slightly improved visual acuity [2].
Melanin is a photoprotective pigment that protects the skin from the harmful effects against ultraviolet (UV) radiation and oxidative damage to DNA [3]. The lack or absence of melanin predisposes skin to UV-induced damage, which includes sunburns, blisters, and actinic keratosis wherein sun-exposed areas located at the face, neck, and shoulders, are particularly prone to transforming into skin malignancies [1,2]. In albino individuals, they commonly develop squamous cell carcinoma (SCC) but other less frequently encountered malignancies were basal cell carcinoma, dysplastic nevus, and melanoma [3]. In addition to this, many international studies have investigated the prevalence of nonmelanoma skin cancer (NMSC) such as BCC and SCC in patients with albinism. However, there were no studies of this nature in the Philippines which highlights the rare occurrence of basal cell carcinoma in a Filipino with oculocutaneous albinism. Persons of color have an increased morbidity and mortality associated with NMSC and this, in combination with the lack of resources or education devoted to skin cancer prevention in the Philippines, highlights the need for more emphasis on this issue [2]. Early diagnosis is critical to inform proper management, education, and well-being of OCA individuals with BCC but as this is not solely based on the skin, patients should also be referred to an ophthalmologist to monitor the patient’s ocular and visual abnormalities [1,2,4].
To our knowledge, this is the first reported case of basal cell carcinoma in a Filipino with oculocutaneous albinism as a risk factor. We hope that it expands our understanding of BCC in patients with OCA and encourages public health initiatives to focus more on education and prevention [2,5].
Case Presentation
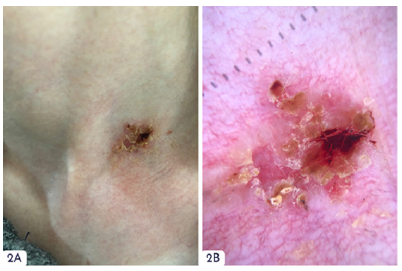
A 25-year-old Filipino female presented to our clinic with a keratotic plaque on the left side of the neck. The lesion first appeared 1 year prior to consult as a small erythematous papule that progressively grew into an erythematous plaque topped with hemorrhagic crusts. She had milky-white skin, silvery hair, and blue eyes at birth that gradually darkened with age associated with progressive photosensitivity, photophobia, and nystagmus. No family history of albinism nor consanguineous marriage was noted. Physical examination revealed a fair-skinned patient with marked nystagmus and decreased visual acuity. Her hair was brown, while her irises had a light gray tint (Figures 1A to 1C). Clinical and genetic counseling was done which led to the diagnosis of OCA 1B. Multiple benign nevi throughout the body were evaluated but upon dermoscopy of the erythematous keratotic plaque on the neck, telangiectasias, ulceration and yellow crusts were appreciated (Figures 2A and 2B).
Figure 1A to 1C: Pigmentary dilution of skin with tan hair and gray-tinted irises characteristic of oculocutaneous albinism 1B. She had nystagmus but not visible here. (Photos taken with patient’s consent)
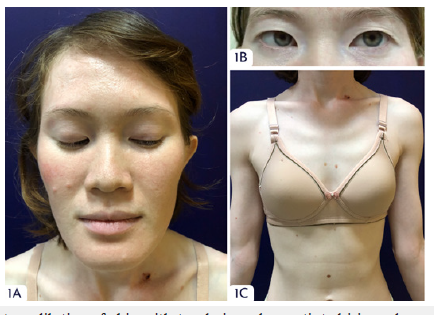
Figure 2A:Clinical image of basal cell carcinoma at the left side of the neck. 2B: On dermoscopy, telangiectasias, ulceration and yellow crusts were seen.
Biopsy was done on the lesion on the neck which showed tumor islands with atypical basaloid cells, peripheral palisading of tumor cells, and retraction artifacts in the epidermis with lymphocytic inflammatory stroma in the upper dermis diagnostic of nodular BCC (Figures 3A to 3C). She underwent stage I of Mohs micrographic surgery and was prescribed with cefalexin and mupirocin cream post procedure. Due to the increased risk of recurrence, she was recommended to follow-up regularly for screening and advised strict sun protection.
Figure 3:Histopathology from a keratotic plaque on the left side of the neck. A: Hematoxylin & Eosin (H&E) staining of basal cell carcinoma at 40×. B & C: H&E at 400×. Note tumor islands with atypical basal cells, peripheral palisading, and retraction artifacts diagnostic of nodular basal cell carcinoma.

Discussion
Oculocutaneous Albinism individuals have a 1000-fold risk for developing skin cancer with a well-established risk of recurrence than the general population due to the lack of melanin which is important against UV radiation and oxidative damage of DNA [2]. As such, the hypopigmented skin of this young OCA patient predisposed her to chronic and severe damage that led to the development of a malignant skin lesion. In a comparable study by Behera et al. (2017), our patient had features consistent with photodamage such as a malignant cutaneous tumor, affecting the photo-exposed area of the body with histopathology results consistent with basal cell carcinoma [3]. Although squamous cell carcinoma is the most common malignancy encountered in albinos, the occurrence of basal cell carcinoma cannot be ignored. Hence, close observation, regular follow-up, biopsy of the suspicious lesion, and the use of sun protection methods should be done at its earliest as skin cancer can be preventable in all patients, especially in those with albinism [3,6,7].
Acknowledgements
I would like to thank the following consultants at the East Avenue Medical Center, Department of Dermatology, Dr. Arunee Siripunvarapon, Dr. Elizabeth Prieto, and Dr. Ma. Angela Lavadia for their guidance and support.
Conflict of Interest
None
References
- Kang S, Amagai M, Bruckner AL, Enk AH, Margolis DJ, et al. (2018) Fitzpatrick’s dermatology in general medicine. In: (9th edn), McGraw-Hill Education, New York, United States, pp. 1310-1329.
- Ma EZ, Zhou AE, Hoegler KM, Khachemoune A (2022) Oculocutaneous albinism: epidemiology, genetics, skin manifestation, and psychosocial issues. Arch Dermatol Res.
- Behera D, Tripathy T, Kar B (2017) Multiple basal cell carcinoma in a patient of oculocutaneous albinism. Indian Dermatol Online J 8(2): 134-135.
- Chatterjee K, Rasool F, Chaudhuri A, Chatterjee G, Sehgal VN, et al. (2013) Basal cell carcinoma, oculo-cutaneous albinism and actinic keratosis in a native Indian. Indian J Dermatol 58(5): 377-379.
- Siauta JT, Windura CA, Putra LK (2022) Cutaneous and lip squamous cell carcinoma in an albinism patient: A case report. Annals of Medicine and Surgery 81: 104556.
- Zhang Q, Jin-Fa D, Yu HQ (2019) oculocutaneous albinism with squamous cell carcinoma, bowen's disease and actinic keratosis: A case report. International Journal of Dermatology and Venereology 2(2):103-105.
- Hassan S, Louis SJ, Fethiere M, Dure D, Rosen J, et al. (2022) The prevalence of nonmelanoma skin cancer in a population of patients with oculocutaneous albinism in Haiti. International Journal of Dermatology 61(7): 867-871.
© 2022 Marianne Isabel A Sayo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






