- Submissions

Full Text
Advancements in Case Studies
Jet Ventilation a Review
Sikora M, Sonal P and Maurtua M*
Anesthesiology Institute, The Cleveland Clinic Foundation, USA
*Corresponding author: Marco M, Anesthesiology Institute, The Cleveland Clinic Foundation, USA
Submission: October 29, 2019;Published: November 01, 2019

ISSN 2639-0531Volume2 Issue2
Abstract
High frequency jet ventilation, low frequency jet ventilation, and transtracheal jet ventilation share a common purpose, to oxygenate and ventilate the patient based on a high-pressure system connected to a pressure regulator. We are going to review, the most used techniques, oxygenation and ventilation mechanisms, clinical indications, complications and new developments.
Keywords: Jet ventilation, High frequency jet ventilation (HFJV), Low frequency jet ventilation (LFJV), Transtracheal jet ventilation (TTJV), Pendulluft effect, Laminar flow, Venturi effect, Can’t intubate can’t ventilate (CI/CV), Cannula cricothyrotomy, Barotrauma
Abbreviations: HFJV: High Frequency Jet Ventilation; LFJV: Low Frequency Jet Ventilation; TTJV: Transtracheal Jet Ventilation; PIP: Positive Inspiratory Pressure; PEEP: Positive End Expiratory Pressure; CI/CV: Can’t Intubate Can’t Ventilate; ENT: Ear Nose and Throat; PVC: Polyvinylchloride
Introduction
There are several ventilation techniques described under jet ventilation (JV), in this review we are going to focus on high frequency jet ventilation (HFJV), low frequency jet ventilation (LFJV) and transtracheal jet ventilation (TTJV) a subtype of LFJV. HFJV and LFJV share a common purpose, to oxygenate and ventilate based on a high-pressure gas system connected to a pressure regulator that can mechanically (ventilator) or manually deliver a stream of gas through a jet cannula.
Discussion
High frequency jet ventilation (HFJV)
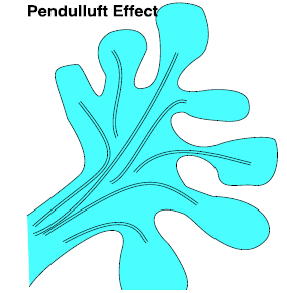
HFJV consists of the intermittent delivery of gas from a high-pressure source connected to a jet ventilator, for example, the Life Pulse 204 by Bunnell Inc, Figure 1. This device is approved for clinical use in neonates and infants [1]. It delivers the jet through a triple-lumen endotracheal tube adapter injector port [1,2]. The control settings include the rate/frequency that ranges from 4-11Hz or 240 to 660 breath per min, the inspiratory time 20 milliseconds to 34 milliseconds and the positive inspiratory pressure (PIP). Positive end expiratory pressure (PEEP) is regulated through the conventional ventilator. It is important to remember that when using HFJV alveolar ventilation does not depend on the rate or frequency of the jet, but rather the difference between PIP and PEEP indicated as delta P [1,2]. This device makes possible the effective removal of CO2 while achieving lower peak and mean airway pressures compared to other conventional techniques of ventilation. Gas exchange during JV in part is due to the conventional delivery of a predetermined volume of gas, however during JV and especially during HFJV, this volume is much smaller than the physiologic tidal volume, therefore other mechanisms have been described that can contribute to a successful ventilation and oxygenation while using this technique. These include, laminar flow, the Pendulluft effect, Taylor dispersion, and cardiogenic mixing. The presence of laminar flow in the airway produces a similar effect to a countercurrent mechanism in which the center of the bronchial tree and alveoli receive the stream of gas molecules pushed forward by the high pressure jet, while the existent gas in the airway is pushed to the periphery of the bronchial tree in the opposite direction, (Figure 2) [3,4]. The Pendulluft effect resides in the anatomical differences among alveoli that lead to an unequal airway resistance and air flow within the lung. Therefore, there is flow of gas molecules inside the lung from areas that are well ventilated to poorly ventilated Figure 3.
Figure 1: Bunnell life pulse HFJV.
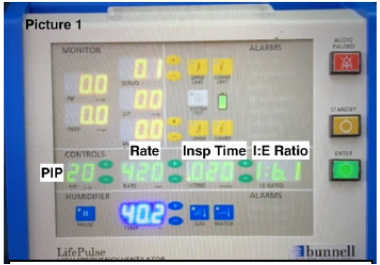
Figure 2: Laminar flow.
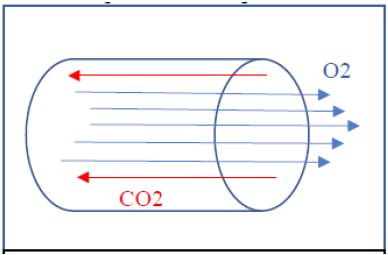
Figure 3: The pendulluft effect.
Taylor dispersion consists of convective streaming of gas and is explained by the diffusion of high velocity central gas molecules to the periphery of the airway. Taylor dispersion occurs more frequently in the smaller airways and further enhances gas mixing and hence exchange. Cardiogenic mixing consists of the mixing of gases due to the pulsatile normal cardiac physiology [4-6]. In adults, HFJV has been used for the treatment of broncho-pleural fistulas, bronchoscopies, micro-laryngeal surgery, airway resection, and end to end anastomosis. In pediatric patients this has been used in the treatment of patients with pulmonary interstitial emphysema, respiratory distress syndrome, etc [5-7].
Low frequency jet ventilation (LFJV)
LFJV shares with HFJV the presence of a high-pressure gas system connected to a down regulation pressure valve. The jet cannula could be placed supraglottic, subglottic, or trans-tracheal. It can also be attached to a rigid bronchoscope, a suspension laryngoscope, placed inside an endotracheal tube, in the trachea, or inserted through a tracheostomy stoma. In the case of LFJV, the jetting is performed manually via hand-triggered devices such as the Sanders injector or Manujet III which allows for the delivery of a controlled gas jet through a cannula appropriately fixed to a bronchoscope or laryngoscope Figure 4. During LFJV supraglottic jetting delivers a stream of gas to the airway at high velocity, but at a slower jet rate of 8 to 10 jets per minute when compared to HFJV [7,8]. The gas molecules driven into the airway generate a vacuum effect that entrains atmospheric gas molecules, making the tidal volume delivered even greater, this phenomenon is called the venturi effect Figure 5. This effect increases the effective tidal volumes delivered. The venturi effect also explains why the peak and mean airway pressures increase to a greater degree when using supraglottic jetting versus subglottic or transtracheal jetting. Other factors affecting airway pressures include the frequency of the jet, the duration of the jet, and the presence of airway obstruction. A higher frequency jet generates auto-PEEP and a greater duration of the jet, an increase in tidal volumes that might produce a direct increase in airway pressures [8,9].
Figure 4: Sanders injector.
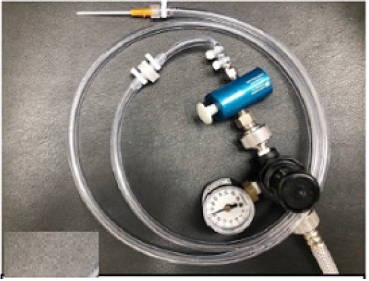
LFJV main applications include short surgical (Ear, nose and throat) ENT procedures and during TTJV as a rescue measure in the can’t intubate can’t ventilate (CI/CV) airway emergency. During ENT procedures LFJV is generally performed from the supraglottic area through a metallic jet Figure 5. Venturi effect explained cannula secured in the rigid laryngoscope used during suspension micro-laryngoscopy by the ENT specialist. This technique takes advantage of the venturi effect and therefore increases the volume of gas delivered. The jetting is performed by the anesthesiologist who at the same time monitors the patient’s chest expansion and passive chest relaxation during the jetting pause to avoid barotrauma. The anesthesiologist and ENT surgeon both monitor the jet cannula position to prevent soft tissue lacerations in the patient’s upper airway [8,9]. The pressure to be delivered should be set to the lowest pressure that accomplishes the goal of successful oxygenation and ventilation. The recommended pressures are between 20 and 30 PSI in adults. One has to check the pressure regulator gauge before its use, since this device is capable of delivering a maximum of 50 PSI of pressure, equal to the operating room wall O2 pressure source, which for reference is fully capable of insufflating a car tire. Supraglottic and subglottic LFJV, has been used also in patients undergoing upper airway laser procedures since both techniques avoid the placement of a polyvinylchloride (PVC) endotracheal tube and improve airway visualization. However, neither technique completely prevents an airway fire, since oxygen at high concentrations can be trapped in and around drapes and towels. Another complication may arise with the use of subglottic catheters, in that they might degrade or fracture and be pushed to the distal bronchial tree by JV, if degradation goes unrecognized [10,11].
Figure 5: Venturi effect explained.
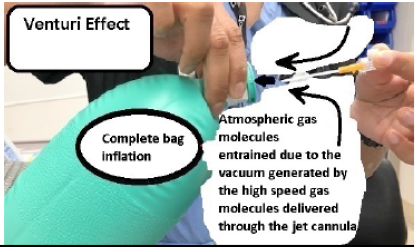
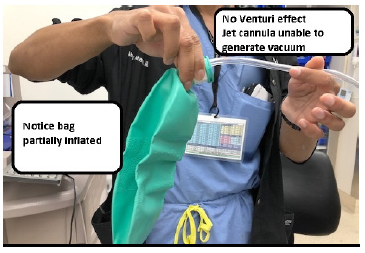
Figure 6: Venturi effect.

If one considers the use of TTJV during the CI/CV case scenario, one must understand that no venturi effect will supplement air entry using this airway management technique Figure 6 & 7. Flint et al. [12] studied and compared different methods of ventilation via cannula cricothyroidotomy. His study showed that the only methods that achieved minute ventilations above 2liters per minute were with devices dedicated to deliver high pressure gas flows, for example, the manujet or the sanders jet ventilation device. In addition, they had to be connected to cannulas of 16 gauge in diameter or greater. That’s why this technique’s primary goal is to keep the patient oxygenated and should be considered a temporary airway intervention followed by an emergent cricothyrotomy or tracheostomy [12].
Figure 7: No venturi effect.
The old concept of a 14-gauge catheter attached to a 3ml syringe and a 7mm endotracheal tube connector connected to an ambu-bag proved to be inadequate to deliver physiologic tidal volumes (Figure 8) [13]. Complications related to the use of JV in general, could be divided in 1. Technical complications, with the most common being disconnection or kinking of the jet catheter. To avoid this complication, the jet cannula should be continuously controlled by a health care provider, who’s only mission is to keep the cannula in the correct place. 2. Adequacy of gas exchange, hypoxia. and hypercarbia. 3. Physical complications, desiccation of the tracheobronchial tree, 4. Barotrauma, pneumothorax, pneumomediastinum, pneumopericardium, pneumoperitoneum, subcutaneous emphysema, 5. Complications related to jet catheter malposition, laceration of the upper airway mucosa, gastric insufflation, gastric rupture and necrotizing trachea-bronchitis [8,11,13]. Jaquet Y et al. [14] in a 10year review of the most severe complications related to JV, concluded that subglottic JV was the major independent factor for severe barotrauma. Duggan LV et al. [15] after performing a systematic review for studies describing TTJV in human subjects to determine complication rates of TTJV in the emergent CI/CV vs the elective surgical setting, found that device failure (inability to place or use TTJV) occurred in 42% of the TTJV cases during emergency airway management vs 0.3% in the non-emergent airway management. Barotrauma occurred in 32% of the TTJV performed during emergent airway management vs 15% when TTJV was performed non emergently. In addition, the study added that an open surgical technique performed by surgeons was almost 100% successful, what might indicate that a cricothyrotomy or tracheostomy might be a more effective way to secure the airway or may also mean that anesthesiologists should be better trained to establish a surgical airway. Some professionals even question the use of TTJV temporarily for oxygenation purposes, because TTJV was reported to be associated with subcutaneous emphysema making subsequent establishment of a definitive airway through cricothyrotomy much more difficult, if not impossible, (Figure 9) [15]. Finally, the authors recommended to re-evaluate the use of TTJV during the CI/CV airway management and reconsider its recommendation by known difficult airway algorithms, and to use an open surgical technique vs TTJV [15].
Figure 8: Old method, inadequate ventilation.
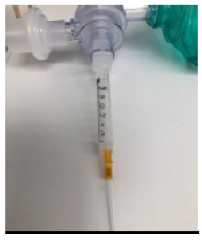
Figure 9: Complications from TTJV in a patient with an obstructed airway.

Figure 10: Ventrain + Cricath LFJV system with active expiration capability.

Recently, it became available a manual LFJV system called ventrain. Ventrain offers in addition to deliver a high-pressure gas jet, the capability of an active expiration phase by suction and venturi effect. Therefore, this device might prevent barotrauma when there is a complete airway obstruction. The recommended jet cannula to be used with this device is a 2mm needle cricothyrotomy cannula (Cricath) Figure 10. As advertised by the manufacturer, this device is capable of delivering up to a minute ventilation of 7 liters. In addition, 2 seconds of inspiration followed by 2 seconds of expiration results in 500ml tidal volumes [16,17]. This device definitely changes the old clinical concepts to the use of TTJV during the CI/CV case scenario. Only clinical experience with its use will confirm the benefits of this new technology.
Discussion
The increase of the intra-abdominal pressure is caused by the increase in the volume of the abdominal organs, the appearance of the free liquid, the diminished abdominal wall compliance as well as the increased pressured in the chest cavity (especially during mechanical ventilation), and the massive infusion therapy [8,9]. In our opinion, the development of the abdominal hypertension and abdominal compartment syndrome in the patient with acute hepatitis was caused by the increase in volume of the parenchymal organs (hepato-splenomegaly), the appearance of ascites, the abdominal swelling, and the inhibition of the gastrointestinal tract motility.
Development of ACS was preceded by gastrointestinal disorders in the form of the absence of peristaltic noises, bloating, constipation, and hemorrhagic stasis of the gastric contents. The damage of the gastrointestinal tract (GIT) in our patient was not included in the primary lesion. Pathogenesis of the gastro-intestinal lesion could involve neuroendocrine disorders, hypoxic and ischemic injuries, the impact of cytokines and other biologically active substances, dysbiosis and side effects of medications etc. [10]. In our patients, the GIT disorders preceded other signs of multiple organs failure, and possibly, stimulated the rise of the abdominal pressure. The accumulation of the free fluids in the physiological cavities (peritoneal and pleural) also belongs to the typical manifestations of intra-abdominal hypertension syndrome and the abdominal compartment syndrome. For instance, there was described direct relationship between the presence of the free fluid in the abdomen and the increased intra-abdominal pressure [11]. The free fluid could be either cause an abdominal compression or appear because of abdominal compression. In our patient the free fluid was found before the symptoms of the abdominal compression were observed. In the patient with the acute hepatitis B, the ascites formation obviously was influenced by the hemodynamic disorders and dysproteinemia.
The fact that intra-abdominal hypertension might cause multiple organs disorders suggests that its timely correction is needed. The methods for treating the intra-abdominal hypertension syndrome and abdominal compartment syndrome include both surgical and therapeutic methods [12]. Among therapeutic methods mostly recommended appropriate sedation and analgesia to improve the compliance of the abdominal wall; the reduction of the intestinal contents through drainage and prokinetics; the removal of the free fluid from the abdominal and pleural cavities; water balance correction; application of diuretics and colloid solutions; and the optimization of the respiratory support [13]. This patient received nasogastric and rectal drainage, early enteral nutrition, adequate sedation, corrected fluid therapy and were provided with negative fluid balance. Treatment was sufficient to achieve full recovery.
Conclusion
Jet ventilation is a novel technique to oxygenate and ventilate patients. It is commonly utilized in the treatment of certain pulmonary pathologies and management of thoracic surgical patients requiring lower pulmonary pressures. Equally important, it is effective in the management of patients undergoing ENT procedures and patients who require emergency airway procedures. In order for this technique to be utilized appropriately we recommend the clinician be knowledgeable about the particular mechanisms of gas exchange outlined in this article. Furthermore, clinicians need full understanding of the limitations and complications that might arise from its use. With regards to the CI/CV case scenario, jet ventilation was questioned as a safe technique in the past due to reported barotrauma and subcutaneous emphysema, especially in the patient with near complete airway obstruction. However, new technology and innovation such as the Ventrain + Cricath may offer a definitive solution to the problem of barotrauma, and we believe has the potential to become the gold standard in the early management of the CI/CV emergency airway.
References
- http://www.bunl.com/hall-of-fame-lectures.html
- Mammel MC, Courtney SE (2017) High-Frequency Ventilation. Assisted ventilation of the neonate (6th edn).
- Galmen K, Harbut P, Freedman J, Jakobson JG (2017) The use of high-frequency ventilation during general anesthesia: An update. F1000Res 6: 756.
- Conlon CE (2012) High frequency jet ventilation. World Federation of Societies of Anesthesiologists Anesthesia Tutorial of the week.
- Morgan GE, Mikhail MS, Murray MJ (2006) Clinical anesthesia. In: Morgan GE, Mikhail MS, Murray MJ (Eds.), (4th edn), Chapter 49, Critical Care, pp. 1034-1035
- Jane JP (2005) High-frequency oscillatory ventilation: Mechanisms of gas exchange and lung mechanics. Crit Care Med 33(3 Suppl): S135-141.
- Standiford TJ, Morganroth ML (2005) High-frequency ventilation. Chest 96(6): 1380-1389.
- Doyle J (2016) Jet ventilation for otolaryngologic procedures-A mini-review. J Anesth Crit Care Open Access 6(4): 00236.
- Evans E, Biro P, Bedford N (2007) Jet ventilation. Continuing Education in Anesthesia Critical Care & Pain 7(1).
- Annette GP, Gerald W, Allan G, Tom K, Jay C, et al. (1993) Upper airway management guide provided for laser airway surgery. Anesthesia Patient Safety Foundation Newsletter 8(2).
- Patel A (2013) Anesthesia for Laser Airway Surgery. In: (3rd edn), Benumof and Hagberg's Airway Management-Chapter 40, pp. 824-858.
- Flint NJ, Russell WC, Thompson JP (2009) Comparison of different methods of ventilation via cannula cricothyrotomy in a trachea-lung model. Br J Anaesth 103(6): 891-895.
- Berré J, Ros AM, Vincent JL, Dufaye P, Brimioulle S, et al. (1987) Technical and psychological complications of high-frequency jet ventilation. Intensive Care Med 13(2): 96-99.
- Jaquet Y, Monnier P, Van MG, Ravussin P, Spahn DR, et al. (2006) Complications of different ventilation strategies in endoscopic laryngeal surgery: A 10-year review. Anesthesiology 104 (1): 52-59.
- Duggan LV, Ballantyne SB, Law JA, Morris IR, Murphhy MF, et al. (2016) Transtracheal jet ventilation in the can’t intubate can’t oxygenate emergency : A systematic review. British Journal of Anaesthesia 117 (Suppl 1): i28-i38.
- Hamaekers HEW, Borg PAJ, Enk DV (2012) Ventrain: An ejector ventilator for emergency use. British Journal of Anaesthesia 108(6): 1017-1021.
- Torres (2016) Ventrain+Cricath= The jet ventilator that works.
© 2019 Marco M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






