- Submissions

Full Text
Archives of Blood Transfusion & Disorders
Evaluation of Haematological Changes Associated to Non- Hodgkin Lymphoma in Subjects in Enugu State, South East, Nigeria
Emmanuel Ifeanyi Obeagu1*, Getrude Uzoma Obeagu2 and Grace I Amilo3
1Department of Health Services, Michael Okpara University of Agriculture, Nigeria
2Department of Nursing Science, Ebonyi State University, Nigeria
3Department of Medical Laboratory Science, Nnamdi Azikiwe University, Nigeria
*Corresponding author: Emmanuel Ifeanyi Obeagu, Department of Health Services, Michael Okpara University of Agriculture, Umudike, Abia State, Nigeria
Submission: November 13, 2017;Published: December 06, 2017
ISSN: 2578-0239Volume1 Issue2
Abstract
Non- Hodgkins lymphoma (NHL) is a clonal proliferation of lymphatic tissues. It still occurs in this part of the world but most times may be misdiagnosed and leads to serious problem to the patients. Human Immunodeficiency Virus (HIV) and falciparum malaria are endemic here and increase chances of suffering from non-Hodgkins lymphoma. The study was done to determine the changes associated with non-Hodgkins lymphoma on haematological parameters in subjects in Enugu, South East, Nigeria. The study was done a secondary health institution in Enugu State, Nigeria. The study is a hospital based prospective cross sectional study using purposive sampling technique from January 2015 to July 2017. The subjects comprised of a total of eighty (80) subjects, 40 subjects were non-Hodgkin lymphoma patients aged 29-75 years (15 females and 25 males) and 40 (20 females, 20 males) subjects were apparently healthy individuals aged matched as the control. The results were presented in tables as mean and standard deviation and student t-test used for analysis and the level of significance was set at P<0.05. The haematological investigations were done using Mindray BC- 5300. The results showed significant increase (P<0.05) in WBC, Neutrophil, Monocytes, and Eosinophil of the non-Hodgkin Lymphoma (NHL) subjects (16.25±3.7 X109/L, 90.3±5.2%, 2.3±0.3%, 0.4±0.1%) compared to the control (5.23±1.2 X109/L, 67.5±6.7%, 30.7±5.6%, 0.2±0.1%), significant decrease (P<0.05) in Lymphocyte, red blood cell, haemoglobin, packed cell volume, mean cell haemoglobin, mean cell haemoglobin concentration and platelets of the non-Hodgkin lymphoma (NHL) subjects (6.8±1.2%, 3.62±0.68 X1012/L,10.3±1.5g/dl, 30.8±5.1%, 85.0±10.4fl, 28.5±2.3pg, 335.0±21.0g/dl, 208.0±16.0 X109/L) compared to the control (30.7±5.6%, 4.73±0.49 X1012/L, 92.0±15.2fl, 30.0±4.6pg, 350.0±25.0g/l, 250.0±20.0 X109/L) and no significant difference (P>0.05) in basophil of the non- Hodgkin Lymphoma (NHL) subjects (0.2±0.1%) compared to the control (0.1±0.1%) respectively. It study shows that non-Hodgkins lymphoma suppresses red blood cell, haemoglobin, packed cell volume, red cell indices and platelets and increases total white cell, neutrophil and monocytes. This will be of diagnostic and prognostic help to the oncologists and the patients.
Keywords: Haematological changes; Non Hodgkin lymphoma subjects; Enugu; Nigeria
Introduction
Lymphoma has been described as a heterogeneous group of malignancies with different biology and prognosis. Generally, lymphomas are grouped into 2, namely non-Hodgkin lymphoma (NHL) and Hodgkin disease. It has been reported that 85% of all malignant lymphomas are NHLs [1]. Non-Hodgkin lymphoma includes many clinicopathologic subtypes, each with unique epidemiologies; etiologies; morphologic, immunophenotypic, genetic, and clinical features; and responses to therapy. With respect to prognosis, NHLs can be divided into two groups, indolent and aggressive [2]. Although a variety of laboratory and imaging studies are used in the evaluation and staging of suspected NHL, a well-processed haematoxylin and eosin (H'E)-stained section of an excised lymph node is the mainstay of pathologic diagnosis. The treatment of non-Hodgkin lymphoma (NHL) varies greatly, depending on tumor stage, grade, and type and various patient factors [3]. It was reported that approximately 287,000 new cases of NHL are reported in the world each year [4]. Non-Hodgkin lymphoma affects more males than females, and the incidence increases with age. In most African populations, NHL is relatively rare but the relative frequency is above the world average in North and sub-Saharan Africa because of the high incidence of Burkitt's lymphoma (BL) in children in the tropical zone of Africa [5].
NHLs are tumors originating from lymphoid tissues, mainly of lymph nodes. Various neoplastic tumor cell lines correspond to each of the cellular components of antigen-stimulated lymphoid follicles [6]. NHL represents a progressive clonal expansion of B cells or T cells and/or NK cells arising from an accumulation of lesions affecting proto-oncogenes or tumor suppressor genes, resulting in cell immortalization. These oncogenes can be activated by chromosomal translocations, or tumor suppressor loci can be inactivated by chromosomal deletion or mutation. Also, the genome of certain lymphoma subtypes can be altered with the introduction of exogenous genes by various oncogenic viruses. A lot of cytogenetic lesions are linked to specific NHLs, reflecting the presence of specific markers of diagnostic significance in sub classifying various NHL subtypes. For many of the B-cell NHL subtypes, the pattern of growth and cell size may be important determinants of tumor aggressiveness. Lymphomas of small lymphocytes generally have a more indolent course than those of large lymphocytes, which may have intermediate-grade or high-grade aggressiveness. However, some subtypes of high-grade lymphomas are characterized by small cell morphology [7-9].
Some viruses are implicated in the pathogenesis of NHL, probably because of their ability to induce chronic antigenic stimulation and cytokine dysregulation, which leads to uncontrolled B-or T-cell stimulation, proliferation, and lymphomagenesis. Epstein-Barr virus (EBV) is a DNA virus that is associated with Burkitt lymphoma (especially the endemic form in Africa), Hodgkin disease, lymphomas in immunocompromised patients [10] and sinonasal lymphoma. Human T-cell leukemia virus type 1 (HTLV- 1) causes a latent infection via reverse transcription in activated T-helper cells. This virus is endemic in certain areas of Japan and the Caribbean islands, and approximately 5% of carriers develop adult T-cell leukemia or lymphoma. Hepatitis C virus (HCV) is associated with the development of clonal B-cell expansions and certain subtypes of NHL (ie, lymphoplasmacytic lymphoma, Waldenstrom macroglobulinemia), especially in the setting of essential (type II) mixed cryoglobulinemia. Kaposi sarcoma-associated herpesvirus (KSHV) is associated with body cavity-based lymphomas in patients with HIV infection and in patients with multicentric Castleman disease [10].
Environmental factors linked to the development of NHL include chemicals, chemotherapy, and radiation exposure. A study by Antonopoulos et al found that maternal smoking during pregnancy may have a modest increase in the risk for childhood NHL but not HL [11]. Congenital immunodeficiency states, acquired immunodeficiency states, and induced immunodeficiency states are associated with increased incidence of NHL and are characterized by a relatively high incidence of extranodal involvement, particularly of the GI tract, and with aggressive histology. Primary CNS lymphomas can be observed in about 6% of patients with AIDS [12].
The American Cancer Society estimated that approximately 72,240 new cases of NHL will be diagnosed in 2017 [13]. Since the early 1970s, the incidence rates of NHL have nearly doubled. Although some of this increase may be attributable to earlier detection (resulting from improved diagnostic techniques and access to medical care), or possibly to HIV-associated lymphomas, for the most part the rise is unexplained. NHL is the most prevalent hematopoietic neoplasm, representing approximately 4% of all cancer diagnoses and ranking seventh in frequency among all cancers. NHL is more than 5 times as common as Hodgkin disease.
There is still increased prevalence of Human immunodeficiency virus infections in Nigeria despite all efforts to reduce and curb the menace which have been linked to non-Hodgkin lymphoma as well as falciparum malaria. Falciparum malaria is a major public health challenge in this part of the World which affects many persons living in Nigeria and increases the chances of exposing someone to non-Hodgkin lymphoma. It is important to carry out this study to understand the level of changes impacted by non-Hodgkin lymphoma on haematological parameters at the point of diagnosis so as to guide the oncologists in the management of non-Hodgkin lymphoma patients and to enlighten the World from this part of the World.
Aim
To determine haematological changes associated to non- Hodgkin lymphoma in subjects in Enugu State, South East, Nigeria.
Materials and Methods
The study was done in Niger Foundation Hospital, Independence Layout, Enugu, Nigeria.
Study design
The study is a hospital based prospective cross sectional study using purposive sampling technique from January 2015 to July 2017.
Subjects
The subjects comprised of a total of eighty (80) subjects, 40 subjects were non-Hodgkin lymphoma patients aged 29-75 years (15 females and 25 males) and 40 (20 females, 20 males) subjects were apparently healthy individuals aged matched as the control.
Ethical consideration
This study was performed in compliance with the guidelines of the Helsinki Declaration on biomedical research on human subjects. It was a prospective study, and confidentiality of the identity of the patients and personal health information was maintained.
Statistical analysis
The results were presented in tables as mean and standard deviation and student t-test used for analysis and the level of significance was set at P<0.05.
Haematological investigation
The haematological investigations were done using Mindray BC-5300. The haematological parameters investigated include total white blood cells, neutrophils, lymphocytes, monocytes, eosinophils, basophils, red blood cells, haemoglobin, packed cell volume, mean cell volume, mean cell haemoglobin, mean cell haemoglobin concentration and platelets.
Results
The Table 1 results showed significant increase (P<0.05) in WBC, Neutrophil, Monocytes, and Eosinophil of the non-Hodgkin Lymphoma (NHL) subjects (16.25±3.7 X109/L, 90.3±5.2%, 2.3±0.3%, 0.4±0.1%) compared to the control (5.23±1.2 X109/L, 67.5±6.7%, 30.7±5.6%, 0.2±0.1%), significant decrease (P<0.05) in Lymphocyte, red blood cell, haemoglobin, packed cell volume, mean cell haemoglobin, mean cell haemoglobin concentration and platelets of the non- Hodgkin lymphoma (NHL) subjects (6.8±1.2%, 3.62±0.68 X1012/L,10.3±1.5g/dl, 30.8±5.1%, 85.0±10.4fl, 28.5±2.3pg, 335.0±21.0g/dl, 208.0±16.0 X109/L) compared to the control (30.7±5.6%, 4.73±0.49 X1012/L, 92.0±15.2fl, 30.0±4.6pg, 350.0±25.0g/l, 250.0±20.0 X109/L) and no significant difference (P>0.05) in basophil of the non- Hodgkin Lymphoma (NHL) subjects (0.2±0.1%) compared to the control (0.1±0.1%) respectively.
Table 1: Showing haematological parameters of non-Hodgkin Lymphoma (NHL) subjects and the control.
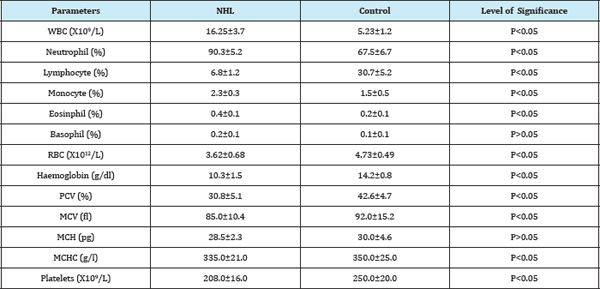
WBC= Total White Cell Count; RBC= Red Blood Cell; PCV= Packed Cell Volume; MCV= Mean Cell Volume; MCH= Mean Cell Haemoglobin; MCHC= Mean Cell Haemoglobin Concentration; NHL=Non- Hodgkin Lymphoma Subjects
Discussion
Rosenberg et al. [14] & Stein et al. [15] have reported that results of haematologic studies are infrequently abnormal in patients with NHL at presentation. However, Bloomfield et al. [16] reported that 57% of patients with NHL have some abnormality in hemoglobin level, leukocyte count, or platelet count at time of diagnosis. The study showed significant increase in total white blood cells, neutrophils, and monocytes of the non-Hodgkin lymphoma and significant decrease in lymphocytes, eosinophils, red blood cells, haemoglobin, packed cell volume, mean cell haemoglobin, mean cell haemoglobin, mean cell haemoglobin concentration and platelets. The decrease in other parameters especially the red cells line and in platelets with red cell indices may lead to anaemia and bleeding disorder. This alteration could be attributable to infiltration of the bone marrow with abnormal cells leading to stress which may be the cause of increase seen in total white cell count, neutrophil and monocytes. These increased white cells could elicit the production and release of cytokines and chemokines which will affect the prognosis of the malignancy. The reduction in the red cell lines may be due to increased destruction of red cells and platelets, pooling to spleen reduced production of blood cells and increased production of abnormal proteins.
Exchange blood transfusion may be of a great help and bone marrow transplant may be option to correct anomaly. Haematologists are needed with the clinicians to make early diagnosis and prompt management of the patients.
Conclusion
The study has shown significant changes in all the haematological parameters studied except the basophils. There was elevation in white cells, neutrophils, and monocytes which could be as a result of stress the body was undergoing. There was reduction in red cells, haemoglobin, packed cell volume, red cell indices and the platelets. Non-Hodgkins lymphoma is associated with anaemia which may be the major cause of deaths in those living with non- Hodgkins lymphoma. Prompt and accurate diagnosis are needed in NHL patients and proper treatment followed immediately.
References
- Cheesbrough M (2004) Lymphoma in district laboratory practice in tropical countries part 2. Cambridge University Press, UK, pp. 292-294.
- PDQ Adult Treatment Editorial Board (2017) Adult Non-Hodgkin lymphoma treatment (PDQ®): health professional version.
- Shustik J, Quinn M, Connors JM, Gascoyne RD, Skinnider B, et al. (2011) Follicular non-Hodgkin lymphoma grades 3A and 3B have a similar outcome and appear incurable with anthracydine-based therapy. Ann Oncol 22(5): 1164-1169.
- Kleihues P, Stewart BW (2003) World cancer report. Lymphoma. Lyon: International Agency for Research on Cancer Press, France, pp. 237-241.
- Sitas F, Parkin M, Chirenje Z, Stein L, Mqoqi N, et al. (2006) Cancers. In: Jamison DT, Feachem RG, Makgoba MW (Eds.), Disease and mortality in sub-Saharan Africa. (2nd edn), World Bank, Washington, DC, USA, pp. 289-304.
- Rosen ST, Winter JN, Gordon LT (2008) Non-Hodgkin lymphoma. In: Pazdur R, Wagman LD, Camphansen KA, Hoskin WJ (Eds.), Cancer management: A multidisciplinary approach. (11th edn), CMP Media, Lawrence, pp. 719-774.
- Tamseela M, Nabila R, Waheed MA (2012) Incidence and clinical manifestation of lymphoma in Central Punjab. Pakistan J Zool 44(5): 1367-1372.
- Friedberg JW, Mauch PM, Rimsza LM, Fisher RL (2008) Non Hodgkins lymphomas. In: Devita VT, Lawrence TS, Rosenberg SA (Eds.), Devita, Hallman, and Rosenberg's Cancer: Principles and Practice of Oncology. (8th edn), Lippincott Williams and Wilkins, Philadelphia, USA, pp. 22782292.
- Oluwasola AO, Olaniyi JA, Otegbayo JA, Ogun GO, Akingbola TS, et al.(2011) A fifteen year review of lymphomas in a Nigerian tertiary health centre. J Health Popul Nutr 29(4): 310-316.
- Marti Carvajal AJ, Cardona AF, Lawrence A (2009) Interventions for previously untreated patients with AIDS-associated non-Hodgkin's lymphoma. Cochrane Database Syst Rev (3): CD005419.
- Antonopoulos CN, Sergentanis TN, Papadopoulou C, Andrie E, Dessypris N, et al. (2011) Maternal smoking during pregnancy and childhood lymphoma: a meta-analysis. Int J Cancer 129(11): 2694-2703.
- Elfström P, Granath F, Ekström Smedby K, Montgomery SM, Askling J, et al. (2011) Risk of lymphoproliferative malignancy in relation to small intestinal histopathology among patients with celiac disease. J Natl Cancer Inst 103(5): 436-444.
- American Cancer Society (2017) Cancer Facts & Figures.
- Rosenberg SA, Diamond HD, Jaslowitz B, Craver LF (1961) Lymphosarcoma: A review of 1269 cases. Medicine 40: 31-84.
- Stein RS, Ultmann JE, Byrne GE, Moran EM, Golomb HM, et al. (1976) Bone marrow involvement in non-Hodgkin's lymphoma. Implications for staging and therapy. Cuncer 37(2): 629-636.
- Bloomfield CD, McKenna RW, Brunning RD (1976) Significance of hematological parameters in the non-Hodgkin's malignant lymphomas. Br J Haemutol 32(1): 41-46.
© 2017 Emmanuel Ifeanyi Obeagu, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






