- Submissions

Full Text
Advances in Complementary & Alternative medicine
Hypoparathyroidism Associated with Plaque Psoriasis-A Case Report
Alireza Rezayi1, Shadab Salehpour2, Fatemeh Kodaei1* and Maryam Saberi1*
1Skull Base Research Center, Shahid Beheshti University of Medical Sciences, Iran
2Department of Pediatric Endocrinology and Metabolism, Shahid Beheshti University of Medical Sciences, Iran
*Corresponding author:Fatemeh Khodaei, Skull Base Research Center, Loghman Hakim Hospital, Shahid Beheshti University of Medical Sciences, Iran
Submission: March 12, 2021;Published: March 30, 2021

ISSN: 2637-7802 Volume 6 Issue 3
Abstract
A 17-year-old Afghani male is described with hypoparathyroidism and plaque psoriasis associated with multiple intracranial calcifications. A diagnosis of hypoparathyroidism was made based on hypocalcaemia, hyperphosphatemia and low PTH level. A skin biopsy was compatible histopatholigically with psoriasis. He mentioned a listed problem consisted of frequent paroxysmal spells of generalized tonic-clonic seizures during the past ten years and a history of suffering from tingling and numbness of the extremities especially localized at the lower limbs, during the recent years. Also, he had frequently spontaneous episodes of invasive behaviors happened during the recent years seemed to be another manifestation of hypocalcemia due to hypoparathyroidism. Considerably, he had an unsuccessful history of phenobarbital therapy during the past years. At admission, positive trousseau and chvostek signs besides a prolonged QT interval obtained on ECG, revealed hypocalcemia, and confirmed by low serum calcium level. After initial treatment with calcium infusion, the maintenance therapy continued with calcium supplement and calcitriol. Surprisingly after serum calcium correction, the clinical condition improved, and the skin rash showed significant improvement.
Keywords: Hypoparathyroidism; Psoriasis; Hypocalcaemia; Intracranial calcifications
Introduction
Psoriasis, a common papulosquamous disease of the skin, affects about 1-3% of the population. Aetiopathogenesis of this dermatosis is complex and not yet well known. It involves the innate immune system (keratinocytes, dendritic cells, histiocytes, mastocytes, and endothelial cells) and acquired immune system (T lymphocytes). Once the innate immune system is activated, dendritic cells present an antigen (not yet defined) to lymphocytes [1]. Finally, a response is generated that leads to an expansion and activation of lymphocytes with a Th1/Th2 imbalance in favor of Th1 [2].
Intracellular calcium plays an important part in the regulation of proliferation and differentiation of keratinocytes [3]. Some cases of various forms of this skin disease have been found to show disturbances in systemic calcium metabolism [4]. The association of psoriasis with hypocalcemia has previously been described by several authors [5,6]. Para Thyroid Hormone (PTH) is one of the two major calciotropic hormones, the other being calcitriol, that regulate calcium and phosphate homeostasis [7].
Reportedly, hypoparathyroidism may cause the onset or aggravate psoriasis in patients with surgical hypoparathyroidism and primary hypoparathyroidism. Association of the disease with pseudohypoparathyroidism was also reported [8]. However, in most cases the metabolic disturbance was secondary to hypoparathyroidism. Reports of less frequent etiologies of psoriasis-associated hypocalcemia are only to be found in Laymon et al. [9] describing psoriasiform plaques in a patient with pseudohypoparathyroidism, and in another description of a girl with pseudohypoparathyroidism and psoriasis vulgaris [10].
Case Report
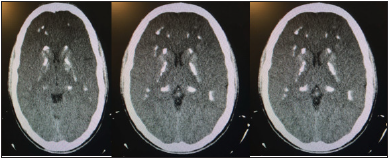
A 17-year-old Afghani male, born of a non-consanguineous marriage, with plaque psoriasis was admitted to Loghman Hakim Hospital, Tehran, Iran in 2015. He had a history of seizures from the age of 7. During this period, the patient has been treated with Phenobarbital 60mg twice daily. His condition was episodically during recent years, approximately every 3 to 4 months, he experienced seizure by falling followed by abnormal movements lasting for 3 to 4 minutes and then by impairing consciousness for few seconds. She also mentioned that the frequency of episodes has increased during the last 6 months. The patient worked in a welding workshop and recently complained of muscle pain and cramps during work. Additionally, he had been suffering numbness, stiffness and tingling of upper and especially lower extremities frequently. Past surgical history for prior parathyroid, thyroid or neck surgery was negative. His mother mentioned episodes of invasive behavior which happened every 2 or 3 months during the last years. Also, there was no history of delayed puberty or erectile dysfunction. No history of any other condition compatible to autoimmune disease has been detected. The patient had additionally noted a history of erythematous scaly and pustular lesions on the face, chest, scalp, on the elbows and knees, which began approximately 3 years before admission (Figure 1). With respect to family history, his sister had psoriasis. At the time of admission his height was 150cm and his weight was 55kg and his vital signs were stable. He presented with somehow normal mental status and acceptable orientation and speech. On examination following inflating sphygmomanometer cuff above systolic blood pressure, he experienced painful spasm of his examined hand revealing positive Trousseau’s sign. The Chvostek sign was also positive and there were no localized neurological signs. Upon investigation, total blood count, liver and renal function tests were normal. Also, the serum calcium was 6mg/dl (8.5-10mg/dl), phosphorus 8.2mg/dl (2.7-4.9mg/dl) and parathyroid hormone (PTH) level was 1.6pg/ ml (10.9-65pg/ml). Brain CT showed widespread intracranial calcification (Figure 2). ECG showed prolonged QT interval according to hypocalcemia. According to pathologic study on skin punch biopsy, regular acanthosis with elongated rete ridges along with suprapapillary thinning of epidermis was seen, additional findings were parakeratosis, neutrophilic micro-abscesses, and loss of granular layer with dilated papillary blood vessels in superficial dermal layer. A diagnosis of hypoparathyroidism was made based on hypocalcemia, hyperphosphatemia and low PTH level. This was further supported by diffuse patchy intracranial calcification in brain CT scan. It was found that the patient had seizures due to hypocalcemia. A skin biopsy was compatible with psoriasis. The EEG obtained from the patient was normal besides revealing widespread slow activity. In view of severe symptomatic hypocalcemia, the patient was started on intravenous infusion of a %10 solution of calcium gluconate (elemental calcium 9.3mg/ dl) at a rate of 0.5-1.ml/min while the heart rate was monitored and a total dose not to exceed 20mg of elemental calcium/kg. When serum calcium level reached above 8mg/dl, calcitriol with initial dosage of 0,5 microgram daily in two equal divided doses added and the regime continued for 48 hours. Then to taper the calcium gluconate infusion, calcium carbonate tablet 400mg for 4 times daily added to the drug list. Finally, calcitriol reached to 2 micrograms daily as a maintenance therapy. Although the seizure was due to the underlying hypocalcemia, the patient benefited sodium valproate 500mg twice daily to taper the phenobarbital prescribed for the patients formerly without any positive results in controlling seizures. One week later, the patient was discharged with clinical and laboratory improvement and therapy continued calcium carbonate tablet for four times daily besides oral calcitriol prescription as the dose mentioned for maintenance therapy. He advised to reduce foods with high phosphorus content such as milk, eggs, and cheese in the diet. Also, he was asked to be visited one week later to be reevaluated and to regulate the drug doses. One month later the patient showed significant regression of the psoriatic lesions and presented without any complains of tingling, muscle weakness and seizure which showed the recovery of underlying hypocalcemia.
Figure 1:Erythematous scaly lesions on the chest.

Figure 2:CT brain shows diffuse patchy calcification.
Discussion
In the present case, we have described an unusual association
of plaque psoriasis and hypoparathyroidism. Hypoparathyroidism
had not been diagnosed prior to current admission. In this case, the
PTH level stayed at the lower limit of the normal range. Biochemical
diagnosis of hypoparathyroidism is based on a combination of
hypocalcemia and hyperphosphatemia with low or inappropriately
normal PTH. Clinical manifestations of hypoparathyroidism are in
large part due to low serum-ionized calcium levels varying from
no symptoms to those of complete and long-lasting deficiency.
Mild deficiency may be revealed only by appropriate laboratory
studies. Muscular pain and cramps are early manifestations; they
progress to numbness, stiffness, and tingling of the hands and
feet. There may be only a positive Chvostek or Trousseau sign or
laryngeal and carpopedal spasms. Convulsion with or without loss
of consciousness can occur at intervals of days, weeks, or months.
These episodes can begin with abdominal pain, followed by tonic
rigidity, retraction of the head and cyanosis. Hypoparathyroidism is often mistaken for epilepsy. Headache, vomiting, increased
intracranial pressure and papilledema may be associated with
convulsion and might suggest a bra tumor. Also, the skin may
become dry and scaly, and the nails might have horizontal lines.
Cataracts in patients with long-lasting untreated disease are a direct
consequence of hypoparathyroidism; other autoimmune ocular
disorders such as keratoconjunctivitis can also occur. Permanent
physical and mental deterioration occur if initiation of treatment
is long delayed [11].
Although our patient had several classic clinical and
biochemical features of hypoparathyroidism, but according to the
probably long-lasting underlying hypocalcemia, the absence of
other manifestations of hypocalcemia was unusual. He had a longstanding
erythematous scaly lesion on his chest.
Hypocalcemia is an exacerbating factor of psoriasis and
severe psoriasis often accompanies hypocalcemia. There are case
reports of hypoparathyroidism-induced hypocalcemia leading
to the worsening of skin symptoms in psoriatic patients [12-14].
Correction of the hypocalcemia usually results in clearing of the
skin disease. It has been suggested that this disturbance is an
inherited disease with variable penetration, although it is believed
that environmental factors also play a role in its clinical expression.
Thus, the possibility that the association between psoriasis
and hypoparathyroidism is related to other mutations not yet
characterized for these diseases cannot be excluded.
Conflict of Interest: The authors declare that they have no conflict of interest.
References
- Lowes MA, Bowcock AM, Krueger JG (2007) Pathogenesis and therapy of psoriasis. Nature 445(7130): 866-873.
- Cayir A, Engin RI, Turan MI, Pala E (2014) Psoriasis vulgaris and autoimmune polyendocrine syndrome type I: a case report. J Pediatr Endocrinol Metab 27(7-8): 791-793. `
- Lebwohl M, Ortonne JP, Andres P, Briantais P (2009) Calcitriol ointment 3 microg/g is safe and effective over 52 weeks for the treatment of mild to moderate plaque psoriasis. Cutis 83(4): 205-212.
- Plavina T, Hincapie M, Wakshull E, Subramanyam M, Hancock WS (2008) Increased plasma concentrations of cytoskeletal and Ca2+-binding proteins and their peptides in psoriasis patients. Clin Chem 54(11): 1805-1814.
- Poojary SA, Lodha N, Gupta N (2015) Psoriasis in autoimmune polyendocrine syndrome type I: A possible complication or a non-endocrine minor component? Indian J Dermatol Venereol Leprol 81(2): 166-169.
- Imaeda K, Kimura R, Kato T, Kaneko N, Morita A, et al. (2012) A case of idiopathic hypoparathyroidism associated with psoriasis vulgaris. Nagoya Med J 52: 67-75.
- Fuleihan G, Brown E, Rosen C, Mulder J (2014) Parathyroid hormone secretion and action. UpToDate p.14.
- Braun GS, Witt M, Mayer V, Schmid H (2007) Hypercalcemia caused by vitamin D3 analogs in psoriasis treatment. Int J Dermatol 46(12): 1315-1317.
- Lima K, Abrahamsen TG, Wolff AB, Husebye E, Alimohammadi M, et al. (2011) Hypoparathyroidism and autoimmunity in the 22q11. 2 deletion syndrome. European Journal of Endocrinology 165(2): 345-352.
- John M, Sudeep K, Thomas N, Thomas M (2006) A mentally challenged adult with tonic convulsions, dysmorphic face and sebopsoriasis. J Postgrad Med 52(2): 145-147.
- Jabbour SA (2003) Cutaneous manifestations of endocrine disorders. Am J Clin Dermatol 4(5): 315-331.
- Lee Y, Nam YH, Lee JH, Park JK, Seo YJ (2005) Hypocalcaemia-induced pustular psoriasis-like skin eruption. Br J Dermatol 152(3): 591-593.
- Maeda T, Hasegawa H, Matsuda A, Kinoshita M, Matsumura O, et al. (2003) Severe hypocalcemia compatible with idiopathic hypoparathyroidism associated with psoriasis vulgaris. Nihon Naika Gakkai Zasshi 92(12): 2412-2414.
- Montenegro JRM, Paula FJAd, Foss NT, Foss MC (2002) Familial association of pseudohypoparathyroidism and psoriasis: case report. Sao Paulo Med J 120(1): 23-27.
© 2021 Fatemeh Kodaei. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






