- Submissions

Full Text
Advancements in Case Studies
Worsening of Previous Vasospasm after Sertraline Ingestion: A Reversible Cerebral Vasoconstriction Syndrome Spectrum?
Carvalho BM1*, Baeta AM1, Silva MA1, Ferreira WSM1, Bentes RGL1, Salzedas HT1, Campos CMS2, Baccin CE3, Abicalaf RS3 and Chaddad Neto FE4
1Department of Neurology, Brazil
2Department of Neuroradiology, Brazil
3Department of Neuro intervention, Brazil
4Department of Neurosurgery, Brazil
*Corresponding author: Carvalho BM, Department of Neurology, The Portuguese Charity Hospital of São Paulo, São Paulo, Brazil
Submission:December 7, 2021;Published: December 22, 2021

ISSN 2639-0531Volume3 Issue2
Abstract
Reversible cerebral vasoconstriction syndrome is an important vascular disease. It is characterized by diffuse segmental constriction of cerebral arteries. It has different etiologies, including medications. We present a case report of a young, previously asymptomatic patient; with a mild vasospasm secondary to a resection of a sphenoid frontotemporal meningioma that had a stroke-like episode following sertraline ingestion due to the potential worsening of a previous vasospasm. Correlating it with a possible spectrum of reversible cerebral vasoconstriction syndrome, it was successfully treated with intra-arterial and intravenous Milrinone and oral Verapamil.
Keywords: Reversible cerebral vasoconstriction syndrome; selective serotonin reuptake inhibitors; Tumor resection
Introduction
Reversible cerebral vasoconstriction syndrome (RCVS), or Call-Fleming syndrome, is a rare entity of multifactorial etiology characterized by the narrowing of multiple cerebral arteries, presenting clinically in patients with sudden headache, seizures and sometimes neurological deficits [1,2]. The pathophysiological mechanism has not yet been fully elucidated and the possible factors involved in its genesis include the increase in oxidative stress, endothelial dysfunction, transient failure of regulation of cerebral arterial tone in the face of sympathetic hyperactivity, genetic predisposition, among others [3].
Triggers are identified in approximately 50% of cases and time between exposure and development of RCVS can be from few days to months, which is a diagnostic challenge, given its low incidence and numerous associated factors. Among the possible causes are neurosurgery, hypertensive encephalopathy, pregnancy and some vasoactive drugs. The increasing use of antidepressant drugs, nasal decongestants and triptans, and illicit drugs, including amphetamines, cocaine, ecstasy and cannabis has resulted in significant increase in the number of cases [4].
We present a case report of a young patient, previously asymptomatic; with a mild vasospasm secondary to a sphenoidal frontotemporal meningioma resection that had a stroke-like episode after ingest 150mg of Sertraline due to potential worsening of the previous vasospasm. Correlating it as a possible spectrum of reversible cerebral vasoconstriction syndrome, it was successfully treated with intra-arterial and intravenous Milrinone and oral Verapamil.
Case Report
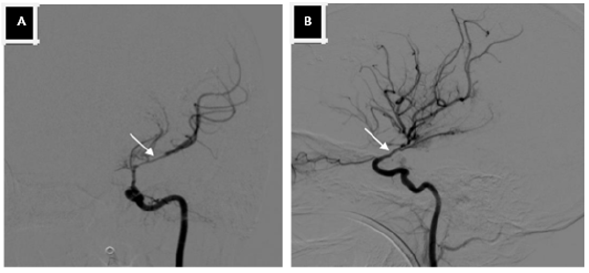
A 23-year-old female patient admitted to the emergency department with previous anxiety disorder under irregular medical follow-up ingested about 150mg of Sertraline, evolving after six hours with obnubilation, global aphasia and right complete hemiparesis (NIHSS Score 15). Twelve days before, she underwent a frontotemporal- sphenoidal meningioma resection which provoked a mild vasoconstriction of the left M1 segment, inferior brunch of M2 segment and cerebral anterior artery, with no clinical deficits (Figure 1). A brain computer tomography was performed under a stroke clinical suspicion revealed a cortical-sub cortical hypodensity in the parasagittal segment of the left frontal lobe projecting itself to the ipsilateral cingulate gyrus, superior frontal gyrus and corpus callosum associated with a narrowing in distal intern carotid artery and in M1 segment of the meddle cerebral artery, showing a much worse scenario compared to previous vascular study..
Figure 1:(A)Magnetic resonance FLAIR image of frontotemporal- sphenoidal meningioma. (B)Digital angiographic of previous mild vasoconstriction of left supraclinoidal internal carotid artery.

Suspecting vascular etiology, she underwent a digital angiographic study which showed displacement and vessel narrowing of the left middle cerebral artery and supraclinoid branch of the internal carotid artery caused by tumor mass effect. Its vascular supply comes from small branches of the internal carotid artery meningohypophyseal and inferolateral trunk as well from the ipsilateral external carotid and ophthalmic arteries (Figure 2). The vasospasm of the left supraclinoid internal carotid artery and M1 segment of the left middle cerebral artery was treated through a right femoral puncture with a 5Fr sheath (Terumo) and selective injection of 6mg of Milrinone in the left internal carotid artery and 4mg in the right internal carotid artery using a 5Fr diagnostic catheter (Cordis).
Figure 2:Digital angiographic. (A) Vasospasm of the left supra-clinoidal internal carotid artery before treatment with Milrinone. (B) During treatment with Milrinone.
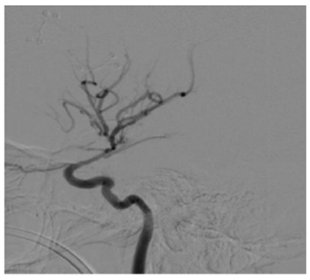
There was significant flow and caliber improvement of previously compromised arteries (Figure 3). Immediately after the procedure, the patient has progressively recovered her language and members movement and has been transferred to the intensive care unit where she has received complementary treatment with 20mg intravenous Milrinone in decreasing doses and 80mg of Verapamil orally three times a day. She has been discharged on the sixteenth day of hospitalization, with no neurological deficits (NIHSS score=0) and a prescription of oral Verapamil 240mg/day for 12 weeks.
Figure 3:Digital angiographic. Vasospasm of the left supra clinoidal internal carotid artery after treatment with Milrinone.
Discussion
Reversible cerebral vasoconstriction syndrome (RCVS) or Call-Fleming syndrome has a poorly known etiology and has been associated to multiple etiological factors. It was first described in 1988 in patients who presented with reversible segmental cerebral vasoconstriction, acute headache with or without focal neurological deficits and convulsions. It is predominant in patients with an average age of 45 years and higher incidence in females, with no prevalence in different ethnic groups. Focal neurological symptoms may or may not be present in 9 to 63% of cases, with brain edema, stroke, seizure or subarachnoid hemorrhage characterizing the most severe condition [1,2].
RCVS can occur spontaneously or secondary to causes that are most often identifiable, such as migraines, complications due to neurological surgeries, hypertensive encephalopathy, pregnancy and exposure to medications, with SSRIs being well described [2]. The cerebral vasospasm is a uncommon complication after intracranial tumors resection but still carries high mortality index. It occurs mostly in young patients probably due to cerebral vasoconstrictors hypersensitivity, exacerbating the vascular stress induced by surgery. Besides the age, other factors like local, vessel manipulation, vascular tonus and hypothalamic dysfunctions may increase the vasospasm risk [4]. In this case report, the patient has two important risk factors for the occurrence of the complication, the use of a drug that stimulates cerebral vasoconstriction and previous brain surgery.
Usually, vasoconstriction occurs in one week after neurosurgery [4]. In our patient case, the symptoms began at twelfth postoperative day, after took serotoninergic pills, resembling Call-Fleming syndrome. Patients with reversible cerebral arterial narrowing have almost identical clinical, laboratory, imaging and prognostic characteristics, regardless of the associated condition. The finding of greatest sensitivity for the diagnosis (100%) is the presence of diffuse vasoconstriction in cerebral arteries in cerebral angiography [1,5,6]. It is important to highlight that in our case, cerebral angiography showed that there was no generalized vasospasm, but worsening of previous vasospasm secondary to surgical manipulation and high levels of serotonin exposure, which narrowed the vascular lumen and caused transient ischemia to its irrigated supplied structures [4,7].
Regarding treatment, there are no specific guidelines for these cases and management is based on observational data and expert opinions. Since 2001, Milrinone, a potent vasodilator drug with a positive inotropic effect for inhibiting phosphodiesterase, has been consolidated mainly in case reports, as a useful drug in situations of cerebral vasoconstriction syndrome [8,9]. In our case, the patient had significant benefits and excellent response to intraarterial Milrinone, with immediate reversal of vasoconstriction and progressive clinical improvement initiated at the time of drug’s administration. As maintenance treatment, we used Verapamil and Milrinone intravenously until complete resolution of symptoms [10,11].
Conclusion
Showing in this case report a possible spectrum of reversible cerebral vasoconstriction syndrome induced by high doses of Sertraline since there was no generalized cerebral vasoconstriction but worsening of previous vasospasm secondary to surgical manipulation, later reversible with Milrinone and Verapamil. The morbidity and mortality of a cerebral vasospasm after tumor resection remains high and it constitutes a real challenge for current neurological practice.
Even in the late postoperative period, an important approach is to avoid the use of serotonergic drugs, even in low doses, in addition to advising caution with any triggering factors to avoid future complications. Further studies are still needed to evaluate the correct approach of these cases, but in our experience the administration of intra-arterial Milrinone was effective and safe, demonstrating a dramatic clinical improvement, without relevant side effects. Therefore, we believe that Milrinone could potentially become a beneficial choice on front lines for treatment of cerebral vasospasm, especially in the critical patients.
References
- Singhal A (2021) UPTODATE: Reversible cerebral vasoconstriction syndrome.
- Mehdi A, Hajj-Ali RA (2014) Reversible cerebral vasoconstriction syndrome: a comprehensive update. Curr Pain Headache Rep 18 (9): 443.
- Oliveira ML, Azevedo MK, Machado MF, Teixeira MJ, Shu ES (2016) The role of metabolism in the ischemia associated with vasospasm following brain tumor resection. Journal of Neuro Interventional Surgery 8(1): e17- e19.
- Alotaibi N, Giuseppe Lanzino G (2013) Cerebral vasospasm following tumor resection. J Neurointerv Surg 5(5): 413-418. doi:10.1136/neurintsurg-2012-010477.
- Ducros A (2012) Reversible cerebral vasoconstriction syndrome. Lancet Neurol 11(10): 906-917.
- Marder CP, Donohue MM, Weinstein JR, Fink KR (2012) Multimodal image of reversible cerebral vasoconstriction syndrome: a series of 6 cases. AJNR Am J Neuroradiol 33(7): 1403-1410.
- Cappelen-Smith C, Calic Z, Cordato D (2017) Reversible cerebral vasoconstriction syndrome: Recognition and treatment. Curr Treat Options Neurol 19(6): 21.
- Santos-Teles AG, Ramalho C, Rosa Ramos JG, Passos RH, Gobatto A, et al. (2020) Efficacy and safety of milrinone in the treatment of cerebral vasospasm after subarachnoid hemorrhage: a systematic review. Rev Bras Ter Intensiva 32(4): 592-602.
- Arakawa Y, Kikuta K, Hojo M, Goto Y, Ishii A, et al. (2001) Milrinone for the treatment of cerebral vasospasm after subarachnoid hemorrhage: report of seven cases. Neurosurgery 48(4): 723-728.
- Singhal AB, Hajj-Ali RA, Topcuoglu MA, Fok J, Bena J, et al. (2011) Reversible cerebral vasoconstriction syndromes: analysis of 139cases. Arch Neurol 68(8): 1005-1012.
- Robert T, Kawkabani Marchini A, Oumarou G, Uske A (2013) Identification of reversible cerebral vasoconstriction syndrome of prognostic factors. Clin Neurol Neurosurg 115 (11): 2351-2357.
© 2021 Carvalho BM. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






