- Submissions

Full Text
Advances in Complementary & Alternative medicine
Patient Communication: Lessons from Covid
Meg Jordan*
Professor of Integrative Health, California Institute of Integral Studies, San Francisco, USA
*Corresponding author: Meg Jordan, PhD, RN, Professor of Integrative Health, California Institute of Integral Studies, 1453 Mission, San Francisco, USA
Submission: April 06, 2022;Published: July 05, 2022

ISSN: 2637-7802 Volume 7 Issue 2
Abstract
The pandemic has offered many unexpected lessons besides the obvious one of needing to augment essential worker preparedness and address urgent supply chain dilemmas throughout national and local public health organizations. One of the most unexpected and valuable lessons was in the realm of patient communication. This article offers lessons and insights from front-line public health nurses who adopted novel approaches in patient communication to address problems with patient compliance regarding masking, physical distancing and receiving vaccinations.
Keywords:Patient communication; Health communications; Patient compliance; Adherence; Autonomy; Intrinsic motivation; Strengths-based counseling
Introduction
A surprising refusal to receive new SARS-CoV2 vaccines, often among the most vulnerable or marginalized populations, spurred a general questioning among some health care professionals about how we talk with our patients. Urgently addressing the need for physical distancing, wearing masks, self-isolating when exposed to individuals with COVID-19, getting vaccinated and boosted were all crucial risk-reducing and potentially life-saving communications. Adopting novel approaches and a reevaluation of customary ways to convince or influence patients was necessary for many front-line public health nurses in this recent pandemic. The following strategies are offered as a means to strengthen transparency and effectiveness in patient communication while taking a holistic approach to meet the health and well-being needs of patients, especially during times of crisis and widespread trauma.
First: Trauma-Informed Counseling
Just as health professionals learn the A, B, Cs of basic life support which put into place a triage protocol for assessing safety, consciousness, breathing, and circulation, there should be communication protocols health care professionals such as nurses, doctors, paramedics, and emergency department personnel follow in the midst of crisis. The widespread impact that initial high-mortality and morbidity from the SARS-CoV-2 pandemic had on communities resulted in a collective shock. There was ongoing insecurity, fear, grief and then a new reality of post-traumatic stress. For essential workers and front-line health care professionals, that collective shock was sometimes delayed due to the urgent nature of their work and the automaticity of their responses. However, the sense of grief and pain does eventually emerge, and people need to talk through the process, and feel grounded and centered again, which is all part of self-regulation of the hyper-aroused sympathetic branch of the autonomic nervous system. Some individuals are better attuned to the need for processing distressing emotions with others in their immediate circles; while others resort to separating, isolating and growing numb or denying the new reality. Likewise, some societies and cultures are better skilled at the need for connecting, sensing and feeling their way through grief and trauma, and have a heritage of dealing with pain and grief as a collective. Some South American cultures and Pacific Island ethnic groups have a tradition of public lament, which is a collective response to either tyranny, injustice, or inescapable violence or illness. Modernity and the encroachment of monoculture mores and values (secularization, commercialization, globalization) has largely eliminated this rather old-world response from highly developed nations. As a result, individuals are forced to confront the pain and horror of cataclysmic events alone, and the sheer force of responding with others in a public lament of tears, groans and cries fails to awaken each other to the power of solidarity to also recover and heal together.
Exploring feelings with a distressed patient is a core skill for
health care professionals and should not be regarded as a special
skill available to only to mental health, counseling or psychotherapy
practices. In instances of trauma or crisis, much of the emergency
medicine literature suggests attending to the physical needs of
individuals first, and then referring to mental health counselors
at a more appropriate time. This paper proposes that the reports
from front-line workers during this pandemic invites an alternative
solution that has the potential for handling negative or distressing
emotions upfront and moving overwhelm to emotion regulation
in a more effective and holistic manner. The emotional climate
inventory proposed consists of these triage steps:
a. Obtain the individual’s view of the current reality (ask
them to describe in brief terms their experience). This will allow
the health care provider to assess their capacity to address
what is of immediate concern, versus what is important but not
necessarily urgent.
b. Listen with empathy, for the degree of emotional
awareness and emotional intelligence exhibited by the
individual.
c. Attend to cultural variation (an understanding of
life’s trauma from a cultural viewpoint, which may enhance
emotional intelligence or thwart it) and respond with cultural
humility and sensitivity.
d. Attempt to reduce the high levels of emotional arousal
with the use of paraphrasing and reflecting back not just intense
feelings expressed by the individual, but also by affirming their
core strengths of resilience and grit and survivability.
e. Pay close attention to expressions of loneliness or a
sense of “not belonging anywhere” and arrange for ongoing
connection with caring support and
f. Keep emotionally exhausted or physically spent
individuals close by and under close supervision, watching
for signs of shock. Expressions of depersonalization and
detachment are additional warning signs; and these individuals
should be monitored with close contact as well and not be left
alone.
g. The remainder of this commentary goes into details on
specific tasks and skills that would enable this emotional triage
and ensuing actions to manifest. (I will use the term “nurse”, but
all health care professionals are invited to consider enhancing
these communication skills.)
Increase Positive Psychological Resources
The nurse helps the patient develop positive psychological resources by cultivating meaning, reflecting positive emotions, applying strengths, and affirming self-worth and efforts. Nurses should emphasize the value of positive resources in improving creativity, open-mindedness, strategic thinking, resilience, connection, and health. Nurses can role model positive emotions of gratitude and hopefulness as a means to optimism and resilience. Emphasizing strengths, even in the face of a crisis, has been shown to be instrumental in mustering resilience. A strengths-based approach is a fundamental part of the patient communication process-some experienced health care professionals, especially nurses, would argue that it is the essential backbone of the advising process. Awareness of signature strengths is critical for the development of self-efficacy for patients who lack the confidence to pursue their health goals [1]. The following tools can all be employed in assisting a patient to develop both presence and for cultivating a greater access to their strengths. Strengths-based approaches permeate much of the positive psychology field. Strengths-based counseling methods focus on a core of inherent and growing strengths or valuable capacities within individuals. A valid means for discovering the strengths that are specific to character-building is offered by the Gallup Clifton StrengthsFinder. Those traits include greater levels of wisdom, courage, humanity, justice, temperance and transcendence-all important traits that were exhibited during various surges of the pandemic. You can identify your personal character strengths-and assist your patient in identifying their own-by taking the online questionnaire at the website. The profile was developed from more than 1.3 million individuals worldwide (in 17 languages) completing measurements that scientifically investigated a person’s character strengths [2]. Talking about one’s strengths is a phrase often heard in counseling. It requires that both you and the patient take an inventory of those strengths, with the nurse serving as a memory jogger helping the patient remember their strengths when they most need to draw upon them during the difficult path of dropping unwanted habits or committing to a new course of action. When patients talk in disparaging ways about their lack of progress, the nurse can help them shift their perspective in the moment by reframing and refocusing on their strengths instead of their limitations or weaknesses. By discovering their talents, patients can have an “ah-ha!” moment within the communication session and enjoy leading with their strengths instead of pointing out their shortcomings. A growing body of research shows how a strengths-based approach is essential to building confidence and moving forward in multiple domains. When used in the pursuit of physical activity and exercise for families, a strengths-based approach focuses on a healthy orientation to body image and overall wellness [3]. Strengths-based approaches permeate much of the positive psychology field. There are strengths-based counseling methods that focus on a core of inherent and growing strengths or valuable capacities within individuals. Much of the scientific work on strengths that are specific to character-building was originall done by the VIA Institute on Character. Those traits include greater levels of wisdom, courage, humanity, justice, temperance, and transcendence. Nurses can identify their personal character strengths-and assist your patient in identifying their own-by taking the VIA Character Strengths Survey at the website. The survey was developed from more than 1.3 million individuals worldwide (in 17 languages) completing measurements that scientifically investigated a person’s character strengths. The VIA Survey for Adults and Survey for Youth take about 30-40 minutes to complete. Again, it requires that both you and the patient take an inventory of those strengths and draw upon them during the difficult path of adopting a new course of action, such as modifying behavior in the face of a newly diagnoses chronic illness. Research on 622 adults placed into either one of nine character-strengths interventions or a placebo group discovered that happiness can be enhanced (and depression somewhat alleviated) with simple activities such as gratitude visits or remembering three good things for a two-week period [4]. Pre- and post-testing at 1, 3, and 6 months confirmed that eight of the nine interventions increased happiness, while depression was decreased in all groups, including the placebo. While happiness may be too difficult an achievement during times of critical health crisis, contentment or a sense of well-being is most helpful. The VIA Institute of Character reports that five VIA character strengths most related to life satisfaction are hope, zest, gratitude, curiosity, and love. The following activities are recommended by the Institute as a means for discovering the link between happiness and strength-building. Nurses could practice these activities are on their own before trying them with patients. Assisting patients in the discovery, exploration, and practice of strengths not only cultivates positive self-regard but opens the realm of more positive cognitions and feelings.
Activity to boost hope
Take a moment to think about the upcoming year and imagine your best possible self-coming forward. You are engaging in activities that are pleasing and you are working toward goals that are important to you. After you get a clear image, write out the details. Writing about your best possible self helps to create a logical structure for the future and can help you move from the realm of foggy ideas to concrete, real possibilities.
Activity to boost zest
Get active! Engaging in physical exercise has been shown to increase energy levels and improve endurance. All you need is 30 minutes a day and you will notice a difference in your spirit and vitality. Pick a physical activity that sounds fun to you, such as iceskating, hiking, touch football, skiing, etc. and do it! You will be boosting your strength of zest AND improving your physical and psychological wellness.
Activity to boost gratitude
Schedule a gratitude visit. Think of a person to whom you are very grateful, but you have not properly thanked. Reflect on how you have positively benefited from their actions and then write them a letter expressing your gratitude. Call the person on the phone or arrange to meet them in person and read the letter aloud to them. The experience will be rewarding for you and the other person!
Activity to boost curiosity
Think of an activity you dislike, such as washing dishes, paying bills, or folding laundry. Next time you are engaging in the unpopular activity focus on three novel or unexpected features of the action. For instance, if your low-interest activity is dishwashing, focus on the smell of the soap, the heaviness of the pot, and the warmth of the sudsy water. Can you find one thing surprising about this humdrum activity?
Activity to boost love
Engage in loving-kindness meditation. Find a comfortable space to sit quietly and practice wishing yourself and others happiness and peace. Maybe you decide to recite phrases of contentment and good fortune, such as “may I be strong and healthy” or “may my sister find happiness and love.” This type of meditation can make us feel more connected to others around us and increase the VIA character strength of love.
Support Freedom of Choice, Autonomy and Intrinsic Motivation
Effective communication involves eliciting the patient’s
intrinsic motivation, which is based on the patient’s purpose,
meaning, values, and preferences and not on external sources. The
knowledge and experience of the patient-not the nurse-are the raw
materials for conversations that facilitate lasting change.
a. Elicit the patient’s perspectives (including reasons for
change, solutions, ideas, experiments, desires, reactions,
desired outcomes, rewards/incentives)
b. Help patients explore and articulate values, sense of
meaning, and purpose
c. Help patients envision their optimal health and/or wellbeing
d. Discuss and honor patient’s preferences for selfmonitoring
(without judgment), accountability, mode of
connecting (email, text, phone call)
e. Apply Self-Determination Theory to discuss autonomy,
competence, and connection [5].
f. Employ Motivational Interviewing techniques to address
ambivalence.
g. Explore Patient Self-Efficacy
h. The nurse helps the patient develop self-efficacy, which is
the patient’s belief in their ability to initiate change, overcome
adversity, and achieve goals by gaining self-awareness and
insight that supports behavior change, learning from setbacks,
developing new resources, and finding new ways to navigate
their environments. Nurses help patients engage in problem solving, evaluate options, and consider short and long-term
benefits and consequences.
Improve Support
Change is too hard to go it alone. Support comes in many
forms, and nurses can open those possibilities to the patients who
may have struggled for a long time in solo fashion. What are the
connections and ties that allow the patient to feel that support and
benefit from it? Do they need to learn how to ask for help? This
is common. What other obstacles or barriers might be in the way?
How can nurses assist in the activity of sourcing? Think about
support in three ways:
a. Social support: friends, allies, relationships, family,
coworkers, mentors
b. Internal support: personal skills, strengths, values,
competencies
c. Structural/environmental support: safe, comfortable
residences, vital neighborhoods, recreational opportunities,
affordable transportation, healthy workplaces.
Inspire Active Experimentation and Self-Discovery
The nurse establishes a trusting environment where the patient feels safe to experiment with new ideas and new behaviors. This experimentation can happen in the advising session or anytime on their own. The nurse helps the patient develop a growth mindset, the belief that the patient’s abilities are not fixed and can be improved continuously through experimentation and persistent efforts. Decisional balance helps the patient evaluate pros and cons of changing behavior, as well as pros and cons of not changing behavior. The nurse can tally the pros and cons as was often done when assessing the benefits of risks of receiving a vaccine against COVID-19.
Connect to Values
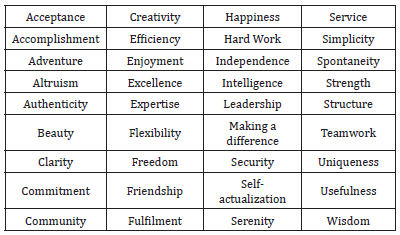
Our values run us. Everyone works from a set of values, whether those values are consciously identified or not. If one values competence over social connection, one tends to seek recognition for talents or can feel humiliated by comments that another may just disregard. If an individual values efficiency and organization, they may want to work independently and quietly and find highly sociable types annoying. Our values also determine what goals we want to achieve in life. During the communication session, nurses will get a sense of their patient’s goals just by what they deem important and what they want to avoid. Nurses can ask them directly what they value, or just take a chance and offer a guess now and then as they get to know patients better. It’s not that hard to decipher someone’s values but one can be surprised now and then, so it’s best to ask them to identify values from a list, such as the following (partial) values list (Table 1). Communicate according to the patient’s, not one’s own. This might be one of the most significant insights from the pandemic. Make that distinction and don’t assume patients share your values. Also, as nurses practice these techniques and increase self-awareness, they can catch themselves if they ever project (attribute your motives, feelings, or thoughts to someone else) their values onto others. Projection is studied extensively in psychotherapy, along with transference and countertransference. These are psychological terms that denote a clouding and blurring of therapeutic relationships, due to crossing over lines of individual wants and desires.
Table 1:Partial values list.
Advance your Skill in Asking Evocative Questions
Some of the best thinking on the art of posing evocative questions comes from Juanita Brown and David Isaacs, founders of the World Café, an organizational and communications firm. The following statements are inspired from his co-authored book, The Art of Powerful Questions: Catalyzing Insight, Innovation, and Action (Isaacs, Vogt & Brown, 2003). Asking evocative, powerful questions fosters breakthrough thinking, creativity, innovation, and action. In Germany, the job title director grundsatzfragen translates as “director of fundamental questions” and reveals the high value placed on ongoing conversations that penetrate the current assumptions and prepare for a next paradigm. The aversion in many cultures to asking creative questions is linked to an emphasis on finding quick fixes and an attachment to black/white, either/or thinking. The authors believe that North American cultures focus on having the right answer rather than discovering the right question, while other societies throughout Asia might find the process of powerful questioning to be intrusive or disrespectful. A great deal of tact and patience is required to learn this artful skill, along with culturally adapative sensitivity.
Rate the following questions according to their ability to stir
innovation and action:
a. What’s the temperature out?
b. Did you take the dog out?
c. What’s the possibility you see in this situation?
d. How could you best manage your work/life balance?
Questions 1 and 2 elicit simple yes/no responses and are
viewed as less powerful than questions 3 and 4. Powerful questions
will:
i. Meet people where they are but stretch them, transcend
their present boundaries.
ii. Reveal hidden assumptions that act as outdated barriers
and unwanted limitations.
iii. Have tremendous energy, allowing people to find meaning
and relevance.
iv. Create possibility-oriented responses and further
conversations.
v. Shift the conversation away from a problem to a
possibility/focus.
vi. Generate curiosity in the listener.
vii. Stimulate reflection and refuel purpose and meaning.
viii. Be thought-provoking.
ix. Invite creativity.
x. focus attention and inquiry.
xi. Stay with you, linger.
xii. Evoke more questions.
Gain Skill in Tracking
Are you able to track a patient’s story? In times of extreme stress, the communication is scattered and neither delivered well nor received accurately. When a nurse’s practice listening attentively, the most salient, important parts stand out, and nurses are prepared to ask evocative questions about that particular piece. I am talking about evocative, powerful questions that arise because you are doing a skillful job of tracking your patient’s tale, no matter how many twists and turns. That is when you come up with the most helpful questions in the supportive conversation, and they are for your patient, not for you. Whenever you find yourself just digging away at underlying causes or tangential information, stop yourself, and think, “Is this really essential for me to know-or am I just being nosy?” There is a big difference between practicing curiosity to help the patient come into greater clarity, and a perverse probing away for no good reason. The line of questioning needs to stay clean, honest, purposeful and direct. The intent of evocative questions is to assist the patient in discovering more about themselves and their inner process, especially where it may lead them astray. A powerful question can help them discover something deeper about their thought process. Tracking is all about staying alert as they talk. Yes, it takes practice.
Interrupt and Redirect
In a stressful environment or critical health time, nurses will need to redirect their patient back to the topic at hand. Sometimes a story the patient is telling has taken some off-subject detours. A nurse can find it difficult to hold the drift of what the patient even started to talk about. They’re on a long-winded repeat story and you’re frankly lost. Just tell the truth: Pause please … I’m lost. We started out talking about how you were going to go about seeking that a new home health aide, and then we fell off topic. I’m here to help you stay on track, as we agreed.”
Reframe
Is there another way to see things? Yes, always. Whether or not we want to-that’s another matter. When your patient is entrenched in being right, even at the sake of their own health and happiness, it’s time to help them reframe the situation and seek another perspective or way of regarding the problem. Paraphrase and reflect back what you heard before asking a patient to reframe. Be sure to seek clarity and to acknowledge, restate, and confirm that the reframing is accurate. Use the session to experiment with reframing attempts by the patient. They take practice. Skillful reframing can turn problems and negativity into opportunities for powerful growth and change.
Example:
Patient: “I am never going to get this blood sugar under control.
It’s impossible. I’m not sure what I can do.”
Nurse: “Your past attempts to manage it have not worked. You
are actively seeking another strategy. I can help with that.”
Work with Rising Emotions
I once heard a public health nurse say, “If strong feelings arise in a patient session, suggest that the patient see a therapist.” I’m never against seeing a therapist when someone wants to, but just because an individual expressed heightened emotion, doesn’t mean we have to shut down its expression and save it for the therapist. Psychotherapy hasn’t cornered the market on emotions. Nurses and patients express feelings (on some level) every day to intimates and strangers alike. Suppressing the feeling for later show-and-tell with a psychotherapist is rather nonsensical and could set up a pattern begetting emotional dishonesty and undelivered communications. Feelings show us what we’re thinking and point out intuitive flashes. Feelings such as unresolved grief or prolonged, disruptive anger or flashes of mean-spirited resentment-these are the types of feelings you may not want to deal with as a nurse and have every right in disclosing this to a patient. Suggest they take these deeper issues to a psychotherapist, but also do not shirk back from heightened negative emotions.
Use Intuition (Carefully)
While nurses are trained in evidence-based methodology, experienced health care personnel recognize that there will be times when nurses need to use their intuition and follow up on a hunch. It will feel like you’re taking a wild guess, and it may not be right. But it’s a valid way of requesting clarification. If you’re right, your patient will hopefully tell you. If you’re off, acknowledge that it was simply a hunch, and that you’re happy to be corrected. Also, don’t let a wrong guess throw you off. You will continually refine your intuitive skills as a nurse with more practice. There truly is a place for intuition when communicating with patients but proceed with caution.
Stretch into Unfamiliar Territory
What to do when it feels risky
Nurses can gain skill in knowing when to “stretch” their patients. This is a process of following the nonverbal cues and signals from the patient about when they might be ready to stretch beyond their comfort zones. This involves listening deeply to when it is appropriate to extend an effort or commitment beyond that place where the patient knowingly or unconsciously drifts back to-that safe place where behavior is routine. Your patient may be having an exacerbation of a chronic ailment and has now exhibited a readiness to get beyond their usual mindset and behavior. If they seem to be circling around that old familiar territory, it is probably time to invite a stretch.
As a nurse, you can help your patient approach this heightened
challenge with new awareness and new solutions. Consider small
initial steps through creative brainstorming and generate new
possibilities for action that lower this risky threshold.
a. Assess and explore an area that is a clear challenge or
stumbling block to progress.
b. Listen fully for the area of focus or inquiry
c. Summarize the essence of what you heard.
d. Ask the patient to generate a few new possibilities.
e. When appropriate, try the 10 Wild Ideas discussion. This
is a much more directive strategy for you as a nurse and will
seem at odds with your usual style of patient communication.
But these 10 Wild Ideas will serve to melt a blockade and open
up the patient’s thinking to the realm of all possibilities.
f. Focus on at least three possibilities (or two, no hard rules
here).
g. Try these “riskier propositions”-all meant to stretch.
i. Ask: Make a big request: You know this familiar
territory. What is life asking from you today? What change
could help make a big difference in your life?
ii. Identify a clear inconsistency: I hear you wanting this, but
doing that …
iii. Ask for a bigger truth: Tell the truth completely on this
one … is it really what you want?
iv. Point out a disheartened compromise: What inner
strength are you capable of, but ignored, as you compromised
on what you need or want here?
v. Try metaphors or imagery: Pretend you’re peeling back
the onion, what would you see? What’s closer to the center of
this issue for you?
vi. Offer an option (as a last resort): Is it okay if I offer you
some suggestions?
Foster Patient Independence
Professional nurses follow an ethical guideline to make sure patients do not become dependent on them by fostering patience independence and supporting self-autonomy from the onset of their managed care. Stringing along a patient just to assure financial livelihood is tantamount to an ethical and moral violation within any profession, from law to accounting, and from medicine to the behavioral sciences. Summarize the patient’s growth and change at regular intervals. Be realistic and not overindulgent. Tell the truth because it will be recognized. Nothing “rings true” like the truth. Patients appreciate when nurses document progress with graphic tools, celebratory markers, and success records. Patients often don’t have a sense of their achievements, therefore, creating milestones that mark and celebrate the success is respectful, vital, and fun. When a milestone or goal is not achieved due to unforeseen challenges, new hardships or difficulties, it is important to empathize with your patients. Setbacks are a normal part of life. Patients may feel that they do not have enough willpower to follow through with medical directives or nursing suggestions, therefore, it helps to teach them that a growth mindset is more important than a perfectionist attitude [4,6]. Always practice authenticity and honest reflection, with either successes or setbacks, and your patients will grow to trust your feedback because it will match their own inner compass. To overcome setbacks, revisit goals and honestly reflect on their appropriateness at this stage of the learning and growing process. This process can be strenuous, so be sure to support a wide variety of stress management skills (breath work, visualization, meditation, guided imagery, walks in nature, listening to music, massage, Therapeutic Touch) to assist patients.
Use Guided Imagery and Visualization
We can only achieve what we can first imagine. Facilitating the process of visualization with patients starts with some basic skills in guided imagery. Imagery is the first language of the brain. Before we have words as a baby, we converse in our minds with images, and continue to do so throughout our lives. Guided imagery is one of the most validated forms of alternative medicine, with scientific evidence supporting a wide variety of goal attainment, such as, pain management, stress reduction, accelerated recovery from surgery, weight loss, and smoking cessation. It is both appropriate and highly useful for nurses to employ guided imagery or simply visualization exercises within dedicated patient communication sessions. It requires a quiet space, however, and is not ideally suited for times of crisis. However, if the patient is accustomed to visualization techniques, they can often access a quick mental rehearsal to embolden their action in an emergency. But for the most part, visualization and guided imagery are most useful when creating an overall health and well-being vision or tapping into one’s life purpose.
Suggested visualization script (3-6 minutes)
In a safe room free of distractions or interruptions, and in a
comfortable chair (seated upright), guide your patient to do the
following:
I. Take a deep breath from your abdomen and slowly go
within, closing your eyes. Breathe in and out naturally at your
own pace. With every breath in, feel yourself grow more relaxed
and at ease. Let the tension fall easily out of your body with
every exhalation. With every inhalation, bring in more peace
and clarity and ease.
II. Keep breathing from the belly. Feel yourself relax more
with each breath. Good.
III. In your mind’s eye, go to a safe and comfortable place
where you feel all your needs are satisfied. You are safe,
protected, feel strong and secure. It’s a place where you feel
relaxed and confident.
IV. What does this special place look like? Feel free to put
anything you’d like there. The sky’s the limit. Your imagination
will serve all your needs.
V. Now fast-forward five years and grant yourself the picture
of perfect health. You’ve accomplished all your wellness goals.
How is your health? What would be the ideal image for a
healthy, fit, happy, healthy you, radiating with well-being? How
do you feel being there? What does this place look like now?
Notice what surrounds you. Take your time to imagine all the
details. Let all your senses be evoked.
VI. Describe how you feel. Imagine how you arrived at this
extraordinary place of well-being. What happened over the
past five years? What actions did you take? Who helped you get
there? What are you doing differently than you’re doing now?
VII. What does it feel like to be in that healthy, fit, happy, well
body and place?
VIII. Because of time, you’re going to say goodbye for now,
but you can always come back to this safe, strong, secure
place. Come up with an image that will symbolize and sum up
this experience. Hold onto that symbol. Put it somewhere for
safekeeping.
IX. As this session draws to an end, take a moment to scan
your body. Rub your hands together, place them over your eyes.
Wiggle your toes and get grounded. On the count of three, you
will open your eyes, feel alert yet calm, relaxed, and peaceful.
Next ask the patient the following questions. Give sufficient
time for them to come back:
a. How do you feel?
b. What happened? What can you share?
c. What symbol did you bring back with you?
d. What wellness vision can you craft from this?
Facilitate a discussion exploring all the qualities, strengths, friends, allies, resources, environmental settings, and unique gifts to support the lessons and insights.
Explore Parts
What do you do when your patient is blocked by false beliefs or disabling emotions? Here is a simple yet elegant way for nurses to do parts work without going down the rabbit hole of therapy or diagnosing or treating. Dialoguing with personality parts (thoughts, feelings, beliefs) within others and within yourself is a way of bringing clarity and spaciousness around emotions, honoring their presence, feeling heard, and moving on. When parts work is accompanied by somatic sensing, the patient can feel a shift and let go of some of the tightness, distress, and judgment that accompanied the emotion. Then the nurses have an opportunity to help the patient explore the validity of the belief or thought that was holding them back.
Example: A nurse notices that her patient is holding her breath, shrinking back and so the nurse asks about her state. How are you feeling right now? I sense a shift.
Patient: I’m too scared to see family again. I think I might have infected my grandparents. The test was negative, but I don’t trust anything anymore.
The patient’s fears may or may not be true, but effective patient communication is not about arguing with beliefs. Instead, the nurse sees a way forward by helping the patient separate emotions from beliefs. Instead of acknowledging that the patient is her fear, the nurse makes the distinction that this fear is a part of her, and there is much more to her whole being. She is also someone who can make good decisions and take charge.
Nurse: A part of you is worried and afraid of what could happen. I invite you to pause a second and sense where in your body you feel that and give it some space. (Pause. Big breaths invited.) And I also want to acknowledge the strong and protective parts of you that declared how you wanted to protect the health of your family and honor that part.
The nurse is acknowledging all the past work this patient has done, expressing motivation and deep concern. It is common for emotions, judgments, and beliefs to rise up and sabotage planned actions. A permission-granting, nonjudgmental discussion about one’s “parts” can often create a new spaciousness and willingness to adopt a new perspective and relieve anxiety. What I appreciate about parts work is how it allows internal shifts to occur naturally in a communication session. The nurse doesn’t have to analyze or make any assumptions about the internal process that the patient is undergoing. Just witnessing and honestly reflecting is enough. Nurses should not be afraid of working with emotions. When given a chance to be seen and heard, emotional blocks will more often than not will shift, dissipate, or release some underlying truth that points to whatever needs attention. Livingstone and [7] offer a 30-seond emotional first-aid for health professionals to work with their own emotions and thoughts (what they call “pop-ups”) that can get in the way of effective patient communication and dissemination of information. Here are the steps: When you notice you are feeling upset or distressed in the middle of a communicating with your patient, and your body is tight or uncomfortable, get curious about that sensation. Check if there is an emotion there or some thought present and then go toward it mentally with curiosity. Say to yourself that what you notice is probably coming from some personality part with you, not all of you. Breathe into what you notice and be with it in an internal relationship between you and a part of you-like a caring parent to a child. Check what you feel toward this part. If there are judgments or fears about it, ask those to soften so that you can just be with it. Befriend it and develop an intention to revisit the pop-up (emotion and thought) later in the day. Ask “What do you need from me right now to soften so I can focus on my patient? Honor the request if possible and promise to come back to this part later. Then refocus on the patient. In teaching this technique to thousands of nurses, I heard John Livingstone, MD, a Harvard-trained psychiatrist say, “Emotions just are beliefs are discussable; different sets of emotions and beliefs are held by the patient’s various personality parts, and vulnerable emotions activate protective parts.” Be sure to keep your promise and offer yourself that caring witness to this part of you later in the day when you are without patients. If you are interested in learning more about this effective and compassionate technique that is dedicated to self-care for clinicians and nurses, read Relationship Power in Health Care [7].
Summary
a. Employ positive psychology resources such as
emphasizing strengths, hope and optimism.
b. Support autonomous decision making and intrinsic
motivation.
c. Enhance support socially, internally and structurally
(environmentally).
d. Inspire a growth mindset and continuous learning and
discovery.
e. Connect to the patient’s values, not your own.
f. Improve your skills in asking evocative questions that
actually assist the patient’s insights and behavior change.
g. Track patients’ stories carefully and with nonjudgment
and curiosity.
h. Stretch your patient into a new behavior or mindset.
i. Assist patients to reframe using a new perspective
Practice basic skills in guided imagery and visualization.
j. Foster patient independence when appropriate.
k. Help patients distinguish between their emotions and
their beliefs by doing parts-work communication.
References
- Náfrádi L, Nakamoto K, Schulz PJ (2017) Is patient empowerment the key to promote adherence? A systematic review of the relationship between self-efficacy, health locus of control and medication adherence. PloS One 12(10): e0186458.
- Lavy S, Benish WM (2021) Character strengths as “Values in Action”: Linking character strengths with values theory – An exploratory study of the case of gratitude and self-transcendence. Front Psychol 12: 576189.
- Warburton D, Bredin S (2019) Health benefits of physical activity: A strengths-based J Clin Med 8(12): 2044.
- Mc Gonical K (2013) The willpower instinct: How self-control works, why it matters and what you can do to get more of it. Avery.
- Barley E, Lawson V (2016) Using health psychology to help patients: theories of behaviour change. Br J Nurs 25(16): 924-927.
- Baumeister RF (2012) Willpower: Rediscovering the greatest human strength.
- Livingstone JB, Gaffney J (2016) Relationship power in health care: Science of behavior change, decision making and clinician self-care. Routledge, UK.
- (2022) VIA Institute on Character. Bring your strengths to life & live more fully.
- Wennberg DE, Marr A, Lang L, O Malley S, Bennett G (2010) A randomized trial of a telephone care-management strategy. The N Engl J Med 363(13): 1245-1255.
© 2022 Meg Jordan. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






