- Submissions

Full Text
Advances in Complementary & Alternative medicine
Patients with Klippel-Trenaunay Syndrome
Tong Zheng Hong*
As-You-Wish Healthcare Institute, Taiwan
*Corresponding author: Tong Zheng Hong, As-You-Wish Healthcare Institute, Taiwan
Submission: June 13, 2018;Published: January 03, 2019

ISSN: 2637-7802 Volume3 Issue3
Abstract
Klippel-Trenaunay syndrome is the most frequent systemic venous angiodysplasia. It is characterized by cutaneous capillary malformations– naevus flammeus, excessive growth of soft and bone tissue, venous and lymphatic malformations. Investigative methods include: clinical examinations, venography as the evidence of dysplastic changes of superficial and/or deep venous system, the Moyne obstruction and venous insufficiency perforator. Treatment is conservative, related to that of chronic venous disease. The surgery is aimed at removing the varices and insufficient perforators.
Keywords: Klippel-Trenaunay syndrome; Varices; Naevus flammeus; Tissue hypertrophy
Introduction
Klippel and Trenaunay in 1900 described the clinical syndrome with characteristic signs on the lower limb:
A. Varices (formed already in the childhood),
B. Naevus flammeus,
C. Hypertrophy of tissues (especially bones with limb prolongation) [1].
They pointed out the venous angiodysplasia, belonging to the non-degenerative and non-inflammatory angiopathies [2]. Naevus flammeus occurs in all cases. The authors also described cruciate, or dissociated type, where varices and hypertrophy occur on one and naevus on the other limb. Klippel-Trenaunay syndrome is often confused with Parks-Weber syndrome. At the other one, A-V shunt is always present, at which there are palpable whirl, pain, pulsing veins prone to rapid progression and frequent relapses. Clinically it manifests by vein dilatation and cardiac decompensation [3,4].
The syndrome is often connected with malformations of lymphatic blood vessels and lymphoedema, therefore it is favorable to perform an operation in childhood to prevent the onset of big oedema and limb elongation [5].
The syndrome incidence is 1/20 000–40 000 live-born children. The diagnosis can be made according to the specialist at the Mayo clinic if two of three main symptoms are present. The incidence is sporadic, men and women are affected equally often, the racial predilection was not found, and symptoms may appear at birth, or during childhood [6].
Case History 1
20 years old patient was admitted to the Clinic of vascular surgery, East Slovak Institute of Cardiovascular Diseases, Inc. in Košice for the first time in December 2014 for surgical solving of the chronic venous insufficiency on the left lower limb with the presence of pronounced stem varices, concentrated mainly medially on the right shin (Figure 1).
Figure 1:Varicosity on the left lower limb in the patient with TKS (status before operation, and after operation).

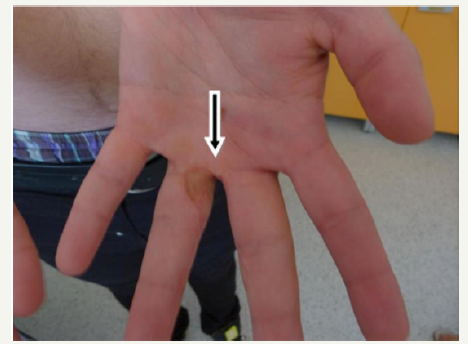
At admission the limb oedema was present +2cm in full size. At physical examination we observed on the chest centrally not clearly limited haemangioma of the size of 7x5cm (Figure 2). The patient in his history told about exercise-induced redness of the skin in the exposed area, deviation of the nasal septum, and status post operation of 3rd and 4th finger of the left upper limb for syndactyly (Figure 3).
Figure 2:Naevus flammeuslocalised on the chest
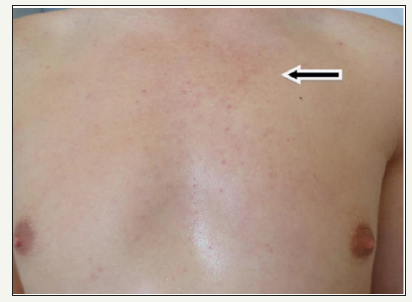
Figure 3:Syndactyly (status post operation) in the patient with KTS.
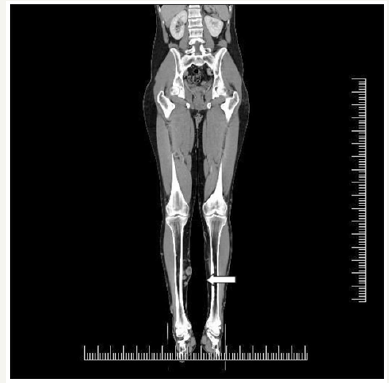
Subsequently, due to suspected Klippel-Trenaunay syndrome, the ultrasound and CT AG examinations of the venous system of lower limbs was supplemented. The CT AG examination shows potential A-V malformation on the lower limb in the anteromedial region of the shin, and varicose focuses throughout the whole tibia (Figure 4). The examination does not confirm any lytic changes of bone structures. The patient was also examined in the respect of haemo-coagulation, and the thrombophilia was confirmed. After diagnostics and preparation, the patient underwent an operation. The stem insufficiency VSM sin.l towards to v. accesoria anterior l.sin., confirmed by ultrasound and CT AG findings were the indication for surgery. Subsequently, crossectomia and stripping VSM throughout the whole course, obliterated vv. perforantes CI-CIII, posterior gastrocnomic and anterior lateral branch. Post operation the patient was afebrile, pressure and pulse stable and compensated, surgical wounds were calm, did not leak healed p.p.i. The patient was informed on the next treatment procedure (elastic bandage, drinking and motion regimen), and was released to the outdoor care.
Figure 4:Varicosity of the right tibia in the transversal section.
After the recovery period in February 2015 he was re-admitted to the Clinic of Vascular Surgery in order to remove SF reflux on the right lower limb, where extensive stem varices were present as well as on the collateral side. In the early post-operative period, there were no complications, so the patient was informed about his health status and the need for the medication and released for the outpatient care.
Case History 2
39 years old woman patient was admitted to the Clinic of vascular surgery, East Slovak Institute of Cardiovascular Diseases, Inc. in Košice for persistent swelling of the left tibia, progression of relapsing varicose veins of the left tibia with the tendency to deterioration. In anamnesis she overcame usual childhood diseases, surgery of varicose veins in the left lower limb at the catchment surgical department, in the dispensary of angiologist and orthopaedist for spine scoliosis. For a long time she used venotonics and anticoagulant therapy with low molecular heparin (LMWH).
Within the family there were no problems with varicose veins. At admission, on the shin on the right there were extensive stem varicosities, pre-tibial and perimalleolar oedema. Pulsations were bilaterally well tangible at full range, trophic changes of the skin and adnex were not present. In the sacral region there was haemangioma of the size of 10x10cm (Figure 5). The whole left lower limb was thicker by 3-4cm. The left foot was significantly smaller than the right one, with skeletal malformation (Figure 6).
Figure 5:Naevus flammeusin the sacral and right gluteal region.

Figure 6:Deformities and changed configuration of the left foot.

In the control ultrasound of the lower limb vein system the finding on the left lower limb was following: v. saphena magna as well as v. saphena parva were extirpated, without any signs of recurrence, perforators on the tibia were sufficient. On the dorsal side of the thigh the cranial extension protruding from the stump of the extirpated v. saphena parva was confirmed by examination. It was significantly dilated with the luminal diameter of 13.5mm. Extension was drained by dilated perforator in the middle of dorsomedial side of the thigh running into v. femoralisl.sin.
In the preoperative examination the normochromatic anaemic syndrome of slight degree v.s. sideropenic, leucopaenia of slight degree, and slight hypercholesterolemia dominated in the laboratory picture. According to the examination conclusion, the patient was cardio-pulmonary compensated without any contraindications to surgery.
Under the total anaesthesia in the position on the abdomen, the stump of v. saphena parva l.sin was anastomized, its distal and proximal extension. The distal extension was fibrotically changed, probably after previous surgery. The proximal one was about 0.7cm, fibrotically changed after previous inflammations. After its skeletinization in the middle third of the back half of the thigh we ligated its tertiary part in the confluence into v. femoralis l.sin. This eliminated the reflux between the proximal extension of v. saphena parva and v. femoralis l.sin.
In the post-operative period the patient was afebrile, stabilised, and compensated. Surgical wounds healed p.p.i., they did not leak immediately after operation, on the left lower limb, there was high elastic bandage, Twelve hours after operation the patient was risen to her feet, rehabilitated, instructed about the necessity of high elastic bandage in home care during 4–6 weeks. On day 3 after operation she was in good condition and was released from hospital to home care.
Conclusion
Klippel-Trenaunay syndrome belongs among the most often occurring venous angio-dysplasia. Its incidence is confirmed at least by two of three malformations: naevus flammeus on the skin, venous and lymphatic malformation, excessive growth of soft and bone tissues [7,8]. Regarding the late diagnostics patients usually come late in their middle age, after repeated operations on the venous system, when the right and precise diagnostics are not possible as well as the treatment of the disorders of the venous and lymphatic systems, which is documented by the case histories in our workplace.
References
- Klippel M, Trenaunay P (1900) Du naevus variquex osteohypertrophique. Arch Gen Med Paris 3: 611-672.
- Mazuch J, Mišánik, L, Mitacz K (1988) Syndróm Klippelov Trenaunayov. Brat Lek Listy 89(12): 899-902.
- Štvrtinová V. Choroby ciev. pp. 546-549.
- Gloviczki P, Driscoll DJ (2007) Klippel-Trenaunay syndrome: Current management. Phlebology 22(6): 291-298.
- Bliznak J, Staple TW (1974) Radiology of angiodysplasias of the limb. Radiology 110(1): 35-44.
- Baskerville PA, Ackroyd JS, Browse NL (1985) The etiology of the Klippel- Trenaunay syndrome. Ann Surg 202(5): 624-627.
- Dvorožňáková M (2016) Mitral clip-intervenčná liečba mitrálnej insuficiencie. Cardiology Letters 25(1): 39-44.
- Jankajová M (2008) Má dĺžka celkového ischemického času (príznaky balón) u pacientov s primárnou PCI dopad na funkciu ľavej komory? Kardiológia pre prax 17(2): 15S.
© 2018 Zavacká M. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






