- Submissions

Full Text
Advances in Complementary & Alternative medicine
Diabetic Patients at Risk from Herb-Drug Interactions
Saud M Alsanad* and Osama A Al-Khamees
Department of Pharmacology, Imam Mohammad Ibn Saud Islamic University (IMSIU), Saudi Arabia
*Corresponding author: Saud M Alsanad, Department of Pharmacology, College of Medicine, Imam Mohammad Ibn Saud Islamic University (IMSIU), Riyadh 13317, Saudi Arabia
Submission: May 24, 2023;Published: June 12, 2023

ISSN: 2637-7802 Volume 7 Issue 5
Abstract
Background: It is well known that diabetic patients use Herbal Medicines (HMs) and antidiabetic drugs concurrently. Therefore, there is always the possibility of Herb-Drug Interactions (HDIs). This study attempted to find an appropriate path to accurately assess the risk of HM usage by diabetic patients.
Methods: The natural medicines comprehensive database and other resources were used to assess the risk of HDIs for about 130 herb-drug combinations used by 38 patients.
Result: Most of these interactions were assessed as “moderate interactions”, with only one assessed as a “major interaction”. No adverse events or harm were reported as the assessments were carried out retrospectively. The vast majority of the evidence on HDIs was based upon the pharmacological activities of the herbal and conventional medicines rather than the clinical outcomes.
Conclusion: Our assessments highlight the gulf between theoretical and real clinical interactions. Although this type of assessment does not measure the actual harms/benefits of HDIs, it highlights the need to reconsider the methods used to assess herb safety and efficacy. This will help physicians and healthcare professionals to provide considered advice to patients based upon documented evidence.
Keywords:Diabetes; Diabetic patients; Herb-drug interactions; Herbal medicines; Antidiabetic medicines; Complementary medicines; Alternative medicines; Saudi Arabia
Introduction
The use of Herbal Medicines (HMs) is well documented and is particularly common in patients with chronic diseases such as diabetes. It has been reported that patients with diabetes are 1.6 times more likely to use HMs than non-diabetics for a range of reasons [1]. The global prevalence of HM usage among diabetic patients was reported as ranging from 17% to 73% [2,3]. However, an updated systematic review showed a prevalence rate of 8-89% with more than 223 HMs identified [4,5]. Patients in Saudi Arabia, particularly diabetic patients, tend to use HMs very frequently [6-12]. Studies have revealed that up to 70% of the Saudi diabetic population have tried HMs [13-17]. The possibility of interactions occurring between herbs and conventional drugs (Herb-Drug Interactions, “HDIs”) may be higher than between multiple conventional drugs because of the large number of components in an herb compared to the single active substance used in conventional medicine [18]. However, the incidence of HDIs is not yet fully known, and there is currently no body of reliable information to draw upon when assessing the scale of any possible problem or predicting clinical outcomes [19]. The lack of evidence may be due to under-reporting or unrecognized interactions, but there is also the possibility that many herbal medicines have a generally safe profile and do not interact significantly with drugs. Given the poor quality of information available, it can be difficult to put the problem into perspective and in the absence of good evidence, speculation has arisen [20]. The concurrent use of antidiabetic herbs and conventional drugs may result in HDIs leading to enhanced effects (which may be desirable clinically), decreased pharmacological effects, or Adverse Drug Events (ADEs), such as hypoglycemia [21,22].
A study exploring interactions between HMs and conventional medicines revealed that 54% of patients were taking at least one combination which were documented as leading to a possible interaction. The researchers found 45 potential interactions, the most serious of which was considered to be between gingko and aspirin (because gingko can reduce platelet aggregation and may increase the risk of bleeding), and between garlic and warfarin (because garlic has an anticoagulant effect). Interestingly, despite this concern, no attempt was made to confirm the occurrence of these interactions, and no adverse events were recorded [23]. Another study on 197 patients showed that about 50% of the patients were at risk of HDIs. Almost 94% of these HDIs were not categorized as serious based on the limited available evidence, while the remaining 6% of interactions were considered potentially severe. However, no adverse events were reported [24].
The fact that these patients suffered no adverse effects is interesting as it reflects the gap between theoretical and actual clinical interactions. Most studies have primarily assessed the safety of HMs theoretically or without always taking into account the actual outcomes of HMs taken by diabetic patients, which can give rise to an inappropriate assessment of risk based on speculation. Our study, therefore, was based on the real-life practice of diabetic patients taking HMs and their experiences of benefit or harm. An individual assessment for each patient was implemented to assess the risk posed by the drug regime and HM consumption, reflecting more closely the actual risk that diabetic patients may face. This will help to provide sensible advice for healthcare professionals and diabetic patients, based upon documented evidence.
Methods
Eligible diabetic patients attending the Medical Services Centre at Imam Mohammed Ibn Saud Islamic University (IMSIU), Riyadh, Kingdom of Saudi Arabia were included in the study as participants over the period from January-March 2022. Diabetic patients aged over 18 years who were currently receiving treatment following a diabetic diagnosis and were able to understand the questionnaire were interviewed by experienced clinical research assistants. The interviewers clearly explained to participants the purpose of the study and assured them that any information they provided would remain strictly confidential and would only be used for research purposes. Patients were asked about all the HMs they had taken, rather than asking them to select HMs from a pre-prepared list, in order to investigate the variety of HMs that they believed could help them manage their diabetes. Also, patients were asked to list all of the conventional medicines they were taking as part of their usual drug regime, as well as any other prescribed conventional drugs taken at the same time as HMs. Information on patients’ demographics and their experiences of HM usage was also obtained.
Questionnaires were formulated based on special consideration of the findings of previously published papers and to align with the circumstances of the target participants. The questionnaire items were validated by a panel of academics, healthcare professionals, and diabetic patients. Interviews were carried out in the Arabic language and the authors then translated the final transcripts into English. To validate the translation, a bilingual academic reviewed the translation. The Natural Medicines Comprehensive Database was used as the basis for the assessment of interactions between HMs and conventional medicines [25].
Also, a literature search was carried out when necessary (to obtain very recent data or when a supplement was not included in the database). This database is a comprehensive, evidence-based, and reasonably up-to-date reference for interactions between HMs/dietary supplements and conventional medicines. The Natural Medicines Comprehensive Database classifies interactions into “major interaction” (do not use combination; contraindicated; strongly discourage patients from using this combination; a serious adverse outcome could occur), “moderate interaction” (use cautiously or avoid combination; warn patients that a significant interaction or adverse outcome could occur), and “minor interaction” (be aware that there is a chance of an interaction; advise patients to watch for warning signs of a potential interaction). Participants were categorized as an HM user if they reported that they had used HMs. Data collected from the questionnaires were entered into SPSS (V.23) to generate descriptive statistics on patient characteristics, including sociodemographic, diabetes diagnosis, specific HMs being taken, prescribed medicines taken concurrently, and the individual HDI assessments. Ethical approval was obtained from the Institutional Review Board (IRB) committee of the College of Medicine at Imam Mohammed Ibn Saud Islamic University (IMSIU) (Ref.: 00105/5/2021). For other required local ethical approvals, procedures were followed as necessary.
Result
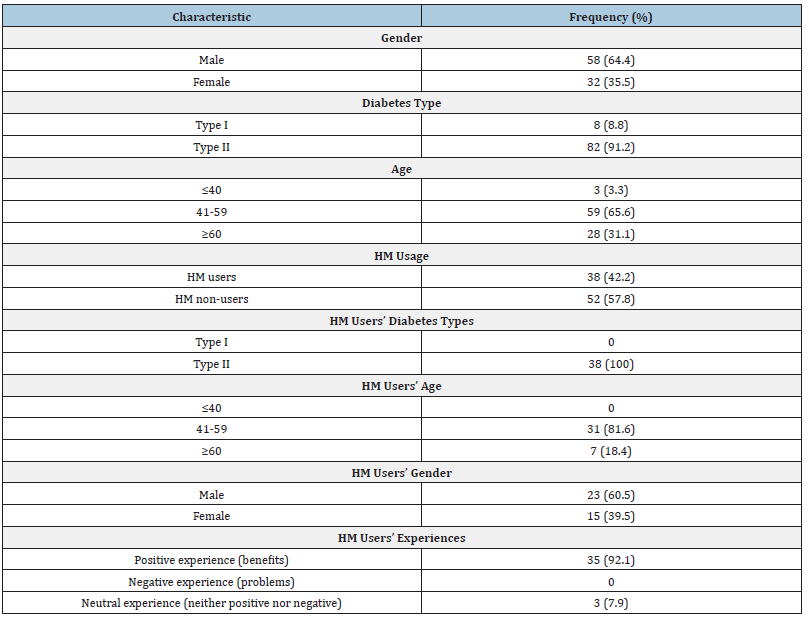
A total of 90 diabetic patients were involved in this study. Of these participants, (38; 42.2%) were HM users. All of the HM users were type II diabetes patients, and most of them were male (23; 60.5%). Patients aged 41-59 (31;81.6%) took HMs more frequently than the other age groups. According to the HM users’ perceptions, most of them (35;92.1%) reported experiencing benefits from their HM usage, while only three (7.9%) patients reported not experiencing any benefits or problems during their HM usage. Interestingly, no patient had consulted their physician before starting to take the HMs. The demographic characteristics of participants, together with their attitude and perceptions, are presented in Table 1. All the participants taking HMs in the study reported that they were taking HMs concurrently with their conventional medicines; the number of HMs taken by these participants ranged from one to seven. Thirteen (34.2%) patients had taken only one herb, while 11 patients (28.9%) reported the use of two HMs. Eight patients (21.1%) reported that they had taken three HMs, and six patients (15.8%) reported the use of up to seven HM products. Participants reported that they had taken olive leaf, green tea, cinnamon, black seeds, fenugreek, ginger, bitter gourd, mulberry leaf, ginseng panax, pomegranate, barley, caraway, coriander, cumin, flaxseed, garden cress seeds, garlic, grapefruit, okra, onion, and parsley. The most prescribed medication groups were antidiabetic drugs, antihypertensives, anti-coagulants, and anti-hyperlipidemia medications (72, 36, 28, 16, respectively).
Table 1:Participants’ characteristics and their attitudes and perceptions towards HMs.
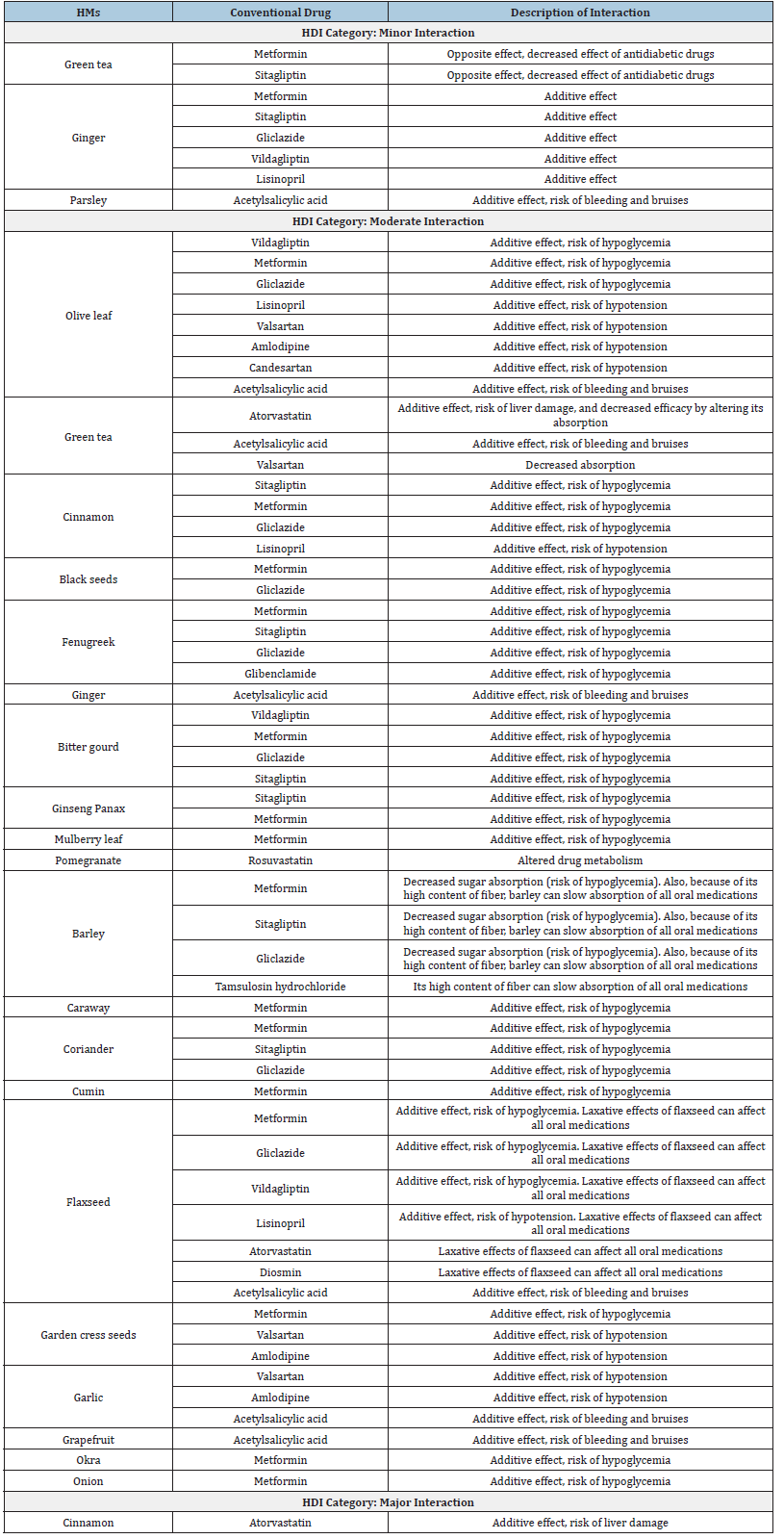
The numbers of patients reporting these, and other medications are given in Table 2. HM users were taking 21HM products concurrently with about 25 different conventional medicines, resulting in 130 herb-drug combinations. All of these combinations were screened to assess the risk of the potential interactions between the HMs and conventional medicines (HDIs). Most of the interactions (105; 80.8%) were assessed as “moderate interaction”, 24(18.4%) were categorized as “minor interaction”, and only one (0.8%) interaction was categorized as a “major interaction”. The most frequently taken HMs associated with some risks of interaction were olive leaf, green tea, cinnamon, and ginger (17.6%, 15.4%, 10.7%, 10%, respectively). The most frequently taken conventional medicines were metformin, atorvastatin, gliclazide, sitagliptin, acetylsalicylic acid, amlodipine, esomeprazole, candesartan, lisinopril, and rabeprazole. Table 3 list types of potential HDIs, as assessed and described by the study authors.
Table 2: HM products used concurrently with conventional drugs (herb-drug combinations).
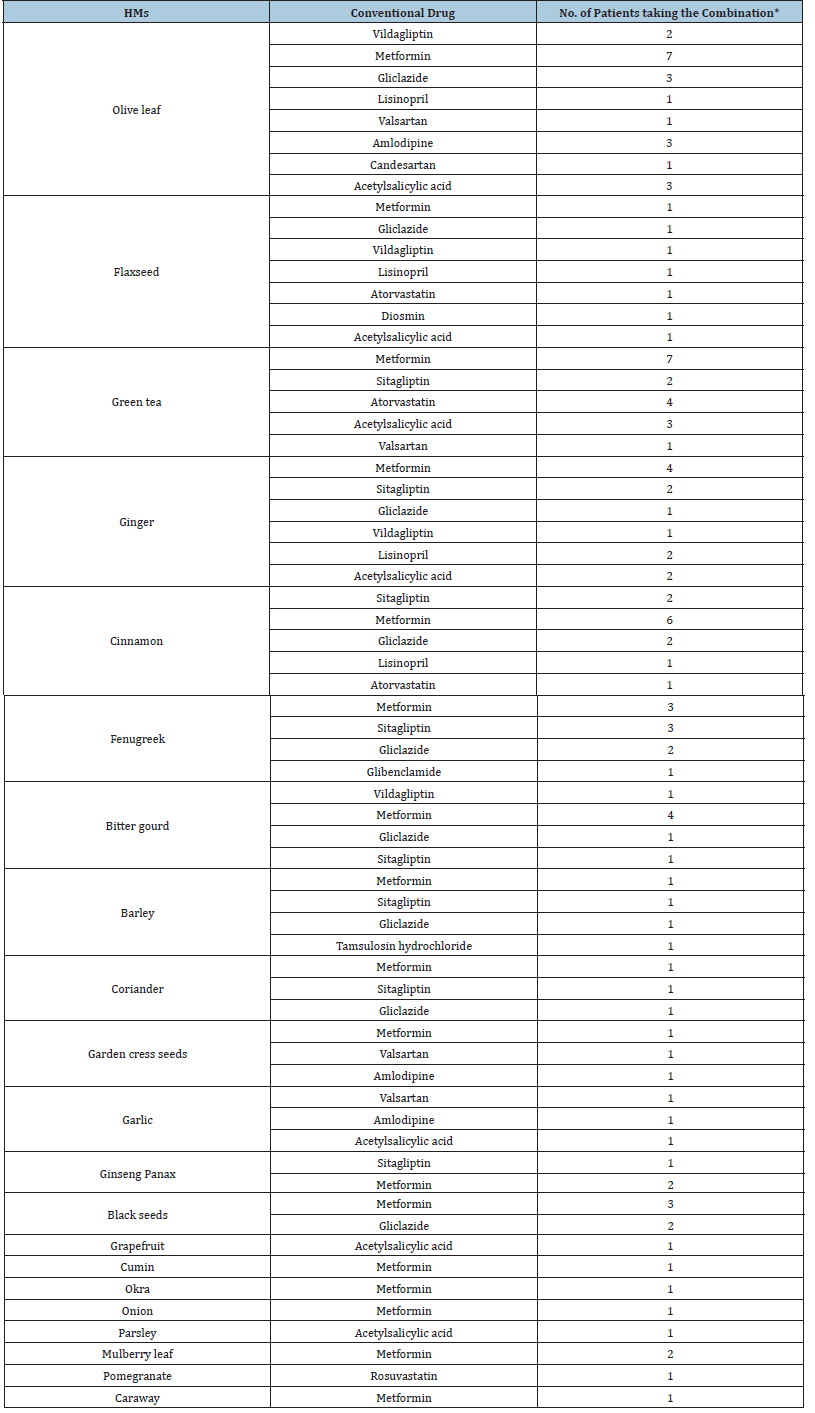
Table 3:Safety assessments of Herbal Medicine (HM)-conventional Drug Interactions (HDIs).
Discussion
More than 1,200 plants and compounds have been evaluated in the literature for their potential to treat type 2 diabetes, and over 400 of these have been shown to have some hypoglycemic properties. Most studies have highlighted that the following herbs are commonly taken by diabetic patients: cinnamon, fenugreek, garlic, aloe vera, and black seed [4,26,27]. Our findings are consistent with this since all these herbs were reported in our study. In addition, patients in Saudi Arabia strictly believe in religious therapy [28]. Therefore, certain HMs, such as olive oil, cinnamon, and black seeds, are commonly taken as a part of prophetic medicine; these herbs are prominently reflected in the study’s findings. Almost 65% of HM users in this study had taken two to seven herbal medicines concurrently with their conventional medicines, indicating high levels of potential HDIs. However, based on our HDI assessments, most of these interactions (80%) were categorized as “moderate interactions”, about 20% were “minor interactions”, and only one was assessed as a “major interaction”. It should be noted that these assessments were carried out retrospectively (i.e., when patients had already taken the herb-drug combinations); no ADEs had been reported and nor had any patient experienced problems. It has been reported that a variety of potential adverse HDIs have been proposed based on the pharmacological properties of herbal and conventional medications rather than their clinical outcomes [29]. Our assessments, therefore, highlight the gulf between theoretical and actual clinical interactions. In addition, although this kind of assessment does not measure the actual harms/benefits of HDIs, it does affirm the need to reconsider the methods used to assess herb safety and efficacy.
Another important issue in this regard is the disagreement between healthcare professionals, researchers, and herbalists on how the evidence concerning HM safety and efficacy should be gathered and interpreted. In other words, there is a strong demand for a framework that is appropriate for evaluating HM safety and efficacy at different levels of patient need, including in social, epidemiological, and clinical studies. Also, providing training and regular programs/courses for healthcare professionals in how to appropriately address HDIs remains essential. By solving such problems, clinicians will be able to confidently deal with HMs and their patients in this regard. Olive oil, cinnamon, and green tea were the most frequently reported HMs in the study with the same incidence of frequency (7; 33.3%). These herbs were responsible for almost 45% of all interactions. The second most commonly taken herbs were black seeds and fenugreek (5; 23.8%), followed by ginger (4;19%). Unlike other studies, aloe vera and garlic were not commonly reported in our study. From these results, it appears that diabetic patients are willing to use HMs. However, although some information is available regarding the most popular products taken by diabetic patients, little attention has been paid to any connection between HM types and diabetes diagnosis [30]. Certain herbs are perceived by patients to be useful for specific diabetes types; this might explain why aloe vera and garlic were not popular in our study since all participants were type II diabetes patients. Numerous preclinical experiments and clinical trials have shown a beneficial effect of olive preparations in type II diabetes. For example, a clinical study on 79 type II diabetes patients showed a significant reduction in HbA1c levels in those treated with olive leaf extract for 14 weeks [31].
Another clinical trial presented a significant decrease in fasting insulin levels in almost 90% of participants [32]. The potentiation of glucose-induced insulin release and increased peripheral uptake of glucose is suggested as the most likely mechanism of action [33]. A recent study on animals showed that olive leaf extract enhanced the antidiabetic effect of glibenclamide. Researchers suggested that the combination could cause an HDI through modulation of Insulin Receptor (INR), glucose transporter 2 (Slc2a2), and Peroxisome Proliferator-Activated Receptor a (PPAR-a) gene expression in the liver of diabetic rats [34]. However, olive leaves, oil, and extracts have nevertheless been widely used in traditional medicine in different cultures with no apparent harmful effects; and most of the HDIs of olive products are theoretical and based on evidence of pharmacological activity with uncertain clinical significance [33]. Reviews have demonstrated that cinnamon is the most frequently mentioned herb taken by diabetic patients [35]. However, it should be noted that a number of clinical and preclinical studies do not clearly distinguish between the various species of cinnamon, which may result in slightly conflicting data since the species differ slightly in phytochemical composition.
Overall, the evidence for blood sugar-lowering effects is positive but conflicting. It is considered unlikely that cinnamon, at standard therapeutic doses, would markedly affect the control of diabetes with conventional drugs [36]. A case report linked an incidence of acute hepatitis with this patient receiving “high dose” statin therapy [37]. Although the report did not provide details about the herb species, dosing, and pattern of use, coumarin (a constituent of Chinese cinnamon “cassia”) is known to cause liver and kidney damage at high concentrations [36-39]. In our study, a patient had taken cinnamon concurrently with atorvastatin; no ADE had been reported and the patient did not experience any harms. However, the potential HDI of this combination was assessed as a “major interaction”, and its usage should be discouraged. Certainly, the patient would not have been advised to use this combination during a consultation.
Interestingly, green tea was commonly used among the study participants although it is not, clinically or even traditionally, supported as an antidiabetic herb. Green tea and its preparations have been widely used to treat a number of conditions, mainly weight loss, cognitive improvement, bone mineralization, and the prevention of degenerative diseases such as cancer and cardiovascular diseases. However, there is a limited evidence base for most of these indications and further clinical studies are warranted [36]. It has been reported that green tea decreases the plasma level of statins (drugs usually prescribed for diabetic patients) through an unexplained mechanism [40]. However, green tea is considered to be safe since it is consumed by a large number of people without notable ill-effects, although the safety of high doses of concentrated extracts has not been confirmed [33]. The second most popular group of herbs used were black seeds, fenugreek, and ginger. Fenugreek is a traditional herb that has been used for thousands of years and is known for its hypoglycemic and hypocholesterolemic activity. Various studies have reported the benefits and wide safety margin of fenugreek [41].
Black seed is a traditional herb that was used to treat several ailments, including diabetes, by the ancient Egyptians and Greeks. A recent review has shown that reliable clinical and animal studies have demonstrated the antidiabetic efficacy of black seeds; suggesting that black seeds could be used as an effective adjuvant therapy with conventional antidiabetic drugs in diabetes control [42]. Ginger is a traditional herb that has been used for more than 2,500 years. It has been suggested that consuming 3 grams of ginger for eight weeks may be beneficial for diabetic patients and may lower both fasting blood sugar and glycosylated hemoglobin [43]. Notably, there is plausible evidence suggesting that most of the HMs taken by diabetic patients have antidiabetic properties. Using these HMs concurrently with conventional antidiabetic drugs is associated with enhancement effects. These enhancement effects may lead to hypoglycemia, meaning there is a high likelihood of adverse events. In addition, an increasing number of studies showed that genetic variations may involve the pharmacokinetic or pharmacodynamic pathways to affect HDIs; hence, monitoring is necessary [44,45].
Physicians, healthcare professionals, and patients should pay attention to these concerns and caution should always be applied. Furthermore, these HMs may interact with other non antidiabetic conventional drugs. For example, it is claimed that ginger and garlic (commonly used herbs) should not be used with anticoagulant drugs since they have antiplatelet effects [43,46]. Although these interactions have not been clinically confirmed, there is still an expected possibility of interactions; consequently, regular monitoring should be practiced. It is clear that diabetic patients have high expectations of HMs [47]. Our study confirmed this perception as most of the patients expressed positive feelings and experiences regarding HM use. They believed their HMs helped them. Some patients were certain that some HMs were “better” than conventional medicine and helped them control their diabetes. Although there is fairly good evidence for the use of some HMs, others do not have supporting evidence for use in diabetes treatment, contrary to what patients believed.
The source from which patients obtain their HMs may determine the quality and even safety of these products. Herbal shops in Saudi Arabia sell products as raw materials and extracts. However, there are few quality standards for herbal products. A study was conducted to assess the quality of herbal remedies present in the market in Saudi Arabia, taking into consideration safety concerns. Researchers showed that the patients used herbal remedies indiscriminately. They suggested that there is an urgent need to control the production, import, and sale of herbal preparations [48]. This study relied on a patient-centered method to obtain factual and holistic information about patients’ use of HMs alongside their conventional medicines. However, it is difficult to draw firm conclusions about the benefits or harms of HMs using question-based studies, especially when the methods of measuring the harm and effectiveness of HMs are highly controversial. In addition, the sample size of patients included in the study could affect the study’s generalizability. Nevertheless, these studies are a necessary preliminary phase for further sociological, preclinical, and clinical investigations and provide information about patients’ motives, expectations, and experiences of HM use.
Conclusion
This study revealed the high expectations of diabetic patients regarding taking HMs to manage their disease. Although the sample size of the study was not sufficient, 130 herb-drug combinations were identified. Some patients reported taking seven HMs concurrently with their conventional drugs. No adverse effects or harm were reported, but the possibility of adverse HDIs remains. However, based on the available evidence, most of the HDI assessments of interactions were categorized as “moderate interactions” and one was a “major interaction”. These assessments indicate the intrinsic need to reconsider the methods used to evaluate the safety and efficacy of HMs in a clinically significant matter. This would closely reflect the actual risk which patients may face. It will help physicians and healthcare professionals to provide sensible advice to patients, based upon documented evidence. Given that HM use is so common among patients, physicians and healthcare professionals have to pay attention to patients’ needs, in particular their psychological and spiritual needs. They should focus on the patient-doctor relationship and understand the patient’s perspective. Patients want to regain some control and enhance their quality of life rather than just focusing on physiological outcomes. Accordingly, ensuring the safety of HMs among this vulnerable group is a priority and appropriate recommendations need to be made.
References
- Medagama AB, Bandara R, Abeysekera RA, Imbulpitiya B, Pushpakumari T (2014) Use of Complementary and Alternative Medicines (CAMs) among type 2 diabetes patients in Sri Lanka: A cross sectional survey. BMC Complement Altern Med 14: 1-5.
- Chang HY, Wallis M, Tiralongo E (2007) Use of complementary and alternative medicine among people living with diabetes: literature review. J Adv Nurs 58(4): 307-319.
- Alsanad SM, Aboushanab T, Khalil M, Alkhamees OA (2018) A descriptive review of the prevalence and usage of traditional and complementary medicine among Saudi diabetic patients. Scientifica (Cairo) 2018: 6303190.
- Alzahrani AS, Price MJ, Greenfield SM, Paudyal V (2021) Global prevalence and types of complementary and alternative medicines use amongst adults with diabetes: Systematic review and meta-analysis. Eur J Clin Pharmacol 77(9): 1259-1274.
- Sheikhrabori A, Dehghan M, Ghaedi F, Khademi GR (2017) Complementary and alternative medicine usage and its determinant factors among diabetic patients: An Iranian case. J Evid Based Complementary Altern Med 22(3): 449-454.
- Alghamdi M, Mohammed AA, Alfahaid F, Albshabshe A (2018) Herbal medicine use by Saudi patients with chronic diseases: A cross-sectional study (experience from Southern Region of Saudi Arabia). J Health Specialties 6(2): 77-86.
- Alrowais NA, Alyousefi NA (2017) The prevalence extent of Complementary and Alternative Medicine (CAM) use among Saudis. Saudi Pharm J 25(3): 306-318.
- El-Olemy AT, Aboushanab TS, Alqaed MS (2020) Knowledge, attitude and practice of Saudi citizens towards complementary and traditional medicine. Health Educ Care 5: 1-5.
- Abuelgasim KA, Alsharhan Y, Alenzi T, Alhazzani A, Ali YZ, et al. (2018) The use of complementary and alternative medicine by patients with cancer: A cross-sectional survey in Saudi Arabia. BMC Complement Altern Med 18(1): 88.
- AlAnizy L, AlMatham K, Al Basheer A, AlFayyad I (2020) Complementary and alternative medicine practice among Saudi patients with chronic kidney disease: A cross-sectional study. Int J Nephrol Renovasc Dis 13: 11-18.
- Shaikh S (2021) Traditional medicine and its use for pain management in Saudi Arabia. Handbook of Healthcare in the Arab World (1st), Springer Publishers, USA, pp. 2057-2085.
- Wuthaynani FSA, Salmi AOA, Shehri AKA, Talhi EHA, Farag SF (2020) Prevalence of using aromatic and medicinal plants in the treatment of gastrointestinal tract diseases in al-Taif city, kingdom of Saudi Arabia. J Adv Med Med Res 32(9): 45-60.
- Almogbel ES, AlHotan FM, AlMohaimeed YA, Aldhuwayhi MI, AlQahtani SW, et al. (2022) Habits, traditions, and beliefs associated with the use of complementary and alternative medicine among diabetic patients in al-Qassim region, Saudi Arabia. Cureus 14(12): e33157.
- Abdullah RI, Allah AA, Mubarak AS, Abdullah RI, Alzhrani SH, et al. (2020) Prevalence and predictors of using complementary and alternative medicine among diabetic patients in Taif city, Saudi Arabia. J Family Med Prim Care 9(4): 2092-2098.
- Alqathama A, Alluhiabi G, Baghdadi H, Aljahani L, Khan O, et al. (2020) Herbal medicine from the perspective of type II diabetic patients and physicians: What is the relationship? BMC Complement Med Ther 20(1): 1-9.
- Kamel FO, Magadmi RM, Hagras MM, Magadmi B, AlAhmad RA (2017) Knowledge, attitude, and beliefs toward traditional herbal medicine use among diabetics in Jeddah Saudi Arabia. Complement Ther Clin Pract 29: 207-212.
- Al-Garni AM, Al-Raddadi RM, Al-Amri TA (2017) Patterns and determinants of complementary and alternative medicine use among type 2 diabetic patients in a diabetic center in Saudi Arabia: herbal alternative use in type 2 diabetes. J Fundam Appl Sci 9: 1738-1748.
- Alsanad SM, Williamson EM, Howard RL (2014) Cancer patients at risk of herb/food supplement-drug interactions: A systematic review. Phytother Res 28(12): 1749-1755.
- Alsanad SM, Howard RL, Williamson EM (2016) An assessment of the impact of herb-drug combinations used by cancer patients. BMC Complement Altern Med 16(1): 393.
- Baxter K, Driver S, Williamson E (2013) Stockley's herbal medicines interactions (2nd), Pharmaceutical Press, UK.
- Gupta RC, Chang D, Nammi S, Bensoussan A, Bilinski K, et al. (2017) Interactions between antidiabetic drugs and herbs: An overview of mechanisms of action and clinical implications. Diabetol Metab Syndr 9(1): 59.
- Thikekar AK, Thomas AB, Chitlange SS (2021) Herb‐drug interactions in diabetes mellitus: A review based on pre‐clinical and clinical data. Phytother Res 35(9): 4763-4781.
- Ly J, Percy L, Dhanani S (2002) Use of dietary supplements and their interactions with prescription drugs in the elderly. Am J Health Syst Pharm 59(18): 1759-1762.
- Peng CC, Glassman PA, Trilli LE, Hayes-Hunter J, Good CB (2004) Incidence and severity of potential drug–dietary supplement interactions in primary care patients: An exploratory study of 2 outpatient practices. Arch Intern Med 164(6): 630-636.
- (2022) The Natural Medicines Comprehensive Database.
- Chang CL, Lin Y, Bartolome AP, Chen YC, Chiu SC, et al. (2013) Herbal therapies for type 2 diabetes mellitus: Chemistry, biology, and potential application of selected plants and compounds. Evid Based Complement Alternat Med 2013: 378657.
- Mishra R, Shuaib M, Mishra PS (2011) A review on herbal antidiabetic drugs (2000-2010). J Appl Pharm Sci 1(6): 235-237.
- Qureshi NA, Khalil AA, Alsanad SM (2020) Spiritual and religious healing practices: some reflections from Saudi national center for complementary and alternative medicine, Riyadh. J Relig Health 59(2): 845-869.
- Bush TM, Rayburn KS, Holloway SW, Sanchez-Yamamoto DS, Allen BL, et al. (2007) Adverse interactions between herbal and dietary substances and prescription medications: A clinical survey. Altern Ther Health Med 13(2): 30-35.
- Harris PE, Cooper KL, Relton C, Thomas KJ (2012) Prevalence of Complementary And Alternative Medicine (CAM) use by the general population: A systematic review and update. Int J Clin Pract 66(10): 924-939.
- Wainstein J, Ganz T, Boaz M, Dayan YB, Dolev E, et al. (2012) Olive leaf extract as a hypoglycemic agent in both human diabetic subjects and in rats. J Med Food 15(7): 605-610.
- Rigacci S, Guidotti V, Bucciantini M, Parri M, Nediani C, et al. (2010) Oleuropein aglycon prevents cytotoxic amyloid aggregation of human amylin. J Nutr Biochem 21(8): 726-735.
- Braun L, Cohen M (2015) Herbs and natural supplements: An evidence-based guide (2nd), Elsevier Health Sciences, Australia.
- Abdel-Kader MS, Soliman GA, Abdel-Rahman RF, Saeedan AS, Abd-Elsalam RM, et al. (2019) Effect of olive leaves extract on the antidiabetic effect of glyburide for possible herb-drug interaction. Saudi Pharm J 27(8): 1182-1195.
- Allen RW, Schwartzman E, Baker WL, Coleman CI, Phung OJ (2013) Cinnamon use in type 2 diabetes: An updated systematic review and meta-analysis. Ann Fam Med 11(5): 452-459.
- Edwards SE, Costa Rocha I, Williamson EM, Heinrich M (2015) Phytopharmacy: An evidence-based guide to herbal medicinal products (1st), John Wiley & Sons, UK.
- Brancheau D, Patel B, Zughaib M (2015) Do cinnamon supplements cause acute hepatitis? Am J Case Rep 16: 250-254.
- Abraham K, Wöhrlin F, Lindtner O, Heinemeyer G, Lampen A (2010) Toxicology and risk assessment of coumarin: focus on human data. Mol Nutr Food Res 54(2): 228-239.
- Ranasinghe P, Pigera S, Premakumara GA, Galappaththy P, Constantine GR, et al. (2013) Medicinal properties of ‘true’cinnamon (Cinnamomum zeylanicum): A systematic review. BMC Complement Altern Med 13: 275.
- Izzo AA (2012) Interactions between herbs and conventional drugs: Overview of the clinical data. Med Princ Pract 21(5): 404-428.
- Neha S, Anand K, Sunanda P (2019) Administration of fenugreek seed extract produces better effects in glibenclamide-induced inhibition in hepatic lipid peroxidation: An in vitro Chin J Integr Med 25(4): 278-284.
- Maideen NMP (2021) Antidiabetic activity of Nigella sativa (black seeds) and its active constituent (Thymoquinone): A review of human and experimental animal studies. Chonnam Med J 57(3): 169-175.
- Khosravi HM, Talaei B, Jalali BA, Najarzadeh A, Mozayan MR (2014) The effect of ginger powder supplementation on insulin resistance and glycemic indices in patients with type 2 diabetes: A randomized, double-blind, placebo-controlled trial. Complement Ther Med 22(1): 9-16.
- Martins IJ (2018) Single gene inactivation with implications to diabetes and multiple organ dysfunction syndrome. J Clin Epigenet 3(3): 24.
- Liu MZ, Zhang YL, Zeng MZ, He FZ, Luo ZY, et al. (2015) Pharmacogenomics and herb-drug interactions: Merge of future and tradition. Evid Based Complementary Altern Med.
- Rehman SU, Choi MS, Choe K, Yoo HH (2015) Interactions between herbs and antidiabetics: an overview of the mechanisms, evidence, importance, and management. Arch Pharm Res 38(7): 1281-1298.
- Ezuruike U, Prieto JM (2016) Assessment of potential herb-drug interactions among Nigerian adults with type-2 diabetes. Front Pharmacol 7: 248.
- Bogusz MJ, Al Tufail M, Hassan H (2002) How natural are ‘natural herbal remedies’? A Saudi perspective. Adverse Drug React Toxicol Rev 21(4): 219-229.
© 2023 Saud M Alsanad. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






