- Submissions

Full Text
Advancements in Case Studies
Docetaxel-Induced Supravenous Serpentine Dermatitis: A Case Report
Hossain N1*, Eshtiaghi P2, Miller Monthrope Y3, Champagne T2 and Rashida Haq4
1Department of Internal Medicine, Canada
2Department of Dermatology, Canada
3Department of Laboratory Medicine, Canada
4Department of Education-Oncology, Canada
*Corresponding author: Nazia Hossain, Department of Internal Medicine, University of Toronto, Canada
Submission: December 03, 2020;Published: December 10, 2020

ISSN 2639-0531Volume2 Issue5
Abstract
Background: Supra-venous serpentine dermatitis is a rare and self-limited cutaneous reaction to various chemotherapeutic agents.
Case presentation: We describe a case of supra-venous serpentine dermatitis triggered by docetaxel in a middle-aged female patient who received chemotherapy for triple negative breast cancer. Lesions affected the chest, neck, and the arm that was used to infuse docetaxel. The diagnosis was based on skin biopsy results showing pathology consistent with an interface dermatitis. The patient was treated with oral and topical glucocorticoids. Her second cycle of chemotherapy was infused at a slower rate, preceded and followed by boluses of normal saline. Her acute reaction resolved after 2 weeks and she tolerated her second cycle of docetaxel-cyclophosphamide without issues.
Conclusion: Oncologists and dermatologists should be aware of this potentially alarming reaction to docetaxel and other chemotherapeutic agents because adjustments to therapy are unnecessary and may result in undue harm as a result of suboptimal cancer treatment.
Keywords: Docetaxel; Supra-venous; Dermatitis; Cutaneous; Toxicity; Chemotherapy; Breast cancer
Abbreviations: ED: Emergency Department; HSV: Herpes Simplex Virus; PCR: Polymerase Chain Reaction; VZV: Varicella Zoster Virus
Introduction
Docetaxel is a taxane chemotherapy used to treat a variety of malignancies, including those of the breast and prostate [1,2]. It promotes stabilization of microtubules to inhibit cell division and promote apoptosis. Possible adverse effects can affect almost every organ including those of the cardiovascular, respiratory, gastrointestinal, nervous, and immune systems [3]. Cutaneous reactions are particularly common [4]. We describe a case of docetaxel-induced supra-venous serpentine dermatitis, which is a potentially alarming interface dermatitis with few case reports in the literature [5-11].
Case Presentation
A 61-year-old female presented to the emergency department (ED) with a one-day history of fever (temperature 38 degrees Celsius) and a two-day history of painless, nonpruritic vesicles on her right breast. Her past medical history was remarkable for a recent diagnosis of stage pT1cN0 triple negative breast cancer. She underwent lumpectomy and sentinel lymph node biopsy and had her first cycle of adjuvant chemotherapy with docetaxel and cyclophosphamide 5 days prior to her presentation to the ED. She had no other medical conditions and took no regular medications, vitamins, or supplements. She had no known drug allergies. Social and family histories were non-contributory. On dermatologic examination, she had two well-demarcated erythematous plaques studded with superficial papulovesicles on her right breast. She also had a number of small edematous and erythematous papules in a linear pattern on the central chest (Figure 1a). Swabs were collected for HSV/VZV PCR. She was initiated empirically on intravenous acyclovir.
The next day, she developed similar lesions on her anterior and posterior neck (Figure 1b). In addition, she developed a cutaneous eruption on her left arm with an entirely different morphology from the vesicular lesions described. The eruption on her left arm was characterized by a dusky erythematous serpiginous plaque with prominent venous accentuation (Figure 1c). This was the same arm that had been used to infuse her chemotherapy one week prior. Over the next few days, the left arm eruption became more hypertrophic (Figure 1d). The patient also described marked pruritus in the area. All of the patient’s cutaneous symptoms were managed conservatively with acetaminophen and diphenhydramine. HSV/ VZV PCR was negative, so acyclovir was discontinued. Blood and urine cultures also remained negative. A 3mm punch biopsy was taken from the thickest part of the lesion on her arm. Pathology findings showed a lichenoid interface dermatitis with scattered eosinophils. Given the clinical context, the histological findings were consistent with docetaxel-induced supra-venous serpentine dermatitis.
Figure 1: (a) Day 1-Erythematous plaques and papulovesicles on right breast (b) Day 2-Eruption on posterior neck (c) Day 2-Dusky erythematous eruption with prominent venous accentuation on left arm (d) Days 3 and 4-Left arm eruption became more hypertrophic
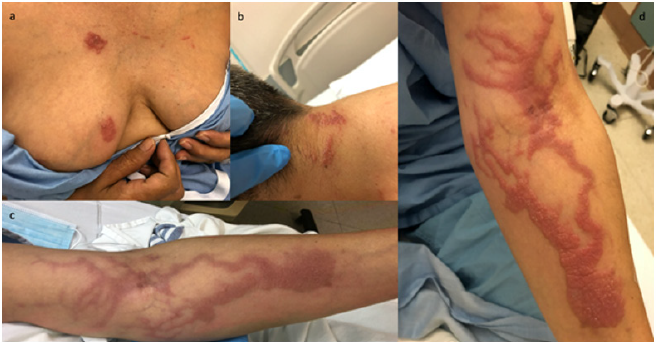
Figure 2: (a) Lesions on breast (b) neck and (c) left arm after treatment with oral prednisone for 7 days and topical betamethasone for 14 days.
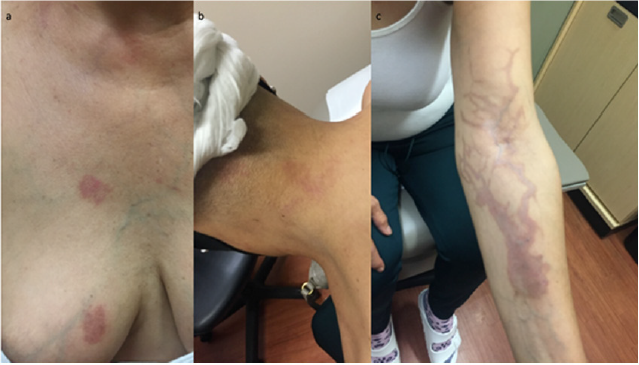
The patient was discharged home with a prescription for a seven-day course of oral prednisone 20mg, as well as betamethasone valerate 0.1% cream applied to the affected areas twice daily for 14 days. After two weeks, she was seen in follow-up by her medical oncologist for consideration of her second cycle of docetaxel and cyclophosphamide. Her lesions had improved remarkably (Figure 2). Her second cycle of chemotherapy was infused at a slower rate and she was administered 250mL of intravenous normal saline before, as well as 500mL after, her chemotherapy. She was also given a three-day prescription for oral dexamethasone 2mg twice daily to be taken after her chemotherapy. She tolerated her second cycle well with no adverse events. Despite the resolution of her initial eruption, post inflammatory pigmentation remains in the areas affected. This is a finding seen following many inflammatory conditions including almost all interface dermatitides, especially in skin of coloured patients [12]. Damage to the basal cell layer of the epidermis where melanocytes are present leads to melanin pigment being released into the dermis. The resulting hyperpigmentation may take years to resolve completely. Avoidance of ultraviolet radiation and regular use of sunscreen can help to speed recovery.
Discussion
Figure 3: (a) This low power view highlights irregular acanthosis, and a band like inflammatory cell infiltrate abutting the dermal epidermal junction (yellow arrows). This view also highlights the deep perivascular and periadnexal inflammatory infiltrates (green arrows) (b) This image shows vacuolar degeneration, numerous necrotic keratinocytes and scattered melanophages (indicating damage to the basal layer) (c) This high-power image highlights rare eosinophils within the inflammatory infiltrate which is predominantly lymphocytes (yellow circles).
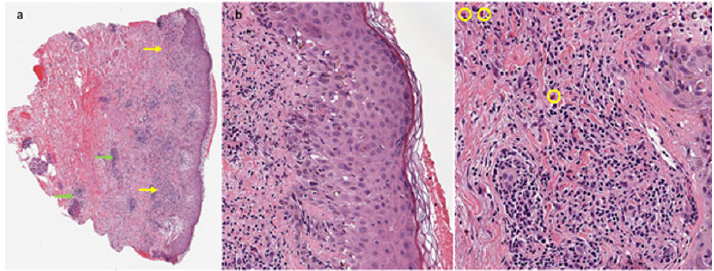
Supra-venous serpentine dermatitis is a rare cutaneous
adverse reaction to irritant medications or chemicals that are
infused intravenously. Few case reports are available in the
literature of similar phenomena caused by chemotherapeutic
agents such as carboplatin, vinorelbine [5], docetaxel [6-9] and
anti-tumour necrosis factor-alpha [10]. Lesions are described as
erythematous macules or purpuric papules that typically develop
24 hours to 15 days after exposure. The exact mechanism of
toxicity remains unclear. It is hypothesized that irritant chemicals
cause direct cytotoxic injury to the vascular endothelium and, in
turn, the dermal and epidermal layers as well as keratinocytes and
melanocytes. Pathological findings are generally reported to show
hyperkeratosis, acanthosis, focal spongiosis, necrotic keratinocytes,
melano-phages, and an interface dermatitis with marked vacuolar
degeneration of the basal cell layer. The presence of a perivascular
inflammatory infiltrate extending to the deep dermis has also been
reported [6,10] (Figure 3).
Supravenous serpentine dermatitis is a self-limited reaction
and typically resolves in several weeks to months. However,
patients may have residual hyperpigmentation of the affected skin.
The acute eruption can be managed with a medium-potency topical
steroid with or without oral glucocorticoids. Importantly, there is
no indication to discontinue or decrease the dose of the offending
agent [5-7]. In order to prevent the reaction with subsequent
exposures, intravenous medications should be infused at a slower
rate with boluses of normal saline before and after to wash out any
toxic metabolites from blood vessels. During long infusion sessions,
central access is preferred over peripheral access. Cold compresses
can be applied over the site of infusion to cause venous constriction
and degradation of metabolites. In addition, compresses can be
used during the acute reaction to decrease pain and inflammation
[5-7].
Conclusion
Supravenous serpentine dermatitis is a rare cutaneous drug eruption secondary to irritant intravenous medications. The acute reaction is managed with topical and oral glucocorticoids. There is no indication to discontinue or adjust the dose of the offending agent. Preventative strategies include using slower infusion rates and infusing boluses of normal saline before and after the drug. Knowledge of this adverse event and its management allowed our patient to continue first line therapy for her malignancy.
Acknowledgement
All clinical images were used with permission granted by the patient.
References
- Lyseng-Williamson KA, Fenton C (2005) Docetaxel: A review of its use in metastatic breast cancer. Drugs 65(17): 2513-2531.
- Basch E, Loblaw DA, Oliver TK, Carducci M, Chen RC, et al. (2014) Systemic therapy in men with metastatic castration-resistant prostate cancer: American Society of Clinical Oncology and Cancer Care Ontario clinical practice guideline. J Clin Oncol 32(30): 3436-3448.
- Ho MY, Mackey JR (2014) Presentation and management of docetaxel-related adverse effects in patients with breast cancer. Cancer Manag and Res 6: 253-259.
- Sibaud V, Loboeuf NR, Roche H, Belum VR, Gladieff L, et al. (2016) Dermatological adverse events with taxane chemotherapy. Eur J Dermatol 26(5): 427-443.
- Akyurek FT, Sari N, Ugurluoglu C, Kurtipek GS (2019) Serpentine supra-venous hyperpigmentation related to carboplatin and vinorelbine chemotherapy: A case report. Dermatol Ther 32(4): e12981.
- Aydogan I, Kavak A, Parlak AH, Alper M, Annakkaya AN, et al. (2005) Persistent serpentine supravenous hyperpigmented eruption associated with docetaxel. J Eur Acad Dermatol Venereol 19(3): 345-347.
- Kamei H, Yano T, Kiura K, Umemura S, Yamane H, et al. (2009) A case of persistent serpentine supravenous hyperpigmented eruption associated with docetaxel. Lung Cancer 49(2): 198-201.
- Chaiyakul S (2018) Docetaxel-induced supravenous serpentine dermatitis: A case report and literature review. J Med Assoc Thai 101: 1297-301.
- Fernandes KAP, Felix PAO (2015) Persistent docetaxel-induced supravenous erythematous eruption. An Bras Dermatol 90(5): 728-730.
- Garcovich S, Burlando M, Rongioletti F, Garcovich A, Parodi A, et al. (2009) Cutaneous drug eruption with an interface dermatitis pattern due to anti-tumour necrosis factor-alpha agents: A relevant class-effect. Acta Dermatol Venereol 90(3): 311-312.
- Spencer HJ (1984) Local erythema multiforme-like drug reaction following intravenous mitomycin C and 5-fluorouracil. J Surg Oncol 26(1): 47-50.
- Davis EC, Callender VD (2010) Post-inflammatory hyperpigmentation: A review of the epidemiology, clinical features, and treatment options in skin of color. J Clin Aesthet Dermatol 3(7): 20-31.
© 2020 Hossain N. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






