- Submissions

Full Text
Advancements in Bioequivalence & Bioavailability
Clinical Considerations of Using Extra Acupoints and Traditional Acupoints
Tong Zheng Hong*
Department of Health Sciences, Taiwan
*Corresponding author: Tong Zheng Hong, Department of Health Sciences, Taiwan
Submission: December 14, 2018;Published: February 20, 2019

ISSN 2640-9275 Volume2 Issue4
Abstract
The clinical uses of extra and traditional acupoints represent the application of acupuncture theories. However, the issues like whether or not to combine these two acupoints, timing, and efficacy deserve attention in practice. Expected outcomes cannot occur if Patter identification is not followed.
Keywords: A-shi acupoints; Extra acupoints; Traditional acupoints; Pattern
Introduction
The efficacy of acupuncture for pain relief has been verified with scientific evidence, which enables acupuncture to become popular and accepted in the past years around the world. In addition, acupuncture has also evolved into one of the frequently used healthcare medicines in the West, even though it has only been viewed up to now as the complementary or the integrative medicine in the West [1]. Looking at the historical developments of acupoints, we can understand that acupoints are discovered accidently in the daily life with the specific indications and actions, which are first accepted and recognized as A-shi acupoints. Accepted gradually with time, these Ashi acupoints are systematically analyzed for the indications and actions, and finally incorporated into the meridians.
Acupoints used clinically at present are generally categorized as:
A. Acupoints on the traditional fourteen meridians and
B. Acupoints not located at the traditional fourteen meridians, such as A-shi acupoints and extra acupoints [2].
In addition to the traditional acupoints located on the fourteen meridians, extra acupoints have also gained more attentions. Whether or not the combination of traditional acupoints and extra acupoints can be more effective actually remains uncertain. This article aims to present issues in the clinical uses for acupuncturists to consider.
Issues in clinic
Pattern identification, the process to identify the disharmony between the systems, is truly the unique concept that plays a key in the diagnosis and treatment. Patterns are derived from the Yin- Yang and the Five Elements theories, which sees the human body as a whole miniature of the universe and emphasizes the similarity of the Zang-Fu organs, based on the inductive logic thinking. In other words, the treatment outcomes cannot be expected if an acupuncturist does not strictly follow the specific requirements of the Yin-Yang and the Five Elements theories.
Application of Ying-Yang
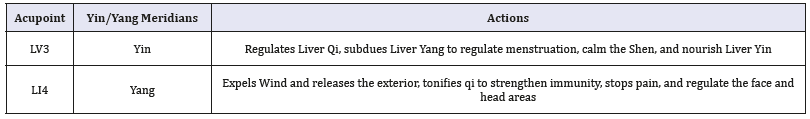
Yin-Yang theory highlights the balance of the Zang-Fu organs. In this theory, the traditional twelve meridians are divided into Yin and Yang meridians, which are subcategorized as three hand and foot Yin and Yang meridians. A disease is the presentation of imbalanced Yin-Yang, in which Yin is defined as materials to fuel the organs and Yang refers to functions of the Zang-Fu organs [3]. The five-shu acupoints located on traditional twelve meridians are also divided into Yin-Yang in accordance with the Five Elements theory. The combination of LI 4 and Liv 3 in (Table 1) is the typical application of Yin-Yang, which is called the Four Gates. Unfortunately, this theory cannot apply to the extra acupoints and A-shi acupoints only for they are not incorporated into the traditional twelve meridians.
Table 1:The Four Gates protocol.
Combination or not
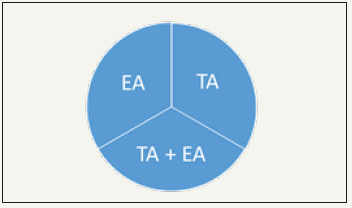
In general, an acupuncturist in practice may face the challenge, considering using the traditional acupoints only, the extra acupoints only, or the combining both traditional and extra acupoints, including A-shi acupoints, as presented in the three-acupointselection protocol in (Figure 1). The indications of extra and A-shi acupoints remains uncertain without scientific evidence; therefore, it is strongly suggested to consider the traditional acupoints first based on the Yin-Yang and the Five Elements theories in the server conditions. The golden rule “Less needling for best outcomes” should be born in mind in order not to make patients uncomfortable. Palpation that facilitates acupuncturists to make diagnosis seems to be the feasible technique for acupuncturists to consider when to combine extra acupoints and A-shi acupoints with traditional acupoints and only select traditional acupoints [4].
Figure 1:Three-acupoint-selection protocol. Note: TA for traditional acupoints on the meridians; EA for extra and A-shi acupoints
Timing
The priority of selecting traditional acupoints and extra and A-shi acupoints for needing is challenging. It is suggested that palpations should be conducted first before making the decisions. In the Decision-making model, the priority can be determined with the palpations.
Efficacy
Whether or not manipulations of sedation and tonification on extra and A-shi acupoints can be used for excess or deficiency patterns deserve attention. The manipulation of lifting-thrusting stimulated on Zusanli (ST36) increased the temperature of the skin [5], which suggests that the scientific evidence of the manipulations is needed to verify if the same result can be applied to extra and A-shi acupoints.
Conclusion
In terms of cost, convenience, and time saving, acupuncture is the top priority for patients. Contemporary scientific evidence shows acupuncture is effective for pain relief, etc.; however, it is surely that expected outcomes and results cannot be obtained if pattern based on TCM is not accurately identified and strictly followed in scientific research and practicing. Without practical guidelines discussed in the literature for acupuncturists to follow in clinical practice, it is expected the issues presented in this paper may be helpful and attract more attentions.
References
- Hong TZ (2018) Notes for clinical use of extra acupoints. J Complement Med Alt Healthcare 8(1): 555728.
- Hong TZ (2018) Reminders for clinical application of extra acupoints. Curr Trends Biomedical Eng & Biosci 16(3): 555939.
- Hong, TZ (2017) Principles of protocol to treat heart blood deficiency. J Complement Med Alt Healthcare 4(4): 555644.
- Hong TZ (2018) Decision-making model proposed in use of extra/a-shi acupoints with traditional acupoints. Advancements Bioequiv Availab 2(2).
- Huang, Tao Huang, Xin Zhang, Weibo Jia, Shu Yong Cheng, et al. (2013) The influence of different acupuncture manipulations on the skin temperature of an acupoint. Evidence-Based Complementary and Alternative Medicine p. 5.
© 2018 Tong Zheng Hong. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






