- Submissions

Full Text
Advancements in Case Studies
Mucormycosis and Aspergillosis have been Linked to Covid-19-Related Fungal Infections in India
Chittaranjan Baruah1*, Papari Devi2, Bhabesh Deka3 and Dhirendra K Sharma4
1Postgraduate Department of Zoology, Darrang College, India
2TCRP Foundation, Guwahati, India
3North Bengal Regional Research and Development Centre, West Bengal, India
4School of Biological Sciences, University of Science and Technology, Meghalaya, India
*Corresponding author: Chittaranjan Baruah, Postgraduate Department of Zoology, Darrang College, India, E-mail: chittaranjan_21@yahoo.co.in
Submission:May 25, 2021;Published: June 04, 2021

ISSN 2639-0531Volume3 Issue1
Abstract
Mucormycosis and aspergillosis have been recorded in alarmingly high numbers in India in recent decades. Even though fungal infections contribute significantly to human morbidity and mortality, the effect of these diseases on COVID-19 patients is unknown. Mucormycosis and aspergillosis were identified as two post-acute symptoms in COVID-19 patients in this study. Coronavirus 2 of the severe acute respiratory syndrome causes direct damage to the airway epithelium, allowing Mucormycosis and aspergillosis to invade. There were 8,848 infected and 219 dead cases of COVID-19-associated mucormycosis in India as of May 22, 2021. In addition, four Aspergillosis patients have been registered in Bihar, India. In India, a COVID-19-related yellow fungus case was also recorded for the first time. Both mild and moderate-tosevere illness tend to be affected by the syndrome. Despite the urgent need for efficient diagnostic tests, as well as safe and effective new drugs and vaccines, research into the pathophysiology of human fungal infections lags behind that of other pathogen-related diseases.
Keywords: Aspergillosis; Black fungus; Candidiasis; COVID-19; Mucormycosis; SARS-CoV-2; White fungus
Introduction
Infections like mucormycosis, candidiasis, and aspergillosis have become more prevalent
in intensive care units and patients who have recovered from Covid. The total number of
coronavirus disease 2019 (COVID-19) cases in India has now reached 2,62,89,290, with
29,23,400 active cases and 2,95,525 deaths (22 May 2021). Amid the rising number of
Covid cases, India is dealing with a Black Fungus outbreak (mucormycosis). Even though
mucormycosis (MCR) is becoming more common in COVID-19 patients, the epidemiological
causes, presentation, diagnostic certainty, and outcome of these patients are not well
understood [1].
Concerns have also been raised regarding COVID-19-associated pulmonary aspergillosis
worsening the disease course and confirmed mortality. Just when the government was
coping with the mucormycosis outbreak, a new fungal infection, White Fungus infection
(Aspergillosis), began to spread. Azole-resistant Aspergillus caused the first case of COVID-
19-associated pulmonary aspergillosis. Aspergillosis is a fungal infection that affects many
parts of the body and spreads to the lungs. It also has serious consequences for the kidneys,
mouth, skin, and brain. Infections like mucormycosis, candidiasis, and aspergillosis have
become more prevalent in intensive care units and patients who have recovered from Covid.
As a result, the current article focused on case reports of mucormycosis and Aspergillosis in
India, as well as infections linked to COVID-19.
Mucormycosis may affect the lungs, but the nose and sinuses are the most common sites
of infection for mucormycosis. It can then spread to the eyes, causing blindness, or to the brain, causing headaches or seizures [2]. Mucormycosis can spread
to the eyes and cause blindness, or it can spread to the brain and
cause headaches or seizures. Mucormycosis infections occur when
a person meets fungal spores in the atmosphere, and Covid-19
patients taking immunosuppressive drugs such as steroids are
more susceptible to infection. While there is currently no official
national count of COVID-19 related mucormycosis infections,
all confirmed and suspected cases must now be reported to the
national health ministry.
Infection, Symptoms, and Treatment
Mucormycosis, formerly known as zygomycosis, is a fungal
disease caused by a variety of fungi in the Mucorales family.
Rhizopus oryzae is the most common member of this family to
cause infections in humans. Since inhaling fungal spores from the
air, it most often affects the sinuses or lungs. It may also happen
because of a cut, a burn, or some form of skin injury. Facial
deformity, fever, facial pain, nasal congestion, loss of vision or pain
in the eyes, altered mental state, confusion, swelling in the cheeks
and eyes, toothache, loosening of teeth, and black crusts in the nose
are all symptoms of Mucormycosis. While rhinocerebral (sinus
and brain), pulmonary (lung), Cutaneous (skin) mucormycosis,
and gastrointestinal mucormycosis are the most common types
of mucormycosis, disseminated mucormycosis typically occurs in
people who are already sick from other medical conditions like
COVID-19, making it difficult to determine which symptoms are
linked to mucormycosis. Patients with a disseminated infection
in the brain can experience changes in mental status or fall into a
coma [3].
Mucormycosis is a severe infection that requires antifungal
medication, such as amphotericin B, posaconazole, or isavuconazole
(CDC, www.cdc.gov). Patients can require antifungal medication
for up to six weeks to recover. Their prognosis is contingent on
how quickly the disease was identified and treated. Surgery is
often required to remove dead or contaminated tissue. This can
lead to the loss of the upper jaw or even the eye in some patients.
Aspergillosis is a fungal infection caused by Aspergillus, a common
mold (fungus) that can be found both indoors and out. Most
people will inhale Aspergillus spores without being ill. People
with compromised immune systems or lung disorders, on the
other hand, are more likely to develop health problems because
of Aspergillus. Aspergillus fumigatus, one of the causative agents
of Aspergillosis, is a saprotrophic fungus that lives mainly in soil
and is well-adapted to thrive in harsh conditions. This ability has
allowed the fungus to withstand and survive human host defense,
as well as to cause one of the most lethal lung infections in terms of
morbidity and mortality [4].
Aspergillus can cause allergic reactions, lung infections, and
infections in other organs, among other things. White fungus can
affect not only the lungs but also the “nails, skin, stomach, kidney,
brain, private parts, and mouth,” according to the CDC. After testing
negative for the virus, people with Aspergillosis are said to have
symptoms like Covid if the infection enters the lungs. A CT scan
or an X-ray may be used to diagnose the infection. While allergic
bronchopulmonary aspergillosis (ABPA), allergic Aspergillus
sinusitis, aspergilloma, and chronic pulmonary aspergillosis are
the most common forms of mucormycosis, invasive aspergillosis
is more common in people who are already sick from other
medical conditions such as COVID-19 [5]. From the lungs, however,
Aspergillosis cannot spread between people or between people and
animals. Itraconazole (for Allergic aspergillosis) and Voriconazole
(for Invasive aspergillosis) are the most common antifungal
medications used to treat aspergillosis (CDC, www.cdc.gov).
Case Studies
Indian Mucormycosis statistics and COVID-19-related reports: Mucormycosis is a life-threatening infection that affects many people. An analysis of published mucormycosis cases discovered a 54 percent all-cause mortality rate, with some cases only being saved by removing an eye [6]. The mortality rate differed depending on the underlying patient condition, fungus type, and affected body location. Sinus infections were associated with a 46% mortality rate, pulmonary infections with a 76% mortality rate, and disseminated mucormycosis with a 96% mortality rate [6]. Table 1 shows the clinical types of mucormycosis recorded in India between 2001 and 2020.
Table 1: Clinical types of mucormycosis that have been recorded in India, as well as the maximum mortality rate (during the period of 2001-2020).
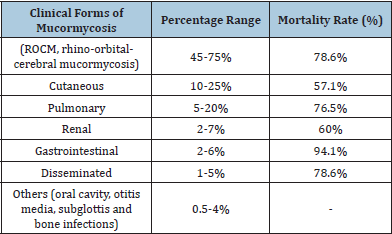
Source: Prakash and Chakrabarti [7]
In a previous study from March 2021, a total of 41 cases of
Covid-19-associated mucormycosis were recorded worldwide, with
70% of them in India [7]. According to recent studies, the number
of cases has risen dramatically, which is unsurprising considering
the ongoing Covid-19 outbreak in India. In a rising outbreak of the
disease, India has recorded 8,848 cases of deadly “black fungus”
(as of May 22, 2021). (The Tribune, 23 May 2021). Gujarat had
the most cases (2281) followed by Maharashtra (2,000), Andhra
Pradesh (910), Madhya Pradesh (720), Rajasthan (700), Karnataka
(500), Haryana (250), Delhi (197), Punjab (95), Chhattisgarh (87),
Bihar (56), Tamil Nadu (40), Kerala (36), Jharkhand (27), Odisha
(15), Goa (12), and Chandigarh (12) [8]. Four Indian doctors looked
at more than 100 cases of Covid-19 patients who had developed
mucormycosis in a separate report. It was discovered that 79 of
them were men, and 83 of them had diabetes. In a survey of 45 black
fungus patients in two Mumbai hospitals, it was discovered that all of them were diabetics or had been diagnosed with diabetes prior
to admission. Their blood sugar levels were both extremely high.
Within 10 days of being admitted to a medical facility for Covid-19
care, up to 30% of patients developed mucormycosis, according to
the report.
According to the CNN News reported situation, a woman from
India’s southern Telangana state, her father was diagnosed with
black fungus on April 26, the same day he recovered from Covid-19.
When he started to feel better, his face began to swell (from Covid).
Doctors recommended her to have an Amphotericin B injection
when the swelling did not go down. She had to apply to the state’s
chief minister for vials of the drug because the hospital did not
have any. Once the medicine was secured, her father underwent an
endoscopic sinus surgery to relieve the swelling.
COVID-19-related Indian Aspergillosis statistics: A recent
research from India found a higher prevalence of Aspergillus
sensitization (39.5%) and allergic bronchopulmonary aspergillosis
(ABPA) in 564 asthma patients (27 percent). According to Nath
et al. [8], the prevalence of Aspergillus hypersensitivity (AH) and
ABPA was 35.1 percent and 21.7 percent, respectively, in a study
of 350 patients. The disease is becoming more well-known, with
prevalence rates for ABPA ranging from 5.9% to 20.5 percent and
38 percent to 43 percent for Aspergillus hypersensitivity (AH) in
recent studies [9]. In this part of the world, there are few data on
prevalence. At the Patna Medical College Hospital (PMCH) in India,
four cases of white fungus linked to coronavirus were discovered.
The first yellow fungus case linked to COVID-19: A 45-yearold
patient in Ghaziabad, Uttar Pradesh, was found infected with
yellow fungus amid an increase in cases of Black Fungus infection
in several Indian states, as well as white fungus cases. Yellow
fungus, which causes superficial and deep mycoses in pets, captive,
and wild animals, especially reptiles, is more dangerous than both
Black and White fungi. The yellow fungus is a contagious fungus
that affects mostly reptiles. The infected patient is currently being
treated in a Ghaziabad, India hospital. Laziness, lack of appetite, or
no appetite at all, and weight loss are all symptoms of yellow fungus.
Yellow fungus may also cause pus leakage and slow wound healing,
starvation and organ failure, and sunken eyes due to necrosis in
severe cases.
CANV, yellow fungus (Chrysosporium anamorph of
Nannizziopsis vriesii). Infection with the virus known as CANV had
previously been identified in humans, often in immunocompromised
patients [10]. However, the recent molecular characterization work
has revealed these cases to be caused by species of Nannizziopsis
that are distinct from those found in reptiles. The possibility of
zoonotic transmission of O. ophiodiicola, Nannizziopsis spp., and
Paranannizziopsis spp. from reptiles to humans is low, although it
is possible in immunocompromised patients [10].
High prevalence of fungal infections among Indian COVID-19 patients
Humans may contract mucormycosis by inhaling spores,
swallowing spores in food or medications, or having spores
contaminate wounds. We inhale the spores of several fungi every
day. Our immune systems and lungs, on the other hand, are less
likely to cause infection if they are in good condition [4]. Mucorales
fungi are opportunistic, infecting people with a compromised
immune system or damaged tissue [6]. Use of drugs which suppress
the immune system such as corticosteroids can lead to impaired
immune function, as can a range of other immunocompromising
conditions.
Covid-19 drugs can deplete the body’s strength and immunity.
They may also cause non-diabetic Covid-19 patients’ blood sugar
levels to rise. Many cases of this unusual fungal infection have
been discovered in Covid patients, as well as diabetics, people
with kidney or heart issues, and people on high steroids. Patients
can develop fungal superinfection because of the virus’s extreme
immunomodulation and lymphocyte depletion, as well as the
subsequent administration of immune-system-targeting drugs.
These spores can develop in our airways or sinuses and enter our
bodies’ tissues when our lungs are weakened and our immune
systems are suppressed, as is the case in patients being treated for
extreme Covid-19. White fungus, which affects the lungs and causes
symptoms like coronavirus, is more common in COVID-19 patients.
COVID patients are susceptible to Mucormycosis and Aspergillosis
due to a lack of immunity caused by one or more of the following
factors.
A. using anabolic steroids for an extended period
B. admitted to the intensive care unit
C. on supplemental oxygen or a ventilator
D. spent a long time in the hospital
E. had to deal with unsanitary conditions in the hospital
F. whether there are comorbidities
G. take COVID19 and other medications at the same time
H. suffer from diabetes and obesity
I. suffer from kidney or heart disease
J. COVID19 causes Pneumonia in the lungs.
K. a lack of immunity
Steroids, which are used to save the lives of critically ill patients,
are thought to be the cause of mucormycosis and aspergillosis,
according to doctors. Steroids tend to help prevent some of the
damage that can occur when the body’s immune system goes into
overdrive to combat the coronavirus by reducing inflammation in
the lungs. However, in both diabetic and non-diabetic Covid-19
patients, they lower immunity and raise blood sugar levels. This
loss of immunity is thought to be the cause of the mucormycosis
outbreaks. According to India’s official National Health Portal,
diabetes affects 12 percent to 18 percent of the adult population,
with the incidence being highest in urban areas. COVID-19 patients
are at an increased risk of failing to defend themselves against
species like the fungi that cause mucormycosis because of these
factors.
Discussion
Mucormycosis was already much more widespread in India
than in any other country prior to the pandemic [11]. In India,
it affects 14 out of every 100,000 people, compared to 0.06 out
of 100,000 in Australia, for example [7]. Increased serum iron
levels and long-term deferoxamine consumption have recently
been linked to an increased susceptibility to mucor infection [12].
Rhizopus species may use deferoxamine as a xenosiderophore
to supplement previously inaccessible iron, allowing them to
accumulate 8 to 40 times more of it [13]. COVID-19-associated
mucormycosis (CAMCR) cases (total 41) were reviewed by John et
al. [1] to identify risk factors, clinical characteristics, and outcomes.
Patients with diabetes mellitus (DM) (94%) were more likely to
have CAMCR, particularly those with poorly regulated DM (67%)
and moderate or critical COVID-19 (95 percent). CAMR is the result
of the collision of two storms, one DM and the other COVID-19.
Doctors conclude that steroids, a life-saving therapy for serious and
critically ill Covid-19 patients, could be triggering mucormycosis,
which has a 54 percent overall mortality rate.
Mucormycosis is 70 times more common in India than it is
worldwide [7]. There are many potential explanations, including
the fact that India has a higher incidence of “uncontrolled diabetes.”
Many of the patients they observed were unaware that they had
diabetes before they were diagnosed with black fungus, highlighting
“the absence of routine health check-ups in the Indian community.”
Due to delays in finding medical treatment and diagnosing the
disease, as well as difficulties in treating the advanced stage of
infection, the mortality rate for mucormycosis in India is also
remarkably high [7].
Covid-19 infections are more serious in people with
diabetes and obesity. This increases their chances of receiving
corticosteroids, which are often used to treat Covid-19 [14].
However, corticosteroids, in combination with diabetes, raise the
risk of mucormycosis. Meanwhile, the virus that causes Covid-19
can damage airway tissue and blood vessels, putting people at
risk of fungal infection. Harm to tissue and blood vessels caused
by Covid-19 infection, corticosteroid therapy, elevated background
rates of diabetes in the population most seriously affected by the
coronavirus, and, most significantly, more widespread exposure
to the fungus in the environment are all likely factors in India’s
mucormycosis situation. It can grow anywhere as a mold, but it
appears to fester in tropical countries due to the humidity.
Conclusion
Mucormycosis is more common in India than it is worldwide. Mucorales fungi are opportunistic, infecting sinus and brain, lung, skin, gastrointestinal tract of people with a compromised immune system, disseminated mucormycosis typically occurs in people who are already sick from other medical conditions like COVID-19. White fungus can affect the lungs as well as other body parts such as the nails, skin, stomach, kidneys, brain, private parts, and mouth. Yellow fungus may cause pus leakage and slow wound healing, starvation and organ failure, and sunken eyes due to necrosis in severe cases. Controlling these fungal infections would necessitate improved vigilance, better testing to detect them early, as well as an emphasis on diabetes management, maintenance of all round hygiene during Covid infection, and the judicious use of corticosteroids. Patients will need access to surgery and antifungal care as soon as possible. A rapid rise in cases of mucormycosis has added to the challenges faced by India’s healthcare system as it deals with a massive second wave of COVID-19 infections. However, urgent research into the prevention of these infections is needed.
References
- John TM, Jacob CN, Kontoyiannis DP (2021) When uncontrolled diabetes mellitus and severe covid-19 converge: the perfect storm for mucormycosis. Journal of Fungi 7(4): 298.
- Jeong W, Keighley C, Wolfe R, Lee WL, Slavin MA, et al. (2019) The epidemiology and clinical manifestations of mucormycosis: a systematic review and meta-analysis of case reports. Clin Microbiol Infect 25(1): 26-34.
- Petrikkos G, Skiada A, Lortholary O, Roilides E, Walsh TJ, et al. (2012) Epidemiology and clinical manifestations of mucormycosis. Clin Infect Dis 54 Suppl 1: S23-34.
- Latge JP, Chamilos G (2019) Aspergillus fumigatus and aspergillosis in 2019. Clin Microbiol Rev 33(1): e00140-18.
- Barnes PD, Marr KA (2006) Aspergillosis: spectrum of disease, diagnosis, and treatment. Infect Dis Clin North Am 20(3): 545-561.
- Roden MM, Zaoutis TE, Buchanan WL, Knudsen TA, Sarkisova TA, et al. (2005) Epidemiology and outcome of zygomycosis: a review of 929 reported cases. Clin Infect Dis 41(5): 634-653.
- Prakash H, Chakrabarti A (2021) Epidemiology of mucormycosis in India. Microorganisms 9(3): 523.
- Nath A, Khan A, Hashim Z, Patra JK (2017) Prevalence of Aspergillus hypersensitivity and allergic bronchopulmonary aspergillosis in patients with bronchial asthma at a tertiary care center in North India. Lung India 34(2): 150-154.
- Agarwal R, Gupta D, Aggarwal AN, Saxena AK, Chakrabarti A, et al. (2007) Clinical significance of hyperattenuating mucoid impaction in allergic bronchopulmonary aspergillosis: An analysis of 155 patients. Chest 132(4): 1183-1190.
- Pare J, Sigler L (2016) An overview of reptile fungal pathogens in the genera Nannizziopsis, Paranannizziopsis, and Ophidiomyces. Journal of Herpetological Medicine and Surgery 26: 46-53.
- Prakash H, Chakrabarti A (2019) Global epidemiology of mucormycosis. J Fungi (Basel) 5(1): 26.
- Boelaert JR, Van Cutsem J, De Locht M, Schneider YJ, Crichton RR (1994) Deferoxamine augments growth and pathogenicity of Rhizopus, while hydroxypyridinone chelators have no effect. Kidney Int 45(3): 667-671.
- Ibrahim AS, Spellberg B, Edwards J (2008) Iron acquisition: a novel perspective on mucormycosis pathogenesis and treatment. Curr Opin Infect Dis 21(6): 620-625.
- Ortiz-Prado E, Simbana-Rivera K, Gomez-Barreno L, Rubio-Neira M, Guaman LP, et al. (2020) Clinical, molecular, and epidemiological characterization of the SARS-CoV-2 virus and the Coronavirus Disease 2019 (COVID-19), a comprehensive literature review. Diagn Microbiol Infect Dis 98(1): 115094.
© 2021 Chittaranjan Baruah. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






