- Submissions

Full Text
Advancements in Bioequivalence & Bioavailability
A Review for Integrating Western and Chinese Medicines in Primary Dysmenorrhea
Tong Zheng Hong*
Department of Health Sciences, Taiwan
*Corresponding author: Tong Zheng Hong, Department of Health Sciences, Taiwan
Submission: September 16, 2018;Published: November 15, 2018

ISSN 2640-9275 Volume2 Issue1
Abstract
The theories of Ying-Yang, Zang-Fu, the Five Elements and pattern identification in the Traditional Chinese Medicine (TCM) are unique and different from those theories of the Western medicine. Qi stagnation and Blood deficiency can block the channels to cause pain in menstruation. Issues like processing of Chinese herbs, side effects and interactions of TCM herbs and Wester medications need considerations in the integration of these two medicines.
Keywords: Dysmenorrhea; NSAIDs; Blood stasis; Anemia
Introduction
Most people in Taiwan, in general, present themselves to the medical doctors first when they need medical treatments. Part of this fact is because there are not enough scientific researches to prove the effects of the traditional Chinese medicine (TCM), acupuncture, Moxa, cupping, or acupressure. Compared to the current acupuncture developments in Taiwan, acupuncture has gained more and more popularity in the past 40 years and been considered “essential health benefits” in the US and is considered a complementary or alternative role of the medical system in most of the Western countries. [1].
The harmony of Yin and Yang is the key principle TCM focused on and is the core of health because Yin-Yang disharmony can result in diseases. Both Chinese herbs and acupuncture are two common modalities based on the theory related to Yin-Yang balance and guidelines derived from the Five Element theory [1].
Dysmenorrhea occurring before, during, or after the menstrual period is one of the common problems for the women at reproductive ages with the 60-90% of the prevalence rate in the US. The occurrence of menstrual cramps with pain in the uterine counts for clinically 37% of the menstrual dates on average, and ranges from 56.4% to 84.1% in several studies worldwide [2]. The common symptoms of dysmenorrhea are sacral pain, discomfort or pain in the low pelvic region, vomiting, headache, nausea, diarrhea, and low back pain or soreness that can radiate to the anterior thighs, which can start a few days before the onset of menses and the intrauterine pressure increases, and the blood flow to the uterus decreases to cause inflammation [3].
Non-steroidal anti-inflammatory drugs (NSAIDs) like mefenamic acid, ibuprofen, naproxen, and ketoprofen are generally given to patients two days before and can it can continue for up to two days after menses for pain relief or alleviation. However, NSAIDs cannot prevent recurrence of dysmenorrhea at all and the pain usually may begin one to two years after the menarche and finally become severe with time. Low dosage of estrogen-progesterone oral contraceptive is taken into consideration for the ovulation suppression in some cases. Dysmenorrhea, unfortunately, may come back if patients stop birth control pills. Surgery in some server cases could be taken into consideration finally [4].
The result provided by Zhu supports the use of Chinese herbal medicine can relieve pain in primary dysmenorrhea with significantly positive evidence, compared to use of Western pharmaceutical medications [5]. On the other hand, the trend of integrating TCM and Western medicine has begun for long internationally. However, concerns of its efficacy, safety, and potential interactions with Western medications have also increased as well with increasing evidence that shows the important pharmacological effects can be imparted with the interactions of Chinese herbs and Western medications [6].
Fundamental differences between chinese medicine and west medicine
TCM and Western Medicine have been viewed as two distinct and divergent medicines for long with the approaches to physiology and healing techniques. Therefore, the fundamental differences in both Western medicine and TCM need attention when healthcare providers are considering the feasible choices in clinical practice.
In theory: TCM sees the body as a miniature of the universe and in diagnosis and treatment, which is totally different from the Western medicine. Yin-Yang, the Five Element, Qi and Blood are the philosophical concepts and abstract with the functions broader than the anatomical knowledge of the Western medicine. On the other hand, TCM emphasizes mostly the congenital constitution passed from the parents because it can result in “root” problems in health [1].
Western medicine is seeking the minor difference from the perspective of etiology and is concerned about diagnosing and treating the symptoms alone. The theory develops with seeing the organs separately and treating parts of the body like a machine. Each part of the organs has its functions and needs the replacement or resection when a part fails to function normally [1,7].
In practice: The evidence from X-ray, urine, blood, stool tests, CT, and MRI targeted at the pathogen or etiology applied on the human body give the directions for treatment, in addition to taking history and physical examination.
Without the assistance of scientific instruments, TCM doctors only make diagnosis based on symptoms related to the Yin- Yang imbalance rather than diseases itself through analyzing the patient’s tongue, facial expressions, pulse, voice, body reaction, hair, and posture.
It should be noted that the vital key to the successful results is that an experienced TCM doctors or acupuncturists can only depend on four skills for diagnosis and pattern identification to write up the prescriptions. In other words, patterns that distinguish TCM from the Western medicine should be the key concern TCM practitioners and acupuncturists stick to in decision- making of treatments [1,7].
A glance at TCM and western medicine for dysmenorrhea
Blood (Xue) is the nourishing agent which can interact with the moving agent Qi to maintain the functions of the body in TCM [8,9]. Blood, which moistens and nourishes the skin, muscles, sinews, bones and internal organs, nourishes Qi and Qi moves Blood. One is inconceivable without the other, based on the concept in TCM that Qi is the commander of Blood, and Blood is the mother of Qi [10].
The pain shall occur without free flow Qi and Blood. The circulation of Qi and Blood in the body should be constant representing the inter-transforming, inter-dependent, and interpromoting features with the dynamic and interdependent functions of Zang-Fu organs of Heart, Liver, Lung, Spleen, Kidney, and San Jiao shown in Table 1 [11].
Table 1:Functions of Zang organs related to Blood.
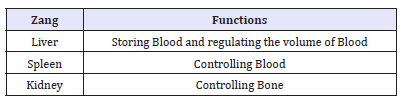
The Liver qi keeps Qi circulate in the body with the connection with Spleen to promote the digestion function for producing Blood. Mechanisms in the disorder of Qi and Blood are external factors like improper exertion in activities, Wind and Heat, negative emotional states, and bad diet [1,11]. External pathogenic factors, dysfunctions of internal Zang-Fu organs, and abnormal emotional states impede both Qi and Blood to circulate freely in the Penetrating and Directing Vessels, which are responsible for the physiology of menstruation. From the aspect of TCM, pain is mainly resulted from Blood deficiency and Qi deficiency, or Blood stasis and the Qi stagnation. The key organs are Liver and Heart. Heart governs the blood, blood vessels, and the root controller of Zang-Fu organs while proper Blood movement is impaired without the free flow of Liver Qi [11].
Liver Qi and Liver Blood are essential for pain relief if they can move freely and properly. Menstruation is identified with duration from the four following phases [12]:
A. Before menstruation: Yang moves Blood, and Liver Qi moves in preparation to move Blood.
B. During mid-cycle: Blood and Yin fill up in the Penetrating and Directing Vessels.
C. During menstruation: Blood moves with the help of Liver Qi and Liver Blood.
D. After menstruation: Blood and Yin are empty.
The pathological perspective of Western medicine indicates the levels of prostaglandins of primary dysmenorrhea elevated is the response to the rise and fall of progesterone after ovulation. Cell membrane fatty acids of the endometrial cells are converted into arachidonic acid with the breakdown of Lysosomes and the release of phospholipase A 2 when progesterone production decreases by the corpus luteum. Uterine hypercontractility, nausea, vomiting, and cramping thus occur with the excessive elevation of prostaglandins. Decreased blood flow to the uterus and the excessive level of hormone Vasopressin can cause contraction and make nerve fibers sensitive to the inflammatory endoperoxides and prostaglandins. [13].
Current treatments in the Western medicine to menstrual pain are bioenergetics therapy, nutrition, botanicals, pharmaceutical, and supplements. Omega-3 Fatty Acids is suggested for modulating painful uterine contractions, inflammation, and the levels of prostaglandins. The prostaglandin synthesis is reduced with the role magnesium plays in the treatment of menstrual pain for its effect on intracellular calcium concentration. This therapy can be given by foods like nuts, leafy greens, fish, and whole grain cereals with supplements suggested like Vitamin E and Vitamin B2 (Pyridoxine) [13].
NSAIDSs like cyclooxygenase (COX)-2 inhibitor like oral contraceptive pills has been considered the first line reactive treatment for the hormonal modulation. However, they can be closely associated with significant side effects to cause gastrointestinal symptoms like nausea and indigestion. It is also pointed out that NSAIDs are associated with higher risk of drowsiness, dizziness, headache, and dry mouth [14].
Discussion
It has been confirmed that acupuncture and TCM herbs can relieve pain effectively in the patients with dysmenorrhea, which seems to remind those who are interested in integrating TCM and Western medicine that safety and efficacy of the integration of TCM and Western medicine should deserve attention [15].
The integrated treatment of TCM and Western medicine for primary dysmenorrhea does not merely refer to putting TCM and medical doctors together at the same time. This model truly means to be “patient first” for the best outcomes. In other words, both TCM and medical doctors should introduce the optimized protocol based on professional discussion and negotiation with patients, according to the patients’ needs.
Terms confused
Blood deficiency in TCM does not equal anemia in the Western medicine, a condition in which the blood lacks enough healthy red blood cells or hemoglobin. From the TCM perspective, Blood acts more than run through the veins and oxygenate cells because it ensures us to have nourishment and moisture for the entire body, including tendons, skin and hair healthy, strong and flexible. In the meantime, it also lubricates joints and allows for smooth movement. With the biological functions stated above, Blood deficiency in TCM mainly refers to volume rather than quality in Western medicine.
Interactions and herb processing
In terms of gynecologic complaints, including dysmenorrhea, Dong quai is popular with Chinese and has been used commonly in TCM formulas on the base of the TCM diagnoses of “blood stasis” and “blood vacuity,” associated with the diagnoses of uterine fibroids, dysmenorrhea, amenorrhea, and endometriosis in Western medicine. However, interaction risks of Dong quai and Western medications deserve attention as in Table 2 [16].
Table 2:Interactions of Dong Quai (Radix Angelicae Sinensis) with Western medications.
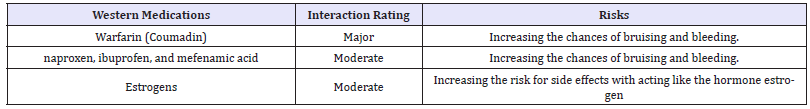
In addition to interactions, side effects can arise from the uses of Western medications. Dampness, which can be caused by Antihistamine and Steroid, is one of the Six Evils in TCM that can induce Blood deficiency and Qi stagnation. The studies reporting that vinegar-baked Radix Bupleuri (VBRB) can enhance the effects of the drugs on Liver and modify drug transport highlight the importance of the processing of Chinese herbs that can change the nature, safety, and action. These two studies remind us that accurate use of proceed Chinese herbs plays an important role that cannot be ignored for the best results [17,18].
It is pointed out that there could not be specific pathological factors in both primary and secondary dysmenorrhea. Recent developments in neuroscience enrich the understanding of pain drive, showing there could be more than one pain drivers in one patient. Multiple mechanisms need healthcare providers’ attentions [15].
Conclusion
Prolonged or habitual emotional disturbance can lead to Liver Qi stagnation in the Penetrating and Directing Vessels, and the Uterus to cause inflammation. From the perspective of TCM, how to avoid obstructions of Qi and Blood which can block the channel, causing pain during menstruation deserves further research.
Literature suggests that it is for sure acupuncture and TCM herbs can control or reach the goal of treating dysmenorrhea effectively as Western medicine. However, integration of Western medicine and Traditional Chinese Medicine for treating dysmenorrhea needs the further consideration of side effects and interactions.
References
- Hong TZ (2017) Exploring a new extra point for sub-acute cough: A case report. Scholar’s Press, Germany.
- Behbahani BM, Ansaripour L, Akbarzadeh M, Hadianfard MJ, Zare N, et al. (2016) Comparison of the effects of acupressure and self-care behaviors training on the intensity of primary dysmenorrhea based on McGill pain questionnaire among Shiraz University students. J Res Med Sci 2: 21-104.
- Lu Y. Treatment of dysmenorrhea with acupuncture and Chinese Herbs-A Case Study
- Tsenov D (1996) The Effect of acupuncture in dysmenorrhea. Akusherstov i Ginekologiia 35(3): 24-25.
- Zhu X, Proctor M, Bensoussan A, Wu E, Smith CA (2005) Chinese herbal medicine for primary dysmenorrhea (Protocol). Cochrane Database Syst Rev 16(2): CD005288.
- Chan E, Tang M, Xing J, Sudarsanam S, Johnson DE (2010) Interactions between traditional Chinese medicines and Western therapeutics. Current Opinion in Drug Discovery & Development 13(1): 50-65
- What are the key differences between T.C.M and Western Medicine?
- Smith CA, Armour M, Zhu X, Li X, Lu ZY, et al. (2014) Acupuncture for dysmenorrhea. Cochrane Database Syst Rev 23(2): 67-73.
- Mc Phee SJ, Papadakis MA (2012) Current Medical Diagnosis & Treatment, Mc Graw Hill, New York, USA
- Sun P (2011) Treatment of pain with Chinese herbs and acupuncture. Churchill Livingstone, NY, USA.
- Zhu B, Wang H (2010) Basic theories of traditional Chinese medicine. People’s Military Medical Press, PA, USA.
- Maciocia G (1994) The practice of chinese medicine: The treatment of diseases with acupuncture and Chinese herbs. Churchill Livingstone, UK.
- Rakel D (2012) Integrative Medicine. ELSEVIER, PA, USA.
- McMahon SB, Koltzengburg (2006) Wall Melzack’s textbook of pain. Elsevier, Churchill Livingstone, UK.
- Chaitow L, Jones RL (2006) Chronic pelvic pain and dysfunctionpractical physical medicine. Elsevier, Churchill Livingstone, UK.
- https://www.webmd.com/vitamins/ai/ingredientmono-936/dongquai
- Ya Z, Feng LM, Liu LJ, Zhang X, Zhao RZ, et al. (2017) Clerosterol from vinegar-baked radix bupleuri modifies drug transport. Oncotarget 8(13): 21351-21361
- Zhao R, Liu L, Wang Y, Xiao Z (2014) Vinegar-baked Radix Bupleuri modulates the cell membrane constituents and inhibits the P-gp activity in rat hepatocytes. BMC Complementary and Alternative Medicine 14: 357.
© 2018 Tong Zheng Hong. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






