- Submissions

Full Text
Advances in Complementary & Alternative medicine
An Integrative Medicine Physician’s Approach to Chronic Medical Disease
Yufang Lin*
Center for Integrative Medicine, Cleveland Clinic, USA
*Corresponding author: Yufang Lin, MD, Center for Integrative Medicine, Cleveland Clinic, USA
Submission: May 25, 2019;Published: June 04, 2019

ISSN: 2637-7802 Volume4 Issue4
Abstract
Many scientific discoveries in the last two centuries have revolutionized medicine, leading to longer survival and a prolonged lifespan. Modern medicine is excellent at treating symptoms and acute illness, but the rising prevalence of chronic diseases and ballooning medical costs suggest a different approach may be necessary. Integrative Medicine promotes a holistic view of a person and his/her concerns, reduces disease by removing the root cause of the illness and supports the innate healing ability of human body. Nutrition and intestinal support are foundational in this process. Herbal medicine and energy medicine are two of the complementary modalities commonly considered in this holistic approach. This article provides an introduction to an integrative medicine approach toward evaluation and treatment of chronic diseases.
Keywords:Integrative medicine; intestinal permeability; Mediterranean diet; herbal medicine; Medicine; Chinese traditional; Ayurveda
Introduction
Most physicians are familiar with the Hippocratic Oath, the ancient Greek text that all physicians swear to as they are officially inducted into the field of medicine. By swearing upon Asclepius, Hygieia and Panacea, we vowed to treat those who seek care as we would our family members, to treat them as partners in life, and to use dietary regiments to benefit them. Hippocratic tradition values health promotion, interventions on trauma care, mental care and art therapy interventions. Health promotion included physical activity as an essential part of physical and mental health and emphasized the importance of nutrition to improve physical performance in the Olympic Games. Furthermore, “Hippocratic tradition emphasized environmental causes and natural treatments of diseases, the causes and therapeutic importance of psychological factors, nutrition and lifestyle, independence of mind, body and spirit, and the need for harmony between the individual and the social and natural environment” [1].
Moving forward two thousand years, the discovery of Germ Theory by Louis Pasteur in the 18th Century and antibiotics by Alexander Fleming in 1928 revolutionized modern medicine. The advances in surgery and pharmaceuticals further tipped the balance in therapeutic options offered toward illnesses. Although lifestyle, stress management and environmental influences are still important, these are less likely to be discussed with patients when there are many more therapeutic options available. However, despite all the advances, the prevalence of chronic disease continues to rise, and the financial, emotional, and physical burdens also continue to rise [2].
This is not news. As an Allopathically trained physician board certified in combined internal medicine and pediatrics, I was a primary care physician for many years. One of the joys of being a primary care physician is the privilege of getting to know my patients really well. Everyone has their own stories, challenges and successes. However, with the release of each evidence-based standard of care guidelines, patients were reduced further and further into sets of data and numbers. Even more frustrating, they were not getting better. Those with chronic medical conditions still have them, they were just on more pharmaceuticals. It was disheartening, yet this was all I knew. I believed wholeheartedly I was doing the best I could to help my patients.
After the loss of my father, I was forced to reassess my beliefs. My family emigrated from Taiwan in 1980s, in search for a better future. While in Taiwan, we ate traditional Taiwanese food: Lots of fresh vegetables and fruits, some meat and lots of fish, all seasonally sourced and prepared. When we came to United States, our budgets were tight. Our dinners were still as traditionally prepared as possible, but my father’s breakfast and lunch while at work were often inexpensive bagels and muffins from the big box warehouses. Through my parent’s hard work, our circumstances improved, but starchy food remained predominant in our diet. Like many Asians, my father had hepatitis (later identified as hepatitis C). He did not tolerate the side effect of treatments, thus was monitored by his physicians to make sure his liver functions were stable. His job was physically active but stressful. At 62, he retired early and spend his days gardening, golfing, and traveling. He saw his doctors regularly and he seemed to be in good health. In the summer of 2008, his best friend died suddenly. That October, my father developed a cold that turned into bronchitis. Six weeks, three doctor’s visits, three courses of antibiotics, steroid and inhalers later, he reported having white stools. On that same day CT showed liver mass and metastasis, and twenty days later he passed away.
What caused a man who previously never had lung disease to have persistent bronchitis? What caused the liver inflammation to get out of control, and what caused the liver cancer to grow during that time? Why did his doctor, who saw him multiple times in the weeks leading up to the diagnosis, miss the progressive jaundice? Why did I, as a daughter who visited him often, miss his ailing health? These questions led me down a journey of self-discovery and healing, eventually to integrative medicine (IM), Traditional Chinese Medicine (TCM) and other complementary medicine therapies. Common to many of these healing traditions are the following concepts:
1) the evaluation of a person’s concerns needs to be holistic,
2) if the trigger of the disease can be removed the symptoms will resolve,
3) if the trigger cannot be removed then goal is to support body’s innate healing process through lifestyle measures, in particular nutrition, botanicals, stress management, movement and/or energy medicine modalities.
These concepts have revolutionized my practice, and I now work as an integrative medicine consultant at the Center for Integrative Medicine at Cleveland Clinic.
Integrative Medicine
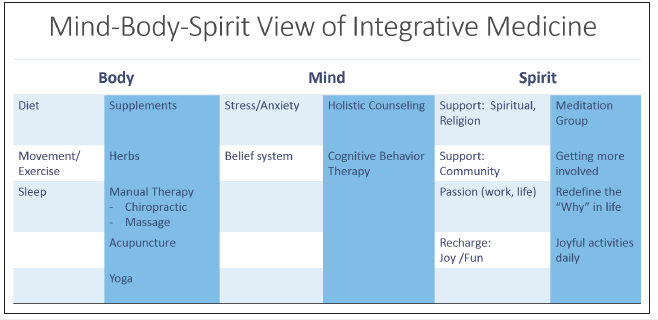
Integrative medicine is a medical practice that evaluate the patient’s health through a mind, body, and spirit perspective. Mind is about what they expend their mental energy on, their stress level and belief systems. Body is about how people physically take care of themselves: How they eat, sleep, exercise. Spirit is about whether they feel supported by their family, community, or religious beliefs. This holistic view harkens back to the Hippocratic tradition, but also reflects TCM and Ayurveda (traditional Indian medicine) practices. One is in optimal health when all of the above is in balance. By identifying the area of imbalance in each individual, we can personalize the treatment plan. IM also combines the tools and understanding from allopathic medicine and complementary medicine such as TCM, Ayurveda, herbal medicine, chiropractic, osteopathy, and holistic psychotherapy, offering a rich array of tools to support patient’s healing. As an IM physician, I have found this approach to be quite effective (Figure 1).
Figure 1:Mind-Body-Spirit view of integrative medicine.
Initial Visit
My first visit with a patient is one hour long, during which we dive deep into his or her history to figure out where the initial dysfunction started. Detailed timeline is taken on when illness occurred. I also review in depth their diet, sleep patterns, and stress levels. Often poor nutrition, high stress, lack of sleep, inadequate exercise and lack of support were identified. Family history can shed light on genetic risks which may predispose the individual to mood related diseases, poor detoxification and increased risk of hormone imbalance or neurological disorders. By spending time with patients to identifying each potential areas of concern and offering tools to support these areas, they are empowered with the ability to support their innate healing. Some are motivated to make immediate changes, others take time to implement baby steps, but this approach allow the healing process to truly be a patientcentered approach. At Cleveland Clinic Center for Integrative Medicine, our care team includes nutritionists, psychotherapists, chiropractic physicians, massage therapists, energy medicine practitioners, acupuncturists, traditional Chinese herbalist, and integrative medicine physicians. We also have the expertise from the wide network of Cleveland Clinic’s specialists when the conditions are better addressed allopathically.
This approach does take time. However, by spending time upfront with patients to truly dig into the root causes of the problems, we reduce the downstream disease burdens and the associated medical cost and suffering. A 6-year study in Netherlands compared the conventional approach among general practitioners (GP) versus care provided by GPs who had additional training in complementary and integrative medicine (CIM) and found a 10% reduction in total annual health care cost, when the GP has CIM training [3]. It is time to retool our medicine model. At my practice, I am blessed to have a full complement of alternative therapies available to offer to patients. However, some concepts and tools are widely applicable. I would like to share with you my approach to chronic medical disease with focus on nutrition, herbal medicine and energy medicine.
Chronic Inflammation, Chronic Disease
Most of the chronic medical conditions in United States are lifestyle based. The World Health Organization estimated that 80% of premature heart disease, stroke, diabetes and over 40% of cancer are preventable [4]. Top three health risk factors are unhealthy diet, physical inactivity and tobacco use. It is however quite challenging to change patients’ behavior. The difficulties are numerous. First, physicians have very limited time with patients. A 2007 study by Ming Tai-Seale et al found average primary care office visits length was 15.7 minutes, covering six topics, with very limited amount of time dedicated to a specific topic [5]. Even if a physician has the inclination to discuss nutrition, only 29% of the United States medical graduates received the minimum 25 hours recommended for nutrition education, and less than half of all school’s report teaching any nutrition in clinical setting [6]. We can’t assess and teach what we don’t know.
By not addressing nutrition adequately, we miss a huge opportunity to impact patients’ health. Chronic inflammatory diseases are the most significant cause of death in the world, and 80% of the immune cells resides (no s) in the gastrointestinal tract. Hippocrates of Kos was attributed the saying “All disease begins in the gut”. Presently, there are over 14,600 articles in PubMed studying the relationship between impaired intestinal permeability and various diseases. Indeed, intestinal permeability has been associated with number of chronic diseases such as multiple sclerosis [7], nonalcoholic fatty liver disease [8], autoimmune disease, type I diabetes mellitus, chronic fatigue syndrome [9], celiac disease, inflammatory bowel disease, colon cancer, and obesity [10]. Studies are now recognizing that intestinal epithelial barrier is a therapeutic target to treat chronic disease [11,12].
Increased Intestinal Permeability
Human gastrointestinal tract (GIT) is the largest organ in body. When spread out, the surface area of GIT is about the size of a tennis court to a double tennis court (200m2-400m2) [13]. In contrast, human skin surface area is a mere 2m2, lung surface area is larger at 100m2 but still dwarfed by the GIT. Thus, GIT is the primary interface between human body and the outside world. Despite the large surface, GIT epithelium is only one cell layer thick, each cell bound together by tight junction proteins. When these proteins become loose, the barrier becomes “leaky” or the intestinal permeability increases, allowing intestinal bacteria particles to leak through the gaps between cells into the submucosa. These foreign substances then trigger an inflammatory response, which adds to the total inflammatory burden of the body [11,12]. This process, known as metabolic endotoxemia (the rise of bacterial derived lipopolysaccharides after a meal), is a significant contributor to chronic inflammation [14], obesity and insulin resistance [15].
Integrity of the intestinal epithelial lining is critical for overall health. Disturbance of intestinal epithelium has been known as “leaky gut syndrome” in the complementary medicine community, “increased intestinal permeability” in the allopathic community, but they both describe the same condition. Primary causes of increased intestinal permeability include high fat and high carbohydrates diet [16], imbalance of the intestinal microbiome [12] and emotional stress [17]. As clinicians, if we can help patients eat better, support gut healing and manage stress better, very often the overall inflammation and the disease burden would reduce, leading to less symptoms and less need for medications.
Nutrition
Out of the many diets available, the Mediterranean diet is most well studied and has the most data supporting its anti-inflammatory benefits. Mediterranean diet consist of the following characteristics: abundant consumption of olive oil, high consumption of vegetables, fruits, legumes, nuts and seeds, moderate amount of fish and shell fish, white meat, eggs, and fermented dairy products, as well as relatively small amounts of red meat, processed meats and foods rich in sugars [18]. The Mediterranean diet has been shown to reduce cardiac disease, insulin resistance, improve blood pressure, lipid profile, reduce inflammation, oxidative stress, carotid atherosclerosis [19], and chronic pain [20].
This is not a low-fat diet. Indeed, participants in the original PREDIMED study were required to consume minimally 4 tablespoon of olive oil a day on top of ≥3 servings of nuts and fish or shellfish a week. Some participants consumed up to 1 liter of olive oil a week. The oils consumed is rich with polyunsaturated and monounsaturated fatty acid, which have proven anti-inflammatory profiles [21]. It is also a diet rich in fermented food, providing an abundance of healthy bacteria to support gut microbiome. This diet however is low in simple carbs, with commercial sweets or pastries such as cakes, cookies, biscuits or custards, limited to ≤3 servings a week. By limiting simple carbohydrates intake, this diet also limits the insulin impact on the metabolic system and inflammation process. The abundance of vegetables and fruits also brings in nature’s pharmacy: a rich spectrum of phytonutrients that are antioxidant, anti-inflammatory, antimicrobial, hepato-protective, insulin sensitizing, and mood supportive. Food, truly, is medicine.
There are two points worth considering regarding the impact of fat on intestinal health. First, many studies show high fat and high carbohydrates diet increases intestinal permeability, however, these studies did not separate out the impact from fat or carbohydrates. Secondly, most of the studies assessing fat impact on intestines were mice studies with mice fed on a high fat diet, using regular chow as control. Regular chow is composed of agricultural byproducts, such as ground wheat, corn, oats, alfalfa or soybean meals, a protein source such as fish, and vegetable oil and is supplemented with minerals and vitamins. This is a high fiber diet containing complex carbohydrates, with fats from a variety of vegetable sources. In contrast, the high fat diet consists of amino acid supplemented casein, cornstarch, maltodextrose or sucrose, and soybean oil or lard, also supplemented with minerals and vitamins. This diet has distinctly less fiber and more simple sugar such as sucrose. Sucrose is 50% fructose, which contributes to weight gain, insulin resistance and dyslipidemia [22]. The quality of lard used is also unclear. Were the studies on high fat diet truly reflecting high fat intake, or reflection the high amount of sucrose and the poor quality of fat ingested?
I often recommend patient to start with the Mediterranean diet, avoid simple sugars and processed food. Beyond simple nutrition intervention, food can be used medicinally to promote certain healing properties. I would like to share with you some of common herbs that can be easily introduced to optimize health.
Herbal Medicine
Herbal medicine is the oldest form of medicine. Neanderthal remains in El Sidrón from 50,000 years ago were found to have yarrow and chamomile in their diet, both are plants with significant medicinal properties [23]. Use of herbs is foundational in TCM and Ayurveda, and Egyptians used herbs in their medical text as early as 1850BC [24]. Indeed, modern medicine often have its roots in herbal medicine. Salicylic acid, an active ingredient of willow bark, was cited in ancient Egyptian text Ebers Papyrus, and was developed into aspirin in 1800s [25]. Popular anticancer drugs, etoposide and teniposide, were derived from yew trees, Taxus brevifolia.
Herbal medicine is the study or practice of medicine and therapeutic use of plants [26]. Plants can be used in many forms, such as teas, decoctions, tinctures, aromatherapy, and of course, as food.
Food, Tea, Aromatherapy and Other Preparations
With the advance of farming and agriculture, the modern Western diet is often rich in animal proteins and grains, but deficient in seasonal vegetables and fruits. Most of the chronic diseases are inflammatory in nature, and a pro-inflammatory diet high in starch, saturated animal fat, processed food and low in plant-based food is certainly the main culprit. As part of a comprehensive therapeutic plan to promote health and healing, a well-balanced diet rich in vegetables and fruits, clean protein, healthy fat, and limited processed food is of utmost importance.
Since we all have to eat and drink, this is also the perfect place where we can start any herbal intervention. Adding antiinflammatory herbs and spices to daily meals is a great way to bring in the healing power of plants. Another easily accessible form of herbal medicine is teas. The act of making tea- putting the water to boil, choosing the right tea, measuring the tea and the time it takes to steep the tea, is a golden opportunity for self-care. It is a quiet moment in an otherwise busy day that allows for brief rest. Many of the leafy herbs can be steeped as tea. In addition to the physical component of the tea, the aroma of tea is also medicinal, a form of aromatherapy.
Aromatherapy is inhalation or bodily application (as by massage) of fragrant essential oils for therapeutic purposes [27]. As plants are heated through cooking or steeping, the volatile oils are released into the air. These oils can be further concentrated through distillation into essential oils. It takes approximately 250lb. of lavender to make 1lb. of lavender essential oil, and 5000lb. of rose petals to make 1lb. of rose essential oil. Essential oil thus is a concentrated form of herbal medicine. As public interest in aromatherapy rises, more and more studies are being done to evaluate the efficacy and safety of aromatherapy. Many studies on the mental benefits of aromatherapy found positive impact on stress, pain, anxiety, and sleep [28,29]. Indeed, the sense of smell is the quickest way to change one’s mood. Studies also show some essential oils have antimicrobial and the anti-inflammatory properties [30,31]. As with any intervention, essential oils if used inappropriately can be harmful. As a general rule I do not suggest oral ingestion of essential oils unless directed by a trained herbalist. However, essential oil can be used easily as inhalation or topical treatments.
Finally, herbs can be extracted in high concentration for medicinal use, in the forms of glycerite extractions, alcohol tinctures, and compounded pills. TCM practitioners often offer herbal mixtures that are made as decoctions (boiling of the plants to make a concentrated tea). The purity and the formulation of these products are critical. In general, these interventions should be used under guidance of trained practitioners.
Common Herbs and Uses
Ginger and turmeric
Studies show Ginger rhizome (Zingiber officinales) is an effective anti-inflammatory, antioxidant, and anti-microbial [32,33]. Ginger is also well known for its anti-emetic and anti-spasmodic qualities, excellent for nausea, intestinal cramping and GI upset [34] I often suggest patient to add ginger into their diet when they have body aches, pains, stomach upsets, or when they are sick with respiratory infections. This is a spice that can be easily introduced into stir-fries, sautés, soups and stews. It is also excellent as a tea or decoction. Usual dose is 1 gram to 3 grams of dried ginger per day, taken as powder, capsules, or can be made as tea (1-inch fresh ginger per 2 cups, drink up to 3 cups per day).
Turmeric (Curcumae longa) rhizome is another herb that has been well studied. The active compounds collectively known as curcuminoids, has anti-inflammatory, antioxidant, anti-catabolic, neuro-protective, anti-cancer, insulin-sensitizing, and gut healing support properties. [35-37]. Turmeric can be used in a similar manner as ginger. However, turmeric is poorly absorbed. To optimize bioavailability, turmeric or curcumin should be taken with black pepper (active ingredient bioperine), which increases curcumin bioavailability by up to 2000% [38] The therapeutic dose for curcumin is 1000-2000mg, which is often difficult to obtain through diet alone (one teaspoon of turmeric, about 2-3 grams, provides 60-100mg curcumin). Thus, this is one herb that I may recommend patients to consider adding into their regimen as a supplement. It is important to note that any anti-inflammatories that impact the prostaglandin pathway can also increase bleeding risk. We see this with pharmaceuticals such as non-steroidal antiinflammatories, and similar side effects can be seen with botanicals.
Garlic and the kitchen sisters: Rosemary, Oregano and Thyme
Garlic (Allium sativum) has a strong presence through its distinctive sulfurous aroma and pungent taste. Rich in organosulfur, garlic is antimicrobial, antiviral, and antifungal, a wonderful addition during cold and flu season whether as added to food or steeped in honey. Garlic is also known for its cardio protective effect. Garlic supplementation reduces blood pressure (systolic 7-16mmHg and diastolic 5-9Hg), total cholesterol by 38.9mg/dl, and inhibit platelet aggregation [39,40]. Its antioxidant property has been shown to reduce cardiac disease progression and inhibit tumor growth [39]. Researches were done using number of garlic preparations including garlic oil, garlic powder, and aged garlic extract; most consistent benefit were shown in studies done in aged garlic extract (at 480mg per day standardized to 1.2mg of S-allylcysteine daily). I much prefer patients to cook with garlic, however, since it is such a wonderful flavoring agent. Garlic is safe and well tolerated in diet, but taking in large amount, it may affect coagulation and prolong bleeding.
Oregano (Origanum vulgare) and thyme (Thymus vulgaris) are widely used in cooking, particularly in the Mediterranean region. Rich in flavonoid and phenolic acid compounds, they have antioxidant, antiviral, antibacterial properties [41] Oregano essential oil has strong action against Staphylococcus species including S. aureus, multiresistant strains of Pseudomonas aeruginosa and Escherichia coli. It is also antifungal and effective against Candida glabarata. Thyme has very similar profile. Rosemary (Rosmarinus officinalis) has been pharmacologically validated for its antimicrobial, anticancer, anti-diabetic, anti-inflammatory, antinociceptive, antioxidant, antithrombotic, and hepato-protective functions. It is such an antioxidant powerhouse; it has long been used as preservative. More recently, rosemary has been studied for its therapeutic effect against degenerative brain disease such as Alzheimer’s, and the results are promising [42]. These herbs are beautiful in appearance, luscious in smell, and tasty in food. I encourage patients to cook with them often. In cold and flu seasons, 1 teaspoon of dried herb infused in a cup of near boiling water for 10 minutes, consume three times a day, can be quite effective. Herb infused honey are tasty and palatable for young children. Last but not least, essential oils of oregano and thyme can be mixed with carrier oils (such as coconut oil or olive oil) to apply topically for minor bacterial or fungal infections.
Chamomile and peppermint
German Chamomile (Matricaria recutita) is perhaps one of the most well-known herbal teas in the world. Chamomile flowers are known for its anti-inflammatory, antioxidant, antidepressant, anti-microbial, anti-diarrheal, hepato-protective, and anti-diabetic properties [43]. It has been shown to support mood [44], sleep [45], intestinal health [46], and safe to use in all ages. Peppermint (Mentha x piperita) leaves has antioxidant, antiviral, antimicrobial actions. It is known for its benefits to GI system as an antispasmodic as well as calming effect on nervous system [47]. Both are wonderful for anxiety and nervous stomachs and are easily available as teas.
Lavender and tea tree
Lavender (Lavendula angustifolia) was used in 1800s in hospital as anti-septic and anti-microbial. Well known for its relaxing properties [48,49], lavender is also an antioxidant, analgesic, and anti-inflammatory [50]. One can cook or make tea with lavender- it is part of Herb de Provence spice, but if used too liberally the dish can taste soapy. The intense aroma of lavender however lends itself to be used as aromatherapy, through sprays, diffusers, perfumes, massage oils and creams. Tea tree (Melaleuca alternifolia) is well known for its antimicrobial and anti-inflammatory properties [51]. Tea tree essential oil can be used topically to treat simple bacterial or fungal infections or added to water as an anti-septic. It is important to note that essential oil is quite strong, and tea tree essential oil can be neurotoxic to infant and little animals [52,53] and should be used with caution.
Energy Medicine
Let’s try a little experiment. Rub your hands briskly until your palms feels warm, then separate your palms by one to two inches and move them around each other. Do you feel anything? In my clinical experience, about half of the individuals feel something. A sense of heat, vibration, pulling. What is it?
TCM calls this Qi (Chi), Ayurveda calls this Prana, both are names for Energy. The concept of Energy Medicine may be foreign to most physicians, but it is foundational in many healing traditions. TCM and Ayurveda believe we are not only made of blood, muscles and bones, we are also made of energy. Energy circulates in our body through energy pathways, just like blood circulates through blood vessels. A healthy energy system is as important as a healthy circulatory system. If the energy becomes stagnant, then the corresponding organ system may become dysfunctional.
All these may sound esoteric and hard to believe. There have been number of studies demonstrating the presence of the energy pathway (known as meridians) in TCM [54,55]. The palm rubbing exercise is a simple way to demonstrate Qi. People have variable sensitivity to the energy flow, some more sensitive than others, but we all have this energy. From a holistic view, food is energy, emotion is energy, and activities- whether physical or mental- can either restore or deplete our energy. A person complaining of fatigue may be eating too much sugar in their diet, which may lead to a quick energy spike but followed by a persistent lull. Fatigue can also come from not getting enough restorative energy from sleep, exercise, joyful activities, or from using too much energy by mental anxiety, stress, or exercise in excess. The environment and the people around us also impact our energy.
As an Integrative Medicine specialist, I always review my patient’s food intake, exercise and sleep patterns, stress level, relationships and work to get a holistic view. It is important to look at the physical aspect to tease out the root cause of illness. For those where the physical patterns are not enough to explain their illnesses, I turn to energy medicine for therapeutic ideas.
The me-too movement and the lower chakras
Over 100 million Americans suffer from Chronic Pain [56], more women than men [57]. Women may be more sensitive to pain and have more opportunity for pain (monthly menstrual pain and childbirth). However, the Me-Too movement in 2018 remind us that many people have unresolved emotional trauma that have not been discussed or addressed. A study of New York City at-risk youth found men were more likely to be physically and emotionally neglected, but women were more likely to be physically, emotionally and sexually abused. Women are at higher risk for depression, anxiety, and post-traumatic stress disorder [58]. Women are also at higher risk for Irritable bowel syndrome [59], chronic pelvic pain [60], and autoimmune conditions. Are these related?
Ayurveda believes we have seven main energy centers known as chakras that spans from perineum to the crown [61]. The root chakra, located at the base of the spine, is associated with adrenal gland and sense of security. The sacral chakra, located at the pelvis, is associated with sex organs, creativity, emotion and sexual energy. The third chakra, or the solar plexus, is located just above the naval region and is associated with pancreas, the sense of power and selfexpression. If a person has been abused, threated, disempowered, or felt insecure, the corresponding energy system can become stagnant, and may manifest in adrenals (adrenal fatigue, chronic stress), intestines (Irritable bowel, obesity), or sex organs (dyspareunia, dysmenorrhea, pelvic pain).
It is important to look at the physical causes. Sometimes gut issues and obesity is due to poor diet and has nothing to do with emotional health. However, in individuals who have been to numerous physicians, tried many interventions and still not improving, the cause of the disease may lie in the emotional body. Full healing may require therapies to release the emotional trauma. In case you are interested, here are the rest of the seven primary chakras. The heart chakra, reside in the center of the chest, is associated with thymus and heart, love, self-love, compassion and relationship to others. The throat chakra, resides in the throat, is associated with thyroid gland and the ability to speak and communicate clearly and effectively. The third eye, located in the center of forehead between eyebrows, is associated with pituitary glands, openness, and intuition. Finally, the crown chakra, resides to top of the head, is associated with pineal gland and connection to the higher power. Dysfunctions in each of these chakras may present with cardiovascular disease or lung disease (heart), thyroid disease or dysphagia (throat), headache and vision changes (third eye, crown).
Heart, lung and emotions
In TCM, every major organ is associated with a specific meridian, emotion, and circadian rhythm. If someone has a symptom that tend to happen at the same time, it may suggest that meridian is not working as well, and by looking at the associated organ system and emotions, it may help us further define the cause of illness. Shortness of breath, for instance, is a serious complaint that require a thorough cardiac and pulmonary work up. However, sometimes no cardiac or pulmonary causes were found. Often these individuals may have suffered significant losses within the last six months to a year. My father never had lung disease, but six months after his best friend’s passing, he developed recurrent bronchitis. Women with miscarriages and losses often present with similar complaints of frequent lung infections or the sensation of unable to take a deep breath in. In TCM, lung holds the emotion of grief; in time of loss, the lung meridian may not work well, and one may be more likely to develop lung symptoms or infections. As the individuals work through stages of grieving, the energy stagnation of the lung meridian usually resolves.
Another helpful tool is the TCM clock. In TCM, each organ energy peaks at certain time of day. If a person has symptoms at same time most days, it is worthwhile looking at the organ system associated with that time. Insomnia, for instance, can be caused by environmental noise, stress and other factors. If someone tend to wake up at 2 am, which is associated with liver meridian (1-3am), the liver may be overworking, or the person may hold unresolved anger, which is the emotion associated with liver meridian. This is another tool that help identify the causes of illnesses.
Energy medicine modalities
A healthy energy system is supported by balanced emotions, proper nutrition, regular movement, restorative sleep, and healthy environment. Exercises such as Tai Chi, Gi Qong and Yoga are known to support healthy energy flow in the body. Mindfulness practices and meditation are helpful at calming the nervous system. In those individuals whose health is impacted by emotional triggers, holistic psychotherapy and biofeedback can be very helpful. Acupuncture is excellent for energy support; massage therapy and chiropractic manipulations can also be supportive. In addition, there are energy healing practices such as Reiki, Healing Touch, and Cranial Sacral therapy by trained energy medicine provider which can be effective in supporting a healthy energy system.
Summary
The many scientific discoveries in the last two centuries has revolutionized medicine, leading to longer survival and prolonged lifespan. We want to live those years with vitality and with ease. Modern medicine is excellent at treating symptoms and acute illness, but the rising prevalence of chronic diseases and the ballooning medical cost suggest something fundamental may be missing. Integrative Medicine promotes a holistic view of a person and his/her concerns, reduce disease by remove the root cause of the illness and support our body’s innate healing ability. Nutritional and intestinal support is foundational in this process. Herbal medicine and energy medicine are two of the complementary modalities commonly considered in this holistic approach. These treatment modalities empower patients and allow the practice of health and healing to start at home.
References
- Kleisiaris CF, Sfakianakis C, Papathanasiou IV (2014) Health care practices in ancient Greece: The hippocratic ideal. J Med Ethics Hist Med 7: 3-7.
- CDC (2019) Health and economic costs of chronic disease. National Center for Chronic Disease Prevention and Health Promotion (NCCDPHP), USA.
- Taw MB (2015) Integrative medicine, or not integrative medicine: that is the question. Journal of Integrative Medicine 13(6): 350-352.
- WHO (2019) Overview-preventing chronic disease: A vital investment. Chronic disease and promotion.
- Tai-Seale M, McGuire TG, Zhang W (2007) Time allocation in primary care office visits. Health Services Research 42(5): 1871-1894.
- Adams KM, Butsch WS, Kohlmeier M (2015) The state of nutrition education at US medical schools. Journal of Biomedical Education 2015: 1-7.
- Annibali V, Policano C, Buscarinu MC, Lionetto L, Mechelli R, et al. (2014) Intestinal permeability in multiple sclerosis. Journal of Neuroimmunology 275(1-2): 54.
- Utzeri E, Usai P (2017) Role of non-steroidal anti-inflammatory drugs on intestinal permeability and nonalcoholic fatty liver disease. World Journal of Gastroenterology 23(22): 3954-3963.
- Morris T, Berk M, Carvalho AF, Caso JR, Sanz Y, et al. (2016) The role of microbiota and intestinal permeability in the pathophysiology of autoimmune and neuroimmune processes with an emphasis on inflammatory bowel disease type 1 diabetes and chronic fatigue syndrome. Curr Pharm Des 22(40): 6058-6075.
- Vancamelbeke M, Vermeire S (2018) The intestinal barrier: A fundamental role in health and disease. Expert Review of Gastroenterology & Hepatology 11(9): 821-834.
- Odenwald MA, Turner JR (2017) The intestinal epithelial barrier: A therapeutic target? Nature Reviews Gastroenterology and Hepatology 14(1): 9-21.
- Bischoff SC, Barbara G, Buurman W, Ockhuizen T, Schulzke JD, et al. (2014) Intestinal permeability-A new target for disease prevention and therapy. BMC Gastroenterology 14(1): 1-25.
- Sekirov I, Russell S, Antunes L (2010) Gut microbiota in health and disease. Physiological Reviews 90(3): 859-904.
- Festi D, Schiumerini R, Eusebi LH, Marasco G, Taddia M, et al. (2014) Gut microbiota and metabolic syndrome. World Journal of Gastroenterology 20(43): 16079-16094.
- Cani PD, Amar J, Iglesias MA, Poggi M, Knauf C, et al. (2007) Metabolic endotoxemia initiates obesity and insulin resistance. Diabetes 56: 1761- 1772.
- Rahman K, Desai C, Iyer SS, Thorn NE, Kumar P, et al. (2016) Loss of junctional adhesion molecule a promotes severe steatohepatitis in mice on a diet high in saturated fat, fructose and cholesterol. Gastroenterology 151(4): 733-746.
- Sun Y, Zhang M, Chen CC, Gillilland M, Sun X, et al. (2013) Stress-induced corticotropin-releasing hormone-mediated NLRP6 inflammasome inhibition and transmissible enteritis in mice. Gastroenterology 144(7): 1478-1487.
- Casas R, Sacanella E, Estruch R (2014) The immune protective effect of the Mediterranean diet against chronic low-grade inflammatory diseases. Endocrine, Metabolic & Immune Disorders-Drug Targets 14(4): 245–254.
- Martínez GA, Salvadó J, Estruch R, Corella D, Fitó M, et al. (2015) Benefits of the Mediterranean diet: Insights from the PREDIMED Study. Progress in Cardiovascular Diseases 58(1): 50-60.
- Veronese N, Stubbs B, Noale M, Solmi M, Luchini C, et al. (2016) Adherence to the Mediterranean diet is associated with better quality of life: data from the Osteoarthritis Initiative. Am J Clin Nutr 104(5): 1403- 1409.
- Calder PC (2017) Omega-3 fatty acids and inflammatory processes: from molecules to man. Biochem Soc Trans 45(5): 1105-1115.
- Warden, Craig H, Fisler JS (2008) Comparisons of diets used in animal models of high fat feeding. Cell Metab 7(4): 277-279.
- Owen J (2012) Neanderthals self-medicated?
- Tieraona Low Dog M (2019) Botanical foundations. University of Arizona Center for Integrative Medicine, USA.
- Jeffreys D (2008) Aspirin: The remarkable story of a wonder drug. Chemical Heritage Foundation. Philadelphia, USA.
- (2019) Merriam-Webster Dictionary.
- (2019) Aromatherapy. Merriam-Webster Dictionary.
- Rasooli SA, Salehi F, Mohammadpoorasl A (2019) Comparing the effects of aromatherapy massage and inhalation aromatherapy on anxiety and pain in burn patients: A single-blind randomized clinical trial. Burns 42(8):1774-1780.
- Johnson JR, Rivard RL, Griffin KH, Kolste AK, Joswiak D, et al. (2018) The effectiveness of nurse-delivered aromatherapy in an acute care setting. Complement Ther Med 25: 164-169.
- Silva GL, Luft C, Lunardelli A, Amaral RH, Melo DA, et al. (2015) Antioxidant, analgesic and anti-inflammatory effects of lavender essential oil. An Acad Bras Cienc 87(2 Suppl): 1397-1408.
- Ueki S, Niinomi K, Takashima Y, Kimura R, Komai K, et al. (2014) Effectiveness of aromatherapy in decreasing maternal anxiety for a sick child undergoing infusion in a Pediatric clinic. Complement Ther Med 22(6):1019-1026.
- Shirvani MA, Motahari Tabari N, Alipour A (2015) The effect of mefenamic acid and ginger on pain relief in primary dysmenorrhea: a randomized clinical trial. Arch Gynecol Obstet 291(6): 1277-1281.
- Semwal RB, Semwal DK, Combrinck S, Viljoen AM (2015) Gingerols and shogaols: Important nutraceutical principles from ginger. Phytochemistry 117: 554-568.
- Srinivasan K (2017) Ginger rhizomes (Zingiber officinale): A spice with multiple health beneficial potentials. Pharma Nutrition 5(1): 18-28.
- Henrotin Y, Priem F, Mobasheri A (2013) Curcumin: A new paradigm and therapeutic opportunity for the treatment of osteoarthritis: Curcumin for osteoarthritis management. Springerplus 2(1): 1-9.
- Hassanalilou T, Ghavamzadeh S, Khalili L (2019) Curcumin and Gastric cancer: A review on mechanisms of action. J Gastrointest Cancer 50(2): 185-192.
- Kim Y, Clifton P (2018) Curcumin, cardiometabolic health and dementia. Int J Environ Res Public Health 1-34.
- Prasad S, Aggarwal BB (2014) Recent developments in delivery, bioavailability, absorption and metabolism of curcumin: the golden pigment from golden spice. Cancer Res Treat 46(1): 2-18.
- Varshney R, Budoff MJ (2016) Garlic and heart disease. J Nutr 146(2): 416S-421S.
- Adaki S, Adaki R, Shah K, Karagir A (2014) Garlic: Review of literature. Indian J Cancer 15(4): 577-581.
- Liu Q, Meng X, Li Y, Zhao CN, Tang GY, et al. (2017) Antibacterial and antifungal activities of spices. Int J Mol Sci 18(6): 1-62.
- Habtemariam S (2016) The therapeutic potential of rosemary (Rosmarinus officinalis) diterpenes for Alzheimer’s disease. Evid Based Complement Alternat Med pp. 1-14.
- Miraj S, Alesaeidi S, Sciences M, Hospital A (2016) A systemic review study of therapeutic effects of Matricaria recuitta chamomile (chamomile). Electron Physician 8(9): 3024-3031.
- Keefe JR, Mao JJ, Soeller I, Li QS, Amsterdam JD (2017) Short-term openlabel Chamomile (Matricaria chamomilla L.) therapy of moderate to severe generalized anxiety disorder. Phytomedicine 23(14): 1699-1705.
- Adib hajbaghery M, Mousavi SN (2019) The effects of chamomile extract on sleep quality among elderly people: A clinical trial. Complement Ther Med 35: 109-114.
- Mehmood MH, Munir S, Khalid UA, Asrar M, Gilani AH (2015) Antidiarrhoeal, antisecretory and antispasmodic activities of Matricaria chamomilla are mediated predominantly through K± Channels activation. BMC Complement Altern Med 24: 15-75.
- Mckay DL, Blumberg JB (2006) A Review of the bioactivity and potential health benefits of peppermint tea (Mentha piperita L.). Phytother Res 20(8): 619-633.
- Bikmoradi A, Khaleghverdi M, Seddighi I, Moradkhani S, Soltanian A, et al. (2019) Complementary therapies in clinical practice effect of inhalation aromatherapy with lavender essence on pain associated with intravenous catheter insertion in preschool children: a quasiexperimental study. Complementary Therapies in Clinical Practice 28: 85-91.
- Seyyed-rasooli A, Salehi F, Mohammadpoorasl A (2018) Comparing the effects of aromatherapy massage and inhalation aromatherapy on anxiety and pain in burn patients: A single-blind randomized clinical trial. Burns 42(8): 1774-1780.
- Silva GL, Melo DA, Luft C, Lunardelli A, Amaral RH (2015) Antioxidant, analgesic and anti-inflammatory effects of lavender essential oil. An Acad Bras Cienc 87(2 Suppl): 1397-1408.
- Hammer KA (2019) Treatment of acne with tea tree oil (melaleuca) products: A review of efficacy, tolerability and potential modes of action. Int J Antimicrob Agents 45(2): 106-110.
- Villar D, Knight MJ, Hansen SR, Buck WB (1994) Toxicity of melaleuca oil and related essential oils applied topically on dogs and cats. Vet Hum Toxicol 36(2): 139-142.
- Morris MC, Donoghue A, Markowitz JA, Osterhoudt KC (2003) Ingestion of tea tree oil (Melaleuca oil) by a 4-year-old boy. Pediatr Emerg Care19(3): 169-171.
- Zhang WB, Wang GJ, Fuxe K (2015) Classic and modern meridian studies: A review of low hydraulic resistance channels along meridians and their relevance for therapeutic effects in traditional chinese medicine. Evid Based Complement Alternat Med 1-14.
- Stefanov M, Potroz M, Kim J, Lim J, Cha R, et al. (2013) The primo vascular system as a new anatomical system. JAMS Journal of Acupuncture and Meridian Studies 6(6): 331-338.
- Rosenquist EW (2018) Overview of the treatment of chronic non-cancer pain. In: Aronson M, Waltham MA (Eds.).
- Van Hecke O, Torrance N, Smith BH (2013) Chronic pain epidemiology and its clinical relevance. Br J Anaesth 111(1): 13-18.
- Gwadz MV, Nish D, Leonard NR, Strauss SM (2007) Gender differences in traumatic events and rates of post-traumatic stress disorder among homeless youth. J Adolesc 30(1): 117-129.
- Canavan C, West J, Card T (2014) The epidemiology of irritable bowel syndrome. Clin Epidemiol 6: 71-80.
- Latthe P, Latthe M, Say L, Gülmezoglu M (2006) WHO systematic review of prevalence of chronic pelvic pain: a neglected reproductive health morbidity. BMC Public Health 6: 177.
- Dale C (2009) The complete book of Chakra Healing: Activate the transformative power of your energy centers. Llewellyn Publishing, Woodbury, Minnesota, USA.
© 2019 Yufang Lin. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






