- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Valve Vacuum Suction Control in Neurosurgery
Manuel Dujovny1*, Onyekachi Ibe2, Erin Morency3,Channan Kositzke4, Pablo Sosa5 and Fabian Cremaschi5
1 Department of Neurology, Johns Hopkins School of Medicine, USA
2 College of Engineering & Information Science, DeVry University, USA
3 Beaumont Hospital Troy, Oakland Medical School of Nursing, USA
4 Western Michigan University, USA
5 Department of Neuroscience, Clinical and Surgical Neurology, University of Cuyo, Argentina
*Corresponding author: Manuel Dujovny, Department of Neurosurgery, Wayne State University, USA, 733 Bagley Dr, Grand Rapids, MI, 49506, USA
Submission: April 27, 2018; Published: May 14, 2018

ISSN 2637-7748
Volume1 Issue4
Abstract
Suction vacuum control in neurosurgery can be recognized as a contributor to neurosurgical complications. The objective of this article is to highlight physical suction valve vacuum systems and to analyze the valve control system. The suction valve systems reviewed include the total partial block, the orifice bent, and the piston coil. This article provides a brief fluid suction control history as well as a synapse of kinetic theory and its implications. Neurosurgeons who experience increased suction control flow manipulation benefit from increased positive patient outcomes.
Keywords: Suction Vacuum; Pressure; Orifice Bent; Piston Coil Valve; Neurosurgery
Introduction
Central nervous system bleeding and homeostasis control have been challenging to the neurosurgeon from the beginning of this newer specialty. Surgical technique, such as clamping or ligature, cannot be performed successfully in the central nervous tissue. The use of a suction cannula, created by Yankaur and Frazier at the beginning of 1900’s, was quickly associated with surgical treatment of central nervous system diseases as another surgical specialty [1]. Frazier developed a surgical suction with fluid flow which became a significant contribution to many neurosurgical procedures, where zero suction is never reached.
The rubber bulb syringe was originally used for suction and irrigation. This rubber bulb syringe was modified with the insertion of a metallic angle tipped cannula by Adson with different sizes. Following the introduction of the suction pump and hospital suction compressor, the rubber bulb syringe became obsolete and was used for irrigation only [2].
At the beginning of the second decade of the 1900’s, brain suction was introduced by Cushing with the removal of a brain tumor, which replaced the surgical technique of resection of the tumor with scissors, which had a severe mortality and morbidity rate [3]. This new technique of vacuum pressure tissue maceration, associated with the valve syringe irrigation, changed the fate of the brain tumor resection. It was discovered very early that the vacuum suction in neurosurgical procedures induced brain bleeding. The development of numerous neurosurgical techniques around the 1930’s and the introduction of improved diagnostics for cerebral angiography by Agas Moniz and cerebral aneurysm clip helped minimize these complications [4-6].
Treatment of cerebral aneurysms is complicated and involves surgical intervention, but has proven to be a success with the use of neurosurgical vacuum suction equipment and the knowledge of microanatomical structures [7-9]. Surgical interventions include dissection of the dome, neck, removal of intracerebral hematoma and main artery with severe bleeding due to aneurysm rupture or tear in the aneurysm wall during dissection [10]. Lacerations of the perforating arteries in the surgical field need suction to minimize fluid irrigation and blood, which impair the surgeon’s ability to visualize necessary anatomic structures. Similar situations have occurred with intra-cerebral hematoma and post-radiation necrosis of the brain or during spinal cord surgeries.
Although 100 years have passed since neurosurgical specialties appeared, there is still no protection from the vacuum power on the neurosurgical cannula tip.
Materials and Methods
The neurological suction control; valve were analyzed, physics, engineering and surgical were examined. books, journal and PubMed, social media and anecdotal were evaluated.
Results
An analysis shows that suction vacuum pressure is the main cause of central nervous system injury. This can be caused by excessive vacuum pressure. Pressure can be controlled by obstructing the suction cannula, the orifice pressure relief valve, or the use of the piston coil valve, which is the oldest techniques
Discussion
Since early civilization water flow has played an important role in mankind’s discoveries. Mathematical and quantitative formulation of the laws of motion began in the 14th century. Crombie stated that motion is the quantitive relationship between different velocities. Dynamics lead to the development of kinematics and kinetics. Kinematics is a purely mathematical description of motion and kinetics is existing relations between force, mass, and motion of the body. Gerald of Brussel began the field of kinematics, the science of motion, which describes how intensity and velocity vary from one moment to another within a moving body. Thomas Bradwardine gave a mathematical account of the laws of motion describing the relationship among force, resistance, and velocity by looking for a functional relationship between the dependent variable (V) and the two independent variables F (force) and R (resistance). Using the given values for F and R to find the comparable value of V. He reached an equation for the law of motion, which in modern terminology, states that the velocity is proportional to the logarithm of F/R [11]. Different types of forces acting upon fluids, such as viscosity, climatic conditions, barometric pressure, and temperature, and density affect the behavior of the fluid [12]. In 1687, Isaac Newton postulated his laws of motion, conservation of energy and the law of viscosity and density [13]. Poiseuille stated flow is a steady viscous fluid driven by an effective pressure gradient established between the two ends of a long straight pipe of a uniform circular cross-section. Using the Poiseuille law, an equation for the flow rate through a pipe can be calculated P x 3.14 x r4 ÷ 8 x η x ∫ = Flowrate Where: P is pressure, η the viscosity of the fluid, r the radius of the tube ∫ is the length of the tube, 8 and 3.14 are constants [14]. Flow control in science was first introduced by Prandtl in 1904, where he introduced the boundary layer theory, which was the beginning of ideas to control a flow field [15].
In general science, a valve is a device that regulates, directs, or controls the flow of a fluid (gases, liquids, fluidized solids, or slurries) by opening, closing, or partially obstructing various passageways [16].
In neurosurgery three fluid valve control have been reported; total or partial at rest of fluid control, orifice pressure relief, and coil piston. The insertion of surgical patties between the suction tip and the central tissue, the changes of the formation of the suction tip, the insertion of the cotton fiber or a tip all are ways to manipulate surgical suction [17]. The neurosurgical patty (also known as a surgical sponge or cottonoid) is a disposable textile pad for fluid management, homeostasis, and tissue manipulation. Surgeons prepare the cotton patty according to their preference in order to control the bleeding
Anecdotally, we analyzed the method of occluding vacuum flow, which can be partial or by blocking the cannula tip. According to the Bernoulli principle, the fluid flow will be faster in a narrower pipe than in a wider channel. The early protection of the Central Nervous System structure was with the use of clothes, it was also common during this early period to use clamping or external compression (kinking), mechanical pedal compression as described by Jefferson et al. [18].
A newer designed cottonoid by Arbit is fixed to the tip of a suction device by the negative pressure. This device has been efficient during microsurgical procedures in areas crowded with neurovascular elements [19]. Lafranc et al. [20] described a latex-free aspirator tip attachment designed for spinal cord tumor resection to help prevent surgical traumas in spinal cord surroundings [20]. Menovsky described an atraumatic suction tip that facilitates atraumatic suction in microsurgery and Mariak et al. [22] describe an atraumatic neurosurgical suction tip during micro neurosurgery to minimize injuries to the brain structures and protect the brain tissue from being aspirated into the suction tube. The simple flow measurement is considered to be the volume of the fluid, to the suction, multiplied by the force of suction, and divided by the resistance. Electrical mechanical suction and wall pressure gauges can be controlled by operating room personnel [21,22].
The vent orifice pressure relief valve was the first valve used in neurosurgery, the pressure relief of suction is graduated by the size of the vent and the number of the relief areas [23]. This technique allows the surgeon to move their finger to occlude the orifice vent which allows for a maximum increase of flow to minimal fluid reduction, placing the thumb on the proximal portion of the suction handle when the vent is occluded. It was introduced by Frazier and become the most commonly used suction cannula, Frazier also originally utilized the single orifice pressure relief valve system [23] (Figure 1).
Figure 1: Frazier Cannula, Orifice Pressure Relief Valve.
Nishizaki and Dujovny utilized a multiple orifice pressure relief valve [24,25]. Gusmao describes a suction cannula with multiple small holes at the proximal end with a lateral sliding bar to open or close the holes [26]. A malleable plastic cannula for readjustment of the suction tip by Spetzler, this canal can be arresting with a surgical clamp, also closing the pressure gage (Figure 2). The size of the vent of the cannula determines the amount of pressure relief. Another variation is the placement of the orifice toward the tip of the cannula, like the Dujovny bayonet style suction with the orifice on the distal end, or distal barrel, for microsurgical procedures [27] (Figure 3).
Figure 2: Suction Pump and Canister, Pump Gauge Monitor.

Figure 3: Clamp Hemostat.

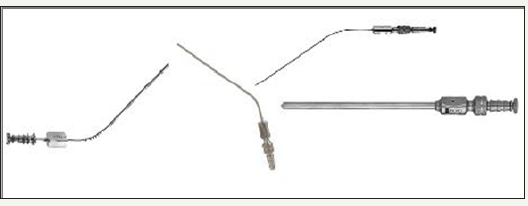
Figure 4: Interchange Suction Cannula, Bayonet Adapter, Piston and Suction Handle, Triangle Hole in the Piston

In 1976, Dujovny introduced three portions of the vacuum cannula. The cannula, the bayonet device, and a box handle for the section for the piston valve (Figure 4). Streamlining the piston’s internal coil and fluid control changed it to a versatile instrument, the handle was enlarged to hold a hollow piston with the coil attached to the bottom or to a special coil [28]. This equipment connects to the bayonet modification for microsurgical procedures and is welded directly to the cannula with a round hole in the piston to communicate with the cannula. In 1978 an improved modified suction valve with a triangular shape where the coil was at the surface of the piston was described by Barrinuevo et al. [29]. A modification was introduced, this device has an inverted triangle hole to control the flow, was created with plastic where the handle encased coil with the piston is integrated. The piston coil on the top allowed the surgeon to maneuver between complete suction, gradual suction, or instantaneously stoppage of suction. A new housing for the suction control valve of the piston coil allows for manual changes, with the potential for full suction, to meet the surgeon’s requirements. The piston coil allows the surgeon a prompt acceleration and can manually calibrate deceleration of suction to zero [30].
Conclusion
The analysis of fluid control in fluid mechanics, velocity control, and fluid valve controls are manually controlled by the neurosurgeon. There are three main valve controls in neurosurgery; partial or total fluid control, orifice pressure relief valve, and piston coil valves. With the development of nanotechnology, nanotubing, and nano-monitoring there may be a potential in the future to obtain better flow fluid control, improve suction safety and reducing surgical morbidity.
Disclosure Statement
The authors report no conflict of interest concerning the materials or methods used in this study or the findings specified in the paper. The article is original and has not been previously published. It is not under consideration for publication elsewhere. The authors received no monetary compensation based on the information provided.
References
- Rhoton AL Jr, Merz W (1981) Suction tubes for conventional and microscopic neurosurgery. Surg Neurol 15(2): 120-124.
- Temple Fay MD (1927) A new instrument combining suction and irrigation for intracranial surgery, JAMA 89(1): 25-26.
- Cushing HW (1915) Concerning the results of operations for brain tumor. JAMA LXIV: 189-190.
- https://www.youtube.com/watch?v=6Pm2KNyVcG0
- Dujovny M, Ibe O, Perlin A, Ryder T (2010) Brain retractor systems. Neurol Res 32(7): 675-683.
- Dujovny M, Agner C, Ibe O, Perlin A (2010) Self-closing aneurysm clip: a historical review. Neurol Res 32(10): 1011-1020,
- Umansky F, Gomes FB, Dujovny M, Diaz FG, Ausman JI, et al. (1985) The perforating branches of the middle cerebral artery. A microanatomical study. J Neurosurg 62(2): 261-268.
- Pedroza A, Dujovny M, Ausman JI, Diaz FG, Cabezudo Artero J, et al. (1986) Microvascular anatomy of the interpeduncular fossa. J Neurosurg 64(3): 484-493.
- Sosa P, Dujovny M, Onyekachi I, Sockwell N, Cremaschi F, et al. (2016) Microvascular anatomy of the cerebellar parafloccular perforating space. J Neurosurg 124(2): 440-449.
- Barrow DL, Spetzler RF (2011) Cotton-clipping technique to repair intraoperative aneurysm neck tear: a technical note. Neurosurgery 68(2 Suppl Operative): 294-299; discussion 299.
- Freely J (2010) Before Galileo: The birth of modern science in medieval Europe. (Chapter 8), Overlook, John Wiley & Sons, New York, USA, pp. 153-173.
- White FM (2007) Fluid Mechanics. (6th edn), McGraw-Hill International Edition, New York, USA, pp. 1-602.
- Newton I (1991) The Principia: Mathematical Principles of Natural Philosophy, University of California Press, USA, pp. 1-991.
- Lamb B (2014) The Principles of Vacuum And Clinical Application in the Hospital Environment. Ohio Medical Corporation, USA, p. 28-29.
- Martin H (2002) The generalized Lévêque equation and its practical use for the prediction of heat and mass transfer rates from pressure drop. Chemical Engineering Science 57(16): 3217-3223.
- http://www.businessdictionary.com/definition/valve.html
- Stratton-Powell AA, Anderson IA, Timothy J, Kapur N, Culmer P (2015) Neurosurgical patties: adhesion and damage mitigation. J Neurosurg 123(1): 153-160.
- Jefferson A (1967) Footpiece for suction control. J Neurosurg 26(4): 448.
- Arbit E (1982) Pressure-mounted cottonoids: technical note. Neurosurgery 11: 786.
- Menovsky T, De Ridder D, de Vries J (2009) Neurosurgical patties and their intraoperative interaction with neural tissue. Surg Neurol 71(3): 326-329.
- Lefranc F, Brotchi J (2007) Performance of a new type of suction tip attachment during intramedullary tumor dissection: technical note. Neurosurgery. 61(5 Suppl 2): E241.
- Mariak Z, Lyson T (2007) Atraumatic suction tip for microneurosurgery- -clinical experience. Minim Invasive Neurosurg 50(6): 379-381.
- Dandy Walter E (1969) The brain; Prior, pp. 1-682.
- Nishizaki T, Wakabayashi T (1985) A self-retaining multipore suction tube. Technical note. J Neurosurg 63(2): 304.
- Dujovny M, Vas R, Osgood CP, Maroon JC, Jannetta PJ (1975) Automatically irrigated bipolar forceps. J Neurosurg 43(4): 502-503.
- Gusmão S (2005) A new device with pressure regulation for microsurgical suction: technical note. Surg Neurol 63 Suppl 1: S36-S38.
- Spetzler RF, Iversen AA (1981) Malleable microsurgical suction device. Technical note. Neurosurg 54(5): 704-705.
- Dujovny M, Barrionuevo PJ, Laha RK, DeCastro S, Maroon JC (1976) Experimental middle cerebral artery microsurgical embolectomy. Surgical Forum 27(62): 495-496.
- Barrionuevo PJ, Dujovny M, Maroon JC, Kossovsky N (1978) Adjustable control suction valve. Surg Neurol 9: 253-254.
- Dujovny M, Barrionuevo PJ, Osgood CP, DeCastro S, Maroon JC, et al. (1978) Experimental middle cerebral artery microsurgical embolectomy. In: Schmiedek P, et al. (Eds.), Microsurgrey for Stroke. Springer-Verlag, New York, Heidelberg, Berlin, USA, p. 91-97.
© 2018 Manuel Dujovny. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






