- Submissions

Full Text
Advancements in Case Studies
Hypertensive Chorioretinopathy and Serous Retinal Detachment in Pre- Eclampsia
Brizido M1*, Almeida AC1, Silva PB2 and Basilio AL2
1Hospital Beatriz Ângelo, Loures, Portugal
2Central Lisbon University Hospital Center, Portugal
*Corresponding author: M Brizido, Department of Ophthalmology, Hospital Beatriz Ângelo, Portugal
Submission:July 06, 2022;Published: July 19, 2022

ISSN 2639-0531Volume3 Issue3
Abstract
Pre-eclampsia is defined as hypertension after 20 weeks of pregnancy associated with specific target organ damage. The disease may be associated with different visual complaints, starting before, during or after labour, which result from retinal, optical nerve or cortical complications. The presented report describes a case of blurred vision in a 24-year-old pregnant woman, whose visual complaints began three days before delivery. After being admitted to the hospital for high blood pressure and proteinuria at 38 weeks of gestation, a diagnose of pre-eclampsia was made and labour was induced. Evaluation at the Ophthalmology Department revealed multiple bilateral serous retinal detachments, associated with massive subretinal and intraretinal macular fluid. After proper control of high blood pressure, symptoms began to improve and patient’s visual acuity recovered, along with complete reabsorption of subretinal and intraretinal fluid. Pre-eclampsia is a serious medical condition with potential visual complications that requires prompt diagnosis and management. Timely recognition is crucial to prevent irreversible organ damage that might lead to neonatal or maternal death.
Keywords:Hypertensive chorioretinopathy; Pre-eclampsia; Pregnancy; Retinal detachment; Hypertension
Abbreviations:BCVA: Best corrected visual acuity; FA: Fluorescein angiography; ICGA: Indocyanine Green Angiography; OCT: Optical Coherence Tomography; RAPD: Relative Afferent Pupillary Defect; RPE: Retinal Pigment Epithelium
Introduction
Hypertension affects 5%-10% of all pregnancies worldwide, according to the International Society of Hypertension [1]. Pre-Eclampsia is defined as the presence of de novo hypertension after 20 weeks of gestation, accompanied by at least one of the following features: proteinuria, maternal organ dysfunction (liver, kidney or neurological impairment), hematological involvement (hemolysis or thrombocytopenia), and/or uteroplacental dysfunction, such as fetal growth restriction or abnormal Doppler ultrasound findings of uteroplacental blood flow [2]. The disease is estimated to affect 4.6% of pregnancies worldwide [3], being responsible for >500.000 fetal and neonatal deaths and >70.000 maternal deaths every year [2]. In some cases, it may only be recognized for the first time intrapartum or during the early postpartum period.
Pre-eclampsia is therefore a multisystemic disorder, frequently associated with a variety of visual changes, arising in approximately 25% of pre-eclamptic women [4]. Health care providers need to be aware that acute onset of visual symptoms in pregnant women can be the first sign of pre-eclampsia. Among the visual manifestations, blurring of vision and photopsia are very common complaints, but patients may also mention diplopia, amaurosis fugax, central or peripheral scotomas and complete blindness, in severe cases. These complaints most frequently result from serous retinal detachment, optic neuropathy secondary to ischemia, retinal vein occlusion, retinal or vitreous hemorrhages or cortical blindness [4-6].
Case Presentation
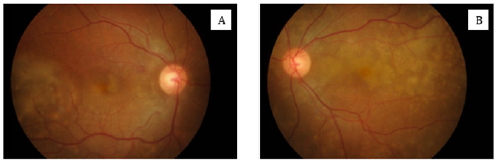
A 24-year-old Pakistani woman was referred to the ophthalmology emergency department one day after labour, for evaluation of bilateral blurred vision and decreased visual acuity starting four days earlier. She had been admitted to hospital at 38 weeks of pregnancy after presenting with high blood pressure (170/110mmHg) and proteinuria, for which a diagnosis of preeclampsia was made and labour was induced. The patient was a primigravida and had no relevant personal medical history. Ocular examination revealed a best-corrected visual acuity (BCVA) of 20/50 in both eyes. Pupils were isochoric and equally reactive to light and no relative afferent pupillary defect (RAPD) was detected. Intraocular pressure and anterior segment evaluation were unremarkable. Dilated fundus examination showed multiple bilateral serous retinal detachments affecting both the posterior pole and retinal peripheries (Figure 1). There were no associated haemorrhages, soft or hard exudates, disc oedema or vitritis.
Figure 1: Fundus photographs showing multiple areas of retinal pallor corresponding to areas of serous detachments involving the posterior pole of right (A) and left (B) eyes.
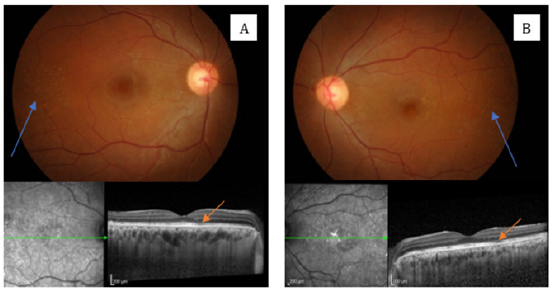
Fluorescein (FA) and indocyanine green angiography (ICGA) were remarkable for the presence of multiple hypo-fluorescent zones, presumably resulting from retinal and choroidal hypoperfusion (Figure 2). Optical coherence tomography (OCT) revealed the presence of subretinal and intraretinal fluid involving the macula (Figure 3). Following delivery, the patient persisted with high blood pressure, for which she was prescribed with nifedipine and captopril, resulting in a progressive improvement on blood pressure control. One week after labour, visual symptoms and visual acuity started to improve, and the patient was discharged, medicated with hypotensive therapy. One month later, she had nearly recovered from all visual deficits and, at the last follow-up (6 months after delivery) her BCVA improved to 20/25 on the right and 20/20 on the left eye, with only scarce areas or irregular retinal pigmentation noticeable (Figure 4).
Figure 2: FA (top pictures) and ICGA (bottom pictures) showing areas of retinal and choroidal hypoperfusion (arrows).
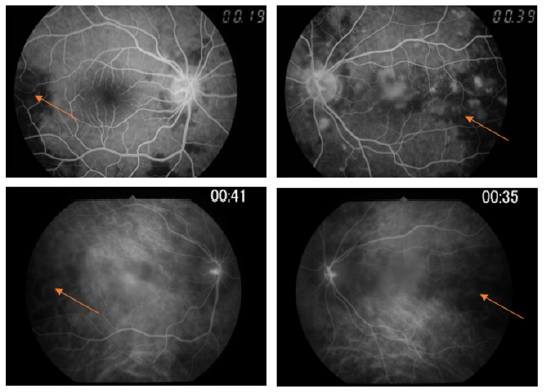
Figure 3: OCT images of the right (A) and left (B) eyes showing cystoid macular oedema with both intraretinal (orange arrows) and subretinal (blue arrows) fluid.
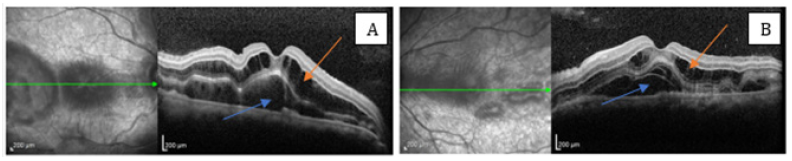
Figure 4:Fundus photographs and OCT images of the right (A) and left (B) eyes showing clusters of small hypopigmented lesions (blue arrows) and nearly imperceptible areas of attenuation of the ellipsoid zone (orange arrows).
Discussion
Pre-eclampsia is a multisystemic disorder resulting from generalized vasospasm and endothelial dysfunction [5]. Both retinal and choroidal circulations are affected, showing severe segmental or generalized constriction of arterioles [7]. Once choroidal vasculature is devoid of autoregulation and controlled by sympathetic nervous system, choroidal vessels are particularly susceptible to this type of insult, resulting in occlusion and necrosis of the microvasculature that compromises the retinal pigment epithelium (RPE) transport function, leading to serous retinal detachment [8].
Hypertension control remains the mainstay of treatment of pre-eclampsia, which normally requires induction of labour. Management of ophthalmic complications associated with preeclampsia is conservative and involves treating the underlying condition [5,8]. In general, prognosis is good, with gradual reabsorption of subretinal and intraretinal fluid once adequate blood pressure control is achieved. Visual acuity progressively improves during weeks following the crisis [4,5] usually recovering to pre-detachment levels. If extreme necrosis of the RPE or massive serous retinal detachment occurs, irreversible damage may arise, which makes early detection crucial to prevent permanent complications [7,9].
Conclusion
Pre-eclampsia may be responsible for serious ocular complications, if not promptly diagnosed and immediately treated. This case illustrates a successfully managed case of bilateral retinal detachment, reflecting the relevance of a multidisciplinary approach in similar cases.
References
- Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, et al. (2020) 2020 International society of hypertension global hypertension practice guidelines. Hypertension 75(6): 1334-1357.
- Brown MA, Magee LA, Kenny LC, Karumanchi SA, McCarthy FP, et al. (2018) Hypertensive disorders of pregnancy: isshp classification, diagnosis, and management recommendations for international practice. Hypertension 72(1): 24-43.
- Abalos E, Cuesta C, Grosso AL, Chou D, Say L (2013) Global and regional estimates of preeclampsia and eclampsia: a systematic review. Eur J Obstet Gynecol Reprod Biol 170(1): 1-7.
- Roos NM, Wiegman MJ, Jansonius NM, Zeeman GG (2012) Visual disturbances in (pre)eclampsia. Obstet Gynecol Surv 67(4): 242-250.
- Radha Bai Prabhu T (2017) Serious visual (ocular) complications in pre-eclampsia and eclampsia. J Obstet Gynaecol India 67(5): 343-348.
- Ghavidel L, Mousavi F, Bagheri M, Asghari S (2018) Preeclampsia induced ocular change. International Journal of Women's Health and Reproduction Sciences 6: 123-126.
- Raposo J, Melo B, Maciel N, Leite SD, Rebelo Ó RC, et al. (2020) Serous retinal detachment in pre-eclampsia: Case report and literature review. Rev Bras Ginecol Obstet 42(11): 772-773.
- Jayaraj S, Samanta R, Puthalath AS, Subramanian K (2020) Pre-eclampsia associated bilateral serous retinal detachment. BMJ case reports 13(9).
- Inan S, Polat O, Cetinkaya E, Inan UU (2019) Bilateral serous retinal detachment accompanied by a rare intraretinal fluid configuration in preeclampsia and PRES Syndrome. Rom J Ophthalmol 63(1): 86-90.
© 2022 Brizido M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






