- Submissions

Full Text
Advancements in Case Studies
Pneumomediastinum as a Rare Consequence of Breast Cancer Surgery
Sparavigna Marco1,2, Gipponi Marco1*, Franchelli Simonetta1, Atzori Giulia1, Cornacchia Chiara1, Diaz Raquel3, Murelli Federica1,3, Depaoli Francesca1, Friedman Daniele1,3 and Fregatti Piero1,3
1Breast Surgery Clinic, San Martino Policlinic Hospital, Italy
2Department of Internal Medicine, University of Genoa, Italy
3Department of Surgical Sciences and Integrated Diagnostic (DISC), School of Medicine, University of Genoa, Italy
*Corresponding author: Marco Gipponi, Breast Surgery Clinic, San Martino Polyclinic Hospital, Genoa, Italy
Submission:July 15, 2022;Published: July 25, 2022

ISSN 2639-0531Volume3 Issue3
Abstract
Occurrence of pneumomediastinum and subcutaneous emphysema during breast cancer surgery procedure is very rare. We report a case of a 73-year-old woman who developed pneumomediastinum and subcutaneous emphysema after breast conserving surgery and axillary lymph node dissection. Careful monitoring, immediate diagnosis and proper treatment are crucial for patient safety.
Keywords:Breast Conserving Surgery; Breast Cancer; Pneumomediastinum
Introduction
Surgical treatment of breast cancer has profoundly changed in the past years, breast conserving surgery being nowadays considered as the gold standard for most patients; it is a safe and cost-effective procedure, with a major decrease in hospital stay and postoperative complications [1]. The management of axillary lymph nodes has also evolved, with standard axillary lymph node dissection (ALND) being now replaced by sentinel lymph node biopsy (SLNB). Actually, ALND is performed only in selected patients with SLNB macrometastasis, representing a safe procedure but with some post-operative complication such as: lymphedema in approximately 30% of patients; numbness of arm; restriction of movement; pain, and infection [2-3]. Pneumomediastinum (PM) is a clinical entity characterized by the presence of air into the mediastinal cavity; it is a rare complication of non-thoracic surgery and, to the best of our knowledge, there are no reported case after breast surgery.
Case Report
Cutaneous ipsilateral breast cancer recurrence (IBCR) of invasive lobular carcinoma was detected into the right upper-outer quadrant of a 73-year-old female patient with no co-morbidity factors. She had been already treated for breast cancer two years before by means of right nipple-sparing mastectomy with SLNB and immediate breast reconstruction. She was scheduled for local excision and repeated SLNB and she had a more than acceptable anesthesiologic risk (ASAI); systemic disease was ruled out by means of total body computerized tomography (CT) and bone scan. The surgical procedure was accomplished through a single lateral incision; at intra-operative histology, a macrometastasis was detected into the SLNB so that immediate ALND was performed; the procedure was completed by single suction drainage positioning into the axilla. No adverse events occurred in the early post-operative hospitalization; the axillary drainage produced 50ml daily, and the patient was discharged without fever on the following day with the axillary drainage still in place with the recommendation of voiding the drainage every 24 hours, as it was carefully explained by a dedicated breast nurse.
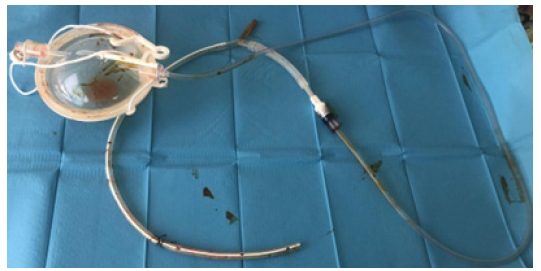
On the second post-operative day she was accepted at a peripheral hospital with acute chest pain and, after a first clinical evaluation, she was centralized at San Martino Policlinic Hospital with a differential diagnosis between PM or acute heart attack. At re-admission she referred an acute chest pain changing with breathing and rhinolalia; she had dyspnoea, 97% peripheral oxygen saturation, with no fever. Subcutaneous crepitus on upper right chest palpation was detected. COVID-19 test by means of nasopharyngeal swab was negative; high sensitivity troponin test was negative, as well. Chest CT with intravenous contrast medium was performed to rule out pulmonary embolism; diffuse subcutaneous emphysema into the upper right chest was detected (Figure 1) with concomitant PM (Figure 2) and the axillary drainage was still in place (Figure 3). After breast and thoracic surgeon evaluation no indication for surgery was proposed. The patient was admitted into the Pneumo- Clinic and she was given oxygen support and broad-spectrum antibiotic therapy.
Figure 1:Sub-cutaneous emphysema.
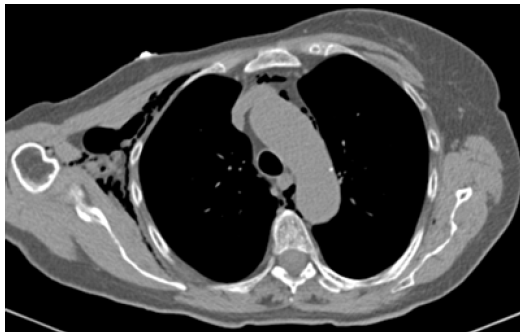
Figure 2: Pneumomediastinum.
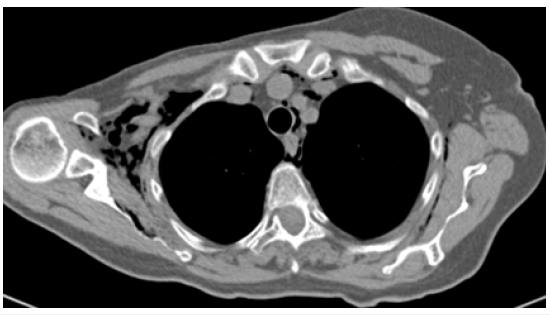
Figure 3:Drainage tube ( ).

On the third post-operative day the drainage was removed with an inspiration manoeuvre, its integrity was checked, and the exit site was closed with a transfixed point (Figure 4). A new chest radiography showed partial resolution of PM with no change in the subcutaneous emphysema. As soon as she had oxygen saturation of 99% in ambient air oxygen supplementation was stopped. On the fifth post-operative day a new chest radiography showed still persistence of subcutaneous emphysema, and on the seventh postoperative day she was discharged. At follow-up visits sub-cutaneous emphysema and rhinolalia were definitively solved, and no surgical site infection did occur.
Figure 4:DT after removal.
Discussion
PM is defined as the migration of air into the mediastinal space, and it may be classified as primary or spontaneous PM, or secondary PM related to external causes, such as: traumas, underlying pulmonary disease, or iatrogenic intervention including intubation, laparoscopic procedures, etc. [4-5]. Although PM is usually regarded as a relatively benign condition, sometimes it can lead to severe complication; so, tension PM is a critical situation that may lead to reduced cardiac output due either to direct cardiac compression (cardiac tamponade) or reduced venous return, as well as to airway compression [6].
PM following surgery may be regarded as a direct surgical complication or due to anaesthetic procedures following orotracheal intubation; this is most common in women, in patients with tracheal wall weakness, or protracted steroid therapy [7-8]. The mechanisms of injury are related to the use of oversized tubes, over inflation of cuff, sudden movements in the tube, vigorous attempts at intubation in emergency situations, or inappropriate use of the guide and repositioning of the tube without complete emptying of the cuff [9-10]. The clinical manifestations are represented by subcutaneous emphysema in the chest and neck; PM; pneumothorax and respiratory failure. The diagnosis is confirmed by means of CT-scan and fibreoptic bronchoscopy [11].
PM related to a surgical procedure has been very seldom reported, with only a few cases after laparoscopic surgery. In facts, the use of positive pressure gas to create the laparoscopic chamber can determine PM due to passage of gas through weak points or defects of the diaphragm. In these circumstances sub-cutaneous emphysema can be associated to PM itself or it is due to the detachment of the subcutaneous plane as a consequence of a misspositioning of Verres-needle [6-12].
To the best of our knowledge there are no reported cases of PM after breast surgery. Mammary emphysema is an uncommon manifestation of PM; in fact, the glandular tissue is separated from the retromammary space by the superficial fascia, in addition the deep pectoral fascia seals and it separates the pectoralis muscles [13]. Mammary emphysema due to breast surgery has been rarely reported and it is generally associated with local anaesthesia during aesthetic breast augmentation [13-14].
It’s not so easy to determine in our case report the exact mechanism of the air migration into the mediastinal space and in the subcutaneous tissue, although a peculiarity is represented by the fact that a silicon gel prosthesis had been positioned in the submuscular space at the former post-mastectomy reconstruction procedure, and this may have weakened local anatomy with an increased risk to barotraumas. On the other hand, anaesthetic manoeuvres can be easily ruled out because no difficulty during the intubation nor barotrauma during the ventilation of the patient were reported by the anaesthesiologist and most of all, no perforations of the tracheal-bronchial wall were detected at chest CT.
We could only speculate that PM was determined by an improper manoeuvre during the re-creation of the negative pressure after the reservoir was emptied. The use of closed suction drainage is a common practice aimed at reducing seroma formation; it is a routine manoeuvre that is generally not burdened by severe complications but, in this peculiar case, the specific anatomical conditions of the patient following previous reconstructive procedures may have predisposed to barotraumas [15-17].
Conclusion
PM is a very unusual complication after breast surgery; clinical monitoring and antibiotic therapy are fundamental in order to avoid serious life-threatening complications, such as mediastinitis and cardiac tamponade. Furthermore, the use of negative pressure drainage, although standardized, should be carried out with particular care and, in this context, great attention should be devoted to educating patients to prevent such, although rare, complications.
References
- Vitug AF, Newman LA (2007) Complications in breast surgery. Surg Clin North Am 87(2): 431-451.
- Hayes SC, Janda M, Cornish B, Battistutta D, Newman B (2008) Lymphedema after breast cancer: incidence, risk factors, and effect on upper body function. J Clin Oncol 26(21): 3536-3542.
- Warmuth MA, Bowen G, Prosnitz LR, Chu L, Broadwater G, et al. (1998) Complications of axillary lymph node dissection for carcinoma of the breast: a report based on a patient survey. Cancer 83(7): 1362-1368.
- Kouritas VK, Papagiannopoulos K, Lazaridis G, Baka S, Mpoukovinas I, et al. (2015) Pneumomediastinum. J Thorac Dis 7 (Suppl 1): 44-49.
- Kostis M, Patriarcheas V, Apergis S, Leontis M, Panayiotakopoulos G (2019) Isolated pneumomediastinum following laparoscopic cholecystectomy: a rare complication. J Surg Case Rep 20: rjz340.
- Mamić I, Danolić D, Puljiz M, Kasum M, Alvir I, et al. (2016) Pneumothorax and pneumomediastinum as a rare complication of laparoscopic surgery. Acta Clin Croat 55(3): 501-504.
- Medina CR, Camargo Jde J, Felicetti JC, Machuca TN, Gomes Bde M, et al. (2009) Post-intubation tracheal injury: report of three cases and literature review. J Bras Pneumol 35(8): 809-813.
- Borasio P, Ardissone F, Chiampo G (1997) Post-intubation tracheal rupture. A report on ten cases. Eur J Cardiothorac Surg 12(1): 98-100.
- Jougon J, Ballester M, Choukroun E, Dubrez J, Reboul G, et al. (2000) Conservative treatment for postintubation tracheobronchial rupture. Ann Thorac Surg 69(1): 216-220.
- Marty-Ané CH, Picard E, Jonquet O, Mary H (1995) Membranous tracheal rupture after endotracheal intubation. Ann Thorac Surg 60(5): 1367-1371.
- Schneider T, Storz K, Dienemann H, Hoffmann H (2007) Management of iatrogenic tracheobronchial injuries: a retrospective analysis of 29 cases. Ann Thorac Surg 83(6): 1960-1964.
- Kalhan SB, Reaney JA, Collins RL (1990) Pneumomediastinum and subcutaneous emphysema during laparoscopy. Cleve Clin J Med 57(7): 639-642.
- Franco T, Franco D, Treiger N (2007) Subcutaneous emphysema during breast augmentation: case report. Rev Bras Anestesiol 57(4): 414-420.
- Trignano E, Trignano C, Baccari M, Serra PL, Pili N, et al. (2021) Iatrogenic subcutaneous emphysema in aesthetic breast augmentation Medicolegal aspects. Ann Ital Chir 92: 131-134.
- Durai R, Ng PC (2010) Surgical vacuum drains: types, uses and complications. AORN J 91(2): 266-274.
- Chilson TR, Chan FD, Lonser RR, Wu TM, Aitken DR (1992) Seroma prevention after modified radical mastectomy. American Surgeon 58(12): 750-754.
- Grobmyer SR, Graham D, Brennan MF, Coit D (2002) High-pressure gradients generated by closed-suction surgical drainage systems. Surg Infect (Larchmt) 3(3): 245-249.
© 2022 Gipponi Marco. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






