- Submissions

Full Text
Advancements in Case Studies
Septic Shock and Severe Acute Respiratory Distress Secondary to Covid-19 in Pediatric: A Case Report
Shirin Sarejloo1*, Mohammad Reza Hatamnejad2 and Arzhang Naseri2
1Medical doctor and cardiologist, Cardiovascular Research Center, Shiraz University of Medical Sciences, Iran
2Medical doctor, Member of Cardiovascular Research Center, Shiraz university of medical science, Iran
*Corresponding author: Shirin Sarejloo, Medical doctor and cardiologist, Cardiovascular Research Center, Shiraz University of Medical Sciences, Iran
Submission:July 11, 2022;Published: August 02, 2022

ISSN 2639-0531Volume3 Issue4
Abstract
Background: We report a patient who was a child and developed septic shock and severe acute
respiratory distress secondary to covid-19 infection to examine the cause of the changes and provide a
theoretical basis for shock management.
Case report: On April 9th, a 14-year-old Iranian boy, a known case of cerebral palsy and convulsion,
was admitted to a local hospital in a shocking state. On admission, his blood pressure was 88/54 mmHg,
respiratory rate was 32 breaths/min, pulse rate was 178 beats/min, body temperature was 39/5 c,
oxygen saturation was 66% but increased to 87% when she received 3-5liter oxygen from face mask;
physical examination showed intercostal retraction, decreased breathing sound in left side, delayed
capillary filling, cold extremities with a weak pulse. Acute resuscitation including dopamine 90mg in
50cc Dextrose 5%/water in 10 hours, endotracheal intubation, mechanical ventilation, and hydration
with 1700cc D/W 5% (77meq NaCl and 20meq KCl were added too) was done. A broad spectrum of
empirical antibiotic therapy was started. Testes showed WBC was higher than the reference interval,
lymphocyte count was lower than reference intervals, hemoglobin was lower than the reference interval
and platelets count was higher than the reference interval. Blood culture showed positive infectious of
staphylococcus aureus. Chest X-ray showed left side pleural effusion. HRCT showed increased vascularity
and peripheral basal part ground-glass opacification with a left side left lower lobe collapse. Throat
swabs tests were positive for covid-19 nucleic acid so a definitive diagnosis of covid-19 was concluded.
Hydroxychloroquine 200mg twice daily and Lopinavir/Ritonavir 300mg twice daily were started. After
resuscitation, his body temperature was 37.1c, Respiratory rate was 20 breaths/min with mechanical
intubation, Heart rate was 148 beats/min, Blood pressure was 98/75 mmHg and she was transferred to
the pediatric intensive care unit after stable condition.
Conclusion: We hypothesize, that air-blood barrier deficit due to covid-19 may lead to transmission of preexisting
pneumonia or other bacterial infection in respiratory tracts and causes bacterial sepsis. Further
study is needed. Treatment of septic shock requires hemodynamic support with the administration of
vasopressors, crystalloid solutions, broad-spectrum anti-biotic, antiviral treatment, high flow of oxygen
therapy, and mechanical intubation if the shock is accompanied by acute respiratory distress was helpful
for pediatric.
Keywords:Case report; Septic shock; Severe acute respiratory distress; Coronavirus disease 2019; Pediatric
Abbreviations:COVID-2019: Coronavirus Disease 2019; SARS-CoV-2: Severe Acute Respiratory Syndrome Coronavirus 2; D/W: Dextrose/Water; NaCl: Sodium Chloride; KCL: Potassium Chloride; HRCT: High Resolution Computed Tomography; ICU: Intensive Care Unit; Po2: Partial Pressure of Oxygen; Pco2: Partial Pressure of Carbon Dioxide; FIo2: Fraction of Inspired Oxygen; HCO3: Bicarbonate Blood Urea Nitrogen; ESR: Erythrocyte Sedimentation Rate; CRP: C Reactive Protein
Introduction
In December 2019, an outbreak of severe acute respiratory syndrome coronavirus 2 (SARSCoV- 2) infection occurred in Wuhan, Hubei Province, China, and spread across China and beyond [1,2]. The most common symptoms of patients include fever (98.6%), fatigue (69.6%), dry cough, and diarrhea [3]. Recent data reported from the Chinese Centers indicated that among the 44,672 confirmed cases of COVID-19 as of February 11, 2020, 416 (0.9%) were aged 0-10 years and 549 (1.2%) aged 10- 19 years [4-6]. The reported prevalence of shock in adult patients with COVID-19 is highly variable (from 1 to 35%), depending on the patient population studied, the severity of illness and the definition of shock. In a recent report summarizing the epidemiological characteristics of 44,415 Chinese patients with COVID-19, 2087 (5%) were diagnosed as critical cases, defined as severe hypoxemia and/or the presence of other organ failures, including shock. In another Chinese study of 1099 patients with COVID-19 with similar severity of illness, only 12 (1.1%) developed shock. In hospitalized patients, the incidence is likely higher and may reach 20-35% among patients in the ICU [7-11]. Although cases of severe acute respiratory syndrome coronavirus 2 in pediatrics were reported, there is no report of bacterial sepsis and severe acute respiratory distress due to covid-19 infection in pediatrics. In this paper, we report a patient who was a child and developed septic shock and severe acute respiratory distress secondary to covid-19 infection to examine the cause of the changes and provide a theoretical basis for shock management in pediatrics.
Case Presentation
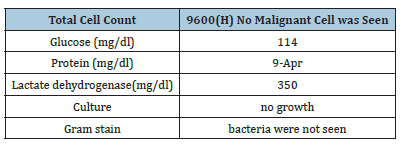
On April 9th, 2020, a 14-year-old Iranian boy with, a known case of cerebral palsy and convulsion, was admitted to a local hospital in a shocking state. The patient had no history of seafood consumption, travel out of the country, and recent hospital admission. Also, there was a negative history of covid-19 or any other viral infections in household members, so the source of infection was obscure. The patient was in his usual state of good health till 20 days before admission which developed into fever and dyspnea. His condition progressed gradually until April 9th when he presented with shock and respiratory distress. On admission, his blood pressure was 88/54mmHg, respiratory rate was 32 breaths/min, pulse rate was 178 beats/min, body temperature was 39/5c, oxygen saturation was 66% but increased to 87% when she received 3-5liter oxygen from face mask; physical examination showed intercostal retraction, decreased breathing sound in the left side and harsh breathing sound of the upper respiratory tract, delayed capillary filling, cold extremities with a weak pulse. Venous blood gas showed: ph:7/04, Po2 :45.2, Pco2:71.6, FI o2: 21%, HCO3: 19.5 mmol/l. Acute resuscitation includes dopamine 90mg in 50cc Dextrose 5%/water in 10 hours (slowly infusion), endotracheal intubation and mechanical ventilation with closed monitoring, and hydration with 1700cc D/W 5% (77meq NaCl and 20meqKCl were added too) had done him. After 40 minutes of resuscitation, body temperature was 37.1 ˚C, Respiratory rate was 20 breaths/ min with mechanical intubation, heart rate was 148 beat/min, blood pressure was 98/75mmHg and she was transferred to the pediatric intensive care unit. Symptoms and the worst vital signs according to the day of illness and day of hospitalization were shown in Table 1. In order to determine the cause of the shock state routine laboratory tests (complete blood count with differential, BUN, Creatinine, Na, K, blood Sugar, ESR, CRP) blood culture, Urine analysis, Urine culture, chest x-ray, High-Resolution CT scan, PCR of throat swabs for covid-19 was requested and also a broad spectrum of empirical anti-biotic therapy (meropenem 1200mg q8 hour and vancomycin 450mgq 6hour) was started. Testes showed that white blood count was higher than reference interval, lymphocyte count was lower than reference intervals, hemoglobin was lower than reference interval, platelets count was higher than reference interval, prothrombin time, partial thrombin time and international normalized ratio were higher than reference interval. Table 2 shows the laboratory test results during this period. Blood culture showed positive infectious of staphylococcus aureus. Chest X-ray showed severe left side pleural effusion with the shift of heart and mediastinum to the right side, superior rib notch, cervical rib, and scoliosis (Figure 1), then chest sonography and pleural fluid aspiration under sonographer’s guide were done and the sample was evaluated. Table 3 shows the pleural effusion laboratory tests. The chest tube was inserted for drainage pleural effusion then he underwent HRCT and showed significantly increased vascularity, peripheral basal part ground-glass opacification with a left side left lower lobe collapse, no vascular anomaly, and no aortic coarctation was seen. Left side pleural effusion was seen that wasn’t chylous (Figure 2) and his throat swabs tests were positive for covid-19 nucleic acid so a definitive diagnosis of covid-19 was concluded. Hydroxychloroquine 200mg twice daily and Lopinavir/Ritonavir 300mg twice daily were started. Unfortunately, next day patient developed respiratory distress and acute resuscitation was done otherwise it wasn’t effective so the patient died just 1 day after his admission.
Table 1: Symptoms and the worst vital signs according today of illness and day of hospitalization.
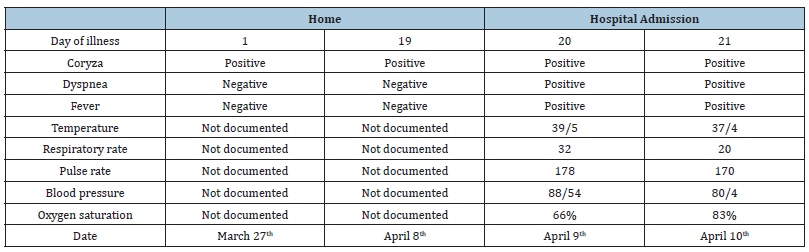
Table 2: clinical laboratory findings
[1] (H) shows higher than reference interval
[2] (L) shows lower than reference interval
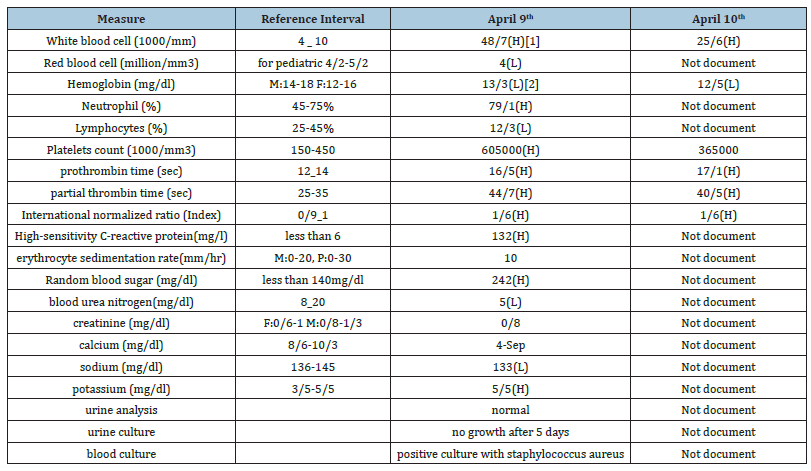
Figure 1CXR: The first image is chest x-ray image of the patient on April 9th which shows severe left side pleural effusion with shift of heart and mediastinum to right side, superior rib notch, cervical rib and scoliosis, retrospectively figure 1 shows the chest x-ray image on April 10th after chest tube insertion in 5th left intercostal space and 1200cc drainage.
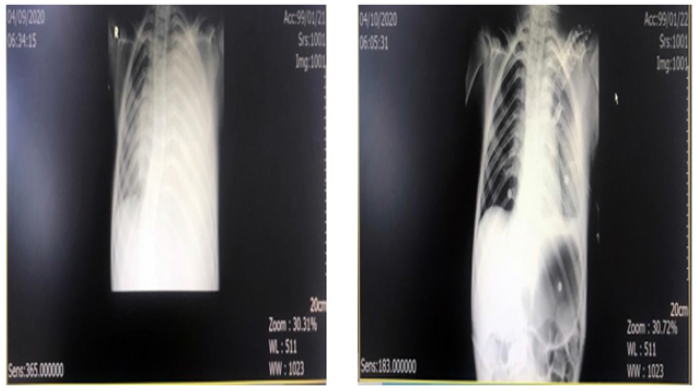
Figure 2HRTC: These are High resolutions computed tomography of patient on April 10th after chest tube insertion and drainage, which show significant increased vascularity, peripheral basal part ground glass opacification with left side left lower lobe collapse. No vascular anomaly and aortic co-architation is seen. Sever left side pleural effusion is seen that isn’t chillosis.
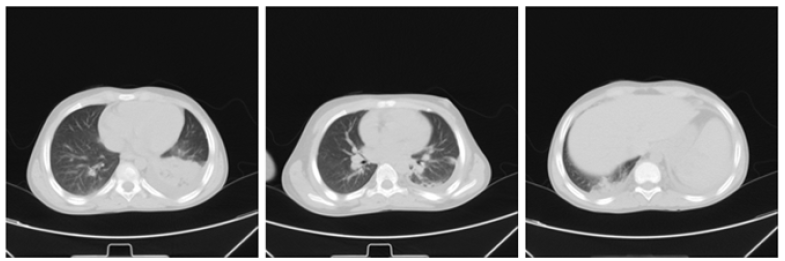
Table 3: pleural fluid analysis.
Discussion
So far, the majority of COVID-19 cases occurred in adults and particularly in older adults so the disease in children has been less well described and those who discussed covid-19 in pediatrics represent it with mild or moderate cases and almost there is a lack of death in children [12-14] so we reported a septic shock and respiratory distress due to coronavirus infection in pediatric in order to examine the cause of the changes and provide a theoretical basis for better management.
In a recent paper, a hypothesis had been announced that in severe or critical COVID-19 cases, the integrity of the epithelialendothelial (air-blood) barrier was severely interrupted. In addition to epithelial cells, SARS-CoV-2 can also attack lung capillary endothelial cells, which leads to a large amount of plasma component exudate in the alveolar cavity [15-17]. In response to the infection of SARS-CoV-2, alveolar macrophages or epithelial cells could produce various pro-inflammatory cytokines and chemokines. Upon this change, monocytes and neutrophils were then chemotactic to the infection site to clear these exudates with virus particles and infected cells, resulting in uncontrolled inflammation. In this process, because of the substantial reduction and dysfunction of lymphocytes, the adaptive immune response cannot be effectively initiated. The uncontrolled virus infection leads to more macrophage infiltration and a further worsening of lung injury [18]. Meanwhile, the direct attack on other organs by disseminated SARS-CoV-2, the immune pathogenesis caused by the systemic cytokine storm, and the microcirculation dysfunctions together lead to viral sepsis [19]. Theory can be supposed for bacterial sepsis; due to air-blood barrier deficit may lead to transmission of pre-existing pneumonia or other bacterial infection in respiratory tracts. Further study is needed to obtain a definite conclusion. A guideline for shock management secondary to covid-19 in adults has been published [3,7] but there isn’t such guideline for children.
Conclusion
According to our experience applying administration of vasopressors, crystalloid, a broad-spectrum antibiotic, antiviral treatment, high flow of oxygen therapy, and mechanical intubation if the shock is accompanied by acute respiratory distress (as the guideline said for an adult) was helpful in pediatric. Vital signs and oxygen saturation changed to the normal level, and capillary filling and skin turgor got normal. Further study is needed.
Declaration
Acknowledgments
We would like to thank the patient’s family for their participation and co-operation.
Authors’ contributions
Conception and design of the work: SS and MH. Clinical data collection: AN and MH. Imaging data collection and analysis: MH, and AN. Laboratory data collection and analysis: SS and AN. Drafting the article: MH and HB. Critical revision of the article: SS, MH, and AN. Agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: SS, MH, and AN. All authors read and approved the final manuscript.
Funding
No funding was received.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Ethical approval and consent to participate
This study was carried out in accordance with the recommendations of the Institutional ethics committee of the university of Shiraz with, ethic code: IR.SUMS.REC.1399.006. All subjects gave written informed consent in accordance with the Declaration of Helsinki. The protocol was approved by the Institutional ethics committee of Shiraz University of medical science, Iran.
Consent for publication
Written informed consent was obtained from the patient’s legal guardians for publication of this case report and any accompanying images. A copy of the written consent is available.
References
- Zu ZY, Jiang MD, Xu PP, Chen W, Ni QQ, et al. (2020) Coronavirus disease 2019 (COVID-19): A Perspective from China. Radiology 296(2): E15-E25.
- Abdolrahimzadeh Fard H, Mahmudi-Azer S, Sefidbakht S, Iranpour P, Bolandparvaz S, et al. (2021) Evaluation of chest CT scan as a screening and diagnostic tool in trauma patients with coronavirus disease 2019 (COVID-19): a cross-sectional study. Emerg Med Int 2021: 4188178.
- Hassan SA, Sheikh FN, Jamal S, Ezeh JK, Akhtar A (2020) Coronavirus (COVID-19): A review of clinical features, diagnosis, and treatment. Cureus 12(3): e7355.
- Lee PI, Hu YL, Chen PY, Huang YC, Hsueh PR (2020) Are children less susceptible to COVID-19? J Microbiol Immunol Infect 53(3): 371-372.
- Jahangiri S, Mousavi SH, Hatamnejad MR, Salimi M, Bazrafshan H (2022) Prevalence of non‐steroidal anti‐inflammatory drugs (NSAIDs) use in patients with hypertensive crisis. Health Sci Rep 5(1): e483.
- Shafiekhani M, Shahabinezhad F, Niknam T, Tara SA, Haem E, et al. (2021) Evaluation of the therapeutic regimen in COVID-19 in transplant patients: where do immunomodulatory and antivirals stand? Virology journal 18(1): 228.
- Alhazzani W, Møller MH, Arabi YM, Loeb M, Gong MN, et al. (2020) Surviving sepsis campaign: Guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Medicine 46(5): 854-887.
- Asadi-Pooya AA, Nabavizadeh SA, Sadeghian S, Shahisavandi M, Barzegar Z, et al. (2021) Psychological problems among patients with chronic medical disorders during the COVID-19 pandemic. Acta Medica Iranica 59(6): 322.
- Fard HA, Borazjani R, Sabetian G, Shayan Z, Parvaz SB, et al. (2021) Establishment of a novel triage system for SARS-CoV-2 among trauma victims in trauma centers with limited facilities. Trauma Surgery & Acute Care Open 6(1): e000726.
- Fard HA, Mahmudi-Azer S, Yaqoob QA, Sabetian G, Iranpour P, et al. (2022) Comparison of chest CT scan findings between COVID-19 and pulmonary contusion in trauma patients based on RSNA criteria: Established novel criteria for trauma victims. Chin J Traumatol 25(3): 170-176.
- Hatamnejad MR, Heydari AA, Salimi M, Jahangiri S, Bazrafshan M, et al. (2022) The utility of SYNTAX score predictability by electrocardiogram parameters in patients with unstable angina. BMC Cardiovascular Disorders 22(1): 8.
- Pearce N, Moirano G, Maule M, Kogevinas M, Rodo X, et al. (2020) Is death from Covid-19 a multistep process?.
- Mehrabi Z, Salimi M, Niknam K, Mohammadi F, Mamaghani HJ, et al. (2021) Sino-orbital mucormycosis associated with corticosteroid therapy in covid-19 infection. Case Rep Ophthalmol Med 2021: 9745701.
- Nematollahi MA, Askarinejad A, Asadollahi A, Salimi M, Moghadami M, et al. (2022) Association and predictive capability of body composition and diabetes mellitus using artificial intelligence: A cohort study.
- Nikoo MH, Mozaffari R, Hatamnejad MR, Bazrafshan M, Kasaei M, et al. (2021) Systolic dysfunction and complete heart block as complications of fulminant myocarditis in a recovered COVID-19 patient. Journal of Cardiology Cases 24(4): 177-181.
- Zibaeenezhad MJ, Sayadi M, Bazrafshan H, Daneshvar Z, Parsa N, et al. (2021) The prevalence of cardiovascular risk factors in fatal cases of COVID-19 in Fars Province, Iran. International Cardiovascular Research Journal 15(1).
- Moghimi N, Faridfar A, Jelodari Mamaghani H, Nikandish M, Shahriarirad R, et al. (2021) Evaluation of the relationship between vitamin D levels and related serum markers as well as disease activity in patients with rheumatoid arthritis: A cross-sectional study. Journal of Bioengineering Research 3(4): 1-9.
- Ranjbar S, Drissi HB (2020) Acute pulmonary embolism as an important differential diagnosis of COVID-19: A case report. Medical Case Reports 6(5): 156.
- Li H, Liu L, Zhang D, Xu J, Dai H, et al. (2020) SARS-CoV-2 and viral sepsis: observations and hypotheses. Lancet 395(10235): 1517-1520.
© 2022 Shirin Sarejloo. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






