- Submissions

Full Text
Advancements in Case Studies
Dermatofibrosarcoma Protuberans Of the Vulva Treated with Mohs Micrographic Surgery
Miguel Olmos Pérez1*, María Fernanda Corrales Sierra1 and Rafael Parra-Medina2,3
1 Department of Dermatology, Colombia
2 Department of Pathology, Colombia
3 Research institute. Colombia
*Corresponding author: Miguel Olmos, Department of Dermatology, Colombia
Submission: December 12, 2018;Published: February 05, 2019

ISSN 2639-0531Volume1 Issue4
Abstract
Dermatofibrosarcoma protuberans (DFSP) of the vulva is extremely rare conditions. It has been published approximately 43 case reports in medical literature; most tumors arise on the labia majora. We present a 57-year-old woman with DFSP in vulva that was removed by Mohs Micrographic Surgery technique. The wound exhibited a satisfying functional and cosmetic appearance, with no evidence of deformity of the vulva
Keywords: Dermatofibrosarcoma protuberans, Mohs surgery, Vulva
Case Report
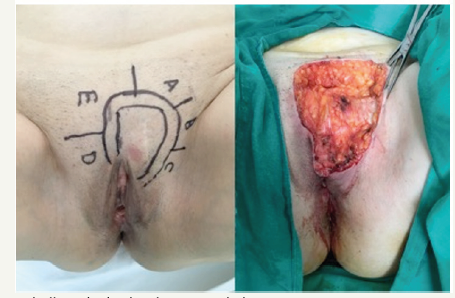
A 57-year-old woman, with no significant past medical history, who presented with a growing nodular lesion in the pubic area. She referred a progressive and asymptomatic enlargement for the past 3 years, eventually compromising the left labia majora. In 2014, a biopsy of the lesion was performed. Immunohistochemical staining showed diffuse CD34 expression, confirming the diagnosis of Dermatofibrosarcoma protuberans (DFSP). The tumor was then surgically removed but histology after surgery showed an incompletely excised DFSP. Despite of the results and the medical advice for a second surgery, the patient never followed up again until two years later when she noticed recurrence of the tumor on the surgical scar. Physical examination revealed a large tumor on the pubic area. The tumor consisted of a 5 x 6cm, ill-defined, pink, indurated, nontender nodular mass. On palpation, the nodule was adhered to deep planes and involved the pubis and extended to the left labia majora of the vulva. No lymphadenopathy was noted. In order to determine the extent of the tumor and its relationship with adjacent structures, a preoperative magnetic resonance imaging study was performed. Coronal and transverse T1 and T2-weighted images revealed a 36 x 36mm solid mass on the left side of the pubis. Abdominal computed tomography scan was normal. The lesion was surgically excised using the Mohs technique (Figure 1).
Figure 1:The lesion was surgically excised using the MMS technique.
The histopathologic examination showed complete tumor clearance after one stage of Mohs micrographic surgery (MMS). The diagnosis of DFSP was confirmed on the sections performed to the center of the specimen. Dermis was affected by a highly cellular tumor composed of fascicles of spindle-shaped cells arranged in a storiform growth pattern. The subcutaneous fat tissue was infiltrated and showed entrapment of mature adipocytes by the neoplastic cells. The mitotic rate was low. The defect was repaired using a rotation flap taken from the adjacent skin of hypogastrium. The wound was then closed in a layered fashion from the deep fascia to the epidermis (Figure 2). At a subsequent follow-up visit, the wound exhibited a satisfying functional and cosmetic appearance, with no evidence of deformity of the vulva (Figure 3).
Figure 2:The wound was then closed in a layered fashion from the deep fascia to the epidermis.

Figure 3:Functional and cosmetic appearance, with no evidence of deformity of the vulva

Discussion
Dermatofibrosarcoma protuberans (DFSP) is a neoplasm that arises from the dermis and subcutaneous tissue with an overall incidence of 4.1 per million person-years and accounting for approximately 0.1% of all malignancies. The preferable location of this type of tumor is the trunk, followed by extremities. However, its appearance in genitals has also been described in less than 1% of patients, being the least common location [1]. The involvement of the vulvar area and clitoris is extremely rare. It has been published approximately 43 case reports in medical literature; most tumors arise on the labia majora [2,3]. DFSP of the vulva tends to affect women between 22 to 83 years; the median patient age is 43 years.
The tumor size reported in medical literature are range o.5 to 12cm, median 3.5cm [2,3]. The typical clinical presentation consists of a firm plaque with surrounding red to blue discoloration or less often with a solitary subcutaneous nodule. Due to its asymptomatic nature, it frequently escapes detection in the early stages of the disease [4].
Histologically, DFSP is characterized by fascicles of spindle cells arranged in a storiform growth pattern in the center of the lesion. The peripheral portion of the tumor is hypocellular with a mixture of slender cells and dermal collagen, whereas, in deep region, the tumor spreads along connective tissue and between adnexae, or it infiltrates the subcutaneous fat, creating a honeycomb appearance. Nuclear pleomorphism is absent and the mitotic index is low. Immunohistochemically, neoplastic cells stain strongly positive for CD34 and vimentin and negative for S-100, smooth muscle actin, desmin and keratin [1]. DFSP is considered locally aggressive, with frequent relapses but low metastatic potential. Lymphatic dissemination is uncommon, and metastases, when occurred, typically involved the lungs and bones [5].
Treatment options for DFSP of the vulva include simple excision, radical vulvectomy, MMS, and occasionally, radiotherapy and chemotherapy. Surgery is considered the optimal therapeutic approach with the highest cure rates. Traditionally, wide local excision (WLE) has been considered the therapy of choice of both primary and recurrent lesions, but the risk of relapses is up to 32%, due to the microscopic projections of the tumor beyond the central nodule. MMS uses systematic sectioning with 100% of the tumor margin being microscopically evaluated; this increases the probability of any tumor projections being detected with maximum preservation of healthy tissue, minimizing recurrence and favoring better aesthetic and functional outcomes. Tissue conservation is fundamental to preserve function, especially of the clitoris [4,6].
References
- Reha J, Katz SC (2016) Dermatofibrosarcoma Protuberans. Surg Clin North Am 96(5): 1031-1046.
- Edelweiss M, Malpica A (2010) Dermatofibrosarcoma protuberans of the vulva: a clinicopathologic and immunohistochemical study of 13 cases. Am J Surg Pathol 34(3): 393-400.
- Gilani S, Al Khafaji B (2014) Dermatofibrosarcoma protuberans of the vulva: a mesenchymal tumour with a broad differential diagnosis and review of literature. Pathologica 106(4): 338-341.
- Doufekas K, Duncan TJ, Williamson KM, Varma S, Nunns D (2009) Mohs micrographic surgery for dermatofibrosarcoma protuberans of the vulva. Obstet Gynecol Int.
- Soergel TM, Doering DL, Oconnor D (1998) Metastatic dermatofibrosarcoma protuberans of the vulva. Gynecol Oncol 71(2): 320-324.
- Bertolli E, Bretchbuhl ER, Camarço WR, Campagnari M, Molina AS, et al. (2014) Dermatofibrosarcoma protuberans of the vulva: margins assessment and reconstructive options - a report of two cases. World J Surg Oncol 12(1): 399.
© 2019 Miguel Olmos Pérez. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






