- Submissions

Full Text
Intervention in Obesity & Diabetes
Evaluation of State’s School Policy on Childhood Obesity: Quasi-Experimental Study
Tetsuji Yamada1, Chia-Ching Chen2, I-Ming Chiu3, Joseph R Harris3, John Carter4, Straso Jovanovski5 and Britney Dang6
1Department of Economics, Rutgers University, the State University of New Jersey, USA
2Department of Public Health, New York Medical College School of Health Sciences & Practice, USA
3Department of Economics, Rutgers University, the State University of New Jersey, USA
4College of Computing & Informatics, Drexel University, USA
5Rohrer College of Business, Rowan University, USA
6Department of Economics and Department of Computer Science, USA
*Corresponding author:Tetsuji Yamada, Department of Economics, Rutgers University, the State University of New Jersey, 311 North Fifth Street, Camden, NJ 08102, USA
Submission:October 09, 2023;Published: March 12, 2024

ISSN 2578-0263Volume6 Issue4
Abstract
The study assessed the effects of various state obesity programs, including obesity-related school standards, obesity-related program options, and obesity-related state initiatives, and was incorporated into the context of a behavioral model using data from the National Survey of Children’s Health and Behavioral Risk Factor Surveillance System by the C.D.C. The implementation of state obesity programs is likely to reduce childhood obesity. State enforcement of health education in schools is the most effective program option in obesity-related school standards. For obesity-related state program options, the dominant program is associated with private insurance coverage for obesity treatment and prevention. The obesity-related state programs are better targeted towards obese Hispanic and African American children than obese white children.
The obesity burden is concentrated more heavily in white children who live in states with fewer obesity-related state programs than Hispanic and African American children. Unlike African American children, obese Hispanic and white children are more evenly spread throughout income levels. Sports activities, exercises, and T.V./video watching are strongly associated with children at risk of obesity. The effects of after-school sports activities on obese and overweight children are about four times larger than those of unstructured physical exercises. T.V./video watching hours demonstrated that an increase in one hour per day of watching T.V./video on a school day would increase obesity in children by 4.1% (aged 6-12 years old) and 7.3% (aged 13-17 years old). An important contribution to the literature is the finding that state health education enforcement is a prime and effective tool that will guide the scale and scope of the local obesity epidemic of school children. Obesity-related state programs are more effective for African American and His-panic children than white children.
Keywords:Childhood obesity prevention; Obesity programs; USA
Introduction
An increasingly imperative issue in the United States is the increasing incidence of childhood obesity. “Obesity” is defined as the accumulation and storage of excess body fat. At the same time, “overweight” is weight over a weight reference standard [1]. Childhood obesity prevalence has become a great nontransferable harmful illness in recent years, with ever-increasing proportions of children falling into the obese grouping. Obesity has become a major public threat to children’s quality of life. It would raise healthcare costs in the long-run future. Studies have shown that child-hood obesity causes significant medical, psychosocial, and neurocognitive abnormalities. They may continue to adulthood and cause adverse cardiovascular consequences or other obesity-related adverse health risk [2-4]. Obesity among youths is on the rise nationwide. Obesity in youths leads to unhealthy physical and mental health and severe health conditions such as type 2 diabetes, high blood pressure, in-creased risk for heart disease, stroke, cancer, etc., [5,6]. According to the Centers for Disease Control and Prevention (hereafter referred to as C.D.C.), the prevalence of childhood obesity has tri-pled during the period 1980 to 2006 and reached 19.7% in 2020 [7]. The annual medical costs of childhood overweight and obesity were $237.55 per capita and $1975.06 for hospitalizations and annual costs, with long-run healthcare costs estimated to be $49.02 billion by 2050 [8].
The U.S. Preventive Services Task Force (USPSTF) reviewed behavioral interventions for targeting lifestyle and behavior change (e.g., counseling on a diet, increasing physical activities, or decreasing sedentary behaviors emphasizing the effectiveness of early detection and interventions through monitoring for children and adolescents and weight management by primary care physicians [9-11]. Differences in race, gender, and poverty contribute to childhood obesity. The major factor is the socioeconomic position of children’s protection against morbid and severe obesity [12-14]. Other important findings have lit the way toward an overall solution by identifying factors and behaviors that enable the unchecked advance of childhood obesity [15]. Much has been done in the health and sociodemographic areas to examine the root of obesity. However, findings alone are not enough. Without a unified program effort, these findings may go to waste. The U.S. finds itself in a precarious position regarding this public health issue. Battling child-hood obesity contains multi-level components: behavioral goal setting and behavioral modification, changes in the environment, and simultaneously focusing on physical activity and dietary changes [4,16]. The Federal government is mandated to protect public health by instituting programmatic solutions to public health problems. But the issue is tangled in which the government steps into the program [4,16]. Federal intrusion into the public-school systems is impossible as these are in state-level purview. The Federal government cannot directly intervene in the home environment either, as it cannot force parents to provide nutritious meals or make children participate in physical activities. The issue truly constitutes a state recognition and implementation of programs aimed at the childhood obesity epidemic. The critical gap is the lack of understanding regarding the roles and the influences of practice factors in obesity that contribute to health disparity among children. This provides a unique opportunity to examine the efficacy of state programs vis-à-vis childhood obesity. Additionally, it provides a method to examine which types of state programs work and the effectiveness of state-obesity-related programs.
State programs aimed at combating childhood obesity are varied, not only in scope but in implementation as well. As the issue of childhood obesity has grown over the past decade, constituents have become more aware of the issue. However, it has not become an overtly political issue. This lack of public focus has created an environment of unequal recognition of the problem amongst different states [17,18]. According to Health People 2020, one of the objectives is to in-crease the number of states with state-level policies to incentivize food retail outlets to provide foods encouraged by the Dietary Guidelines for Americans. However, according to the Midcourse Review [18], the objective was unmet. Although there is encouraging evidence for the efficacy of policy and environmental intervention strategies, there is limited understanding of the pathways from promising policy and environmental changes to demonstrated reductions in the prevalence of childhood obesity and the marked sociodemographic disparities in its prevalence and its health and economic tools [8,15,19]. Legislation involving public schools and childhood obesity falls into three categories: physical education, health education, and nutritional/food standards; physical activity behaviors and neighborhood environment significantly influence obesity among children and their par-ents/ caregivers [7,12,20]. Physical education has been studied and is highly statistically significant in many childhood obesity studies. It is a prominent program area to focus on as it has the potential to produce higher benefits for childhood health directly. Implementing health education is typically a long-run investment in overall health. However, it can deliver short-term benefits by arming children with the necessary information to raise health awareness of obesity [21].
Educational interventions are effective in treating, but not preventing, childhood obesity and its consequences (specifically diastolic blood pressure) and the high heterogeneity among studies, various educational programs conducted, and the low quality of included studies, including trials with more comprehensive and specific strategies, are needed to improve these results [11,22,23]. Modifiable factors explain childhood obesity disparities. Nutritional and food standards are the most challenging legislative aspects. Various stakeholders may be arrayed against a change in the status [7]. Children spend half of their waking hours in the school setting, and the recent advent of schools offering both interventions and strategies in the target area of physical activity is the most essential obesity intervention [7,24]. The subject of obesity studies shows that influential factors shape daily diet and physical activity behaviors in children and adolescents, suggesting that successful prevention and treatment of childhood overweight/obesity must discourse on leading factors together. Poor choices that stem from socioeconomic factors or unhealthy habits that lead to obesity can modify the performance of genetics in children. Unhealthy diets halt the Sirtuin1 (Sirt1, anti-aging) gene, which is calorie sensitive, disrupting the epigenetic processes that assists the immune system alteration [25]. Food intake and calorie restriction should be monitored to regulate appetites to balance Sirt1 to ensure the interaction between various health factors that prevent Multiple Organ Dysfunction Syndrome (MODS) [25,26]. Mostly aiming to maintain the Sirt1 gene in both the brain and liver. Therefore, a healthy low-calorie diet without harmful substances and active lifestyle should be introduced early on to reduce the aging process in organs and minimize mutations associated with aging [27].
Various federal and state agencies have addressed and implemented guidelines, strategies, and programs to reduce and prevent obesity in children. The association between childhood obesity and programs is undeniable regardless of their effectiveness. However, the effectiveness of interventions and actions is not clear. Understanding the predictive factors associated with childhood obesity and improving children’s quality of life are vital for preventing and managing the epidemic. Evaluating obesity-related state health program implementation through a comprehensive comparison of the interfaces and interactions between various sociodemographic and economic variables is essential. First aim: this study evaluates various program impacts on children to prevent childhood obesity. The study uses three types of state-related obesity programs: obesity-related school standards, obesity-related state program options, and obesityrelated state initiatives, and compares their different influences on child obesity. Second aims: this study examines distinct factors that cause obesity in children and adolescents by applying an extended PRECEDE-PROCEED model (here-after referred to as the P.P. model). Third aim: the study employs concentration indices to examine the influence of state programs on different races about health, i.e., obesity and program disparities.
Methods
Data source and samples
The study assessed the effects of various state obesity programs, including obesity-related school standards, obesityrelated program options, and obesity-related state initiatives. It was incorporated into the context of a behavioral model using data from the National Survey of Children’s Health and Behavioral Risk Factor Surveillance System by the C.D.C. The data was derived from the 2011-2012 National Survey of Children’s Health, a national telephone survey conducted 2011- 2012 by the C.D.C. and Prevention, National Center for Health Statistics, and was sponsored by the U.S. Department of Health and Human Services Administration, Maternal and Child Health Bureau. The survey was designed to (1) estimate national and state-level prevalence for a variety of child health indicators, (2) generate information about children, families, and neighborhoods, and (3) provide baseline estimates for federal and state performance measures. A total of 102,353 surveys completed nationally by parents/caregivers of children and youth ages 0-17 years were collected. Survey results are weighted to be the population of non-institutionalized children and youth ages 0-17 years in each state. Topics include demographics, physical and mental health status, health insurance, access and use of healthcare services, early childhood-specific information, family health activities, parental health status, and beliefs of neighborhood characteristics.
Table 1 shows the characteristics of two groups stratified according to weight status category. The weight status category of obesity is “equal to or greater than the 95th percentile,” and overweight is “85th to less than the 95th percentile”. The 7,050 children (ages 6-17) represent 60.4 % of the total number of obese children, and the 5,484 children stand for 54.2% of the total number of those who are overweight.
Measures
Body Mass Index (BMI) is calculated from a child’s weight and height. B.M.I. is a reliable indicator of body fat for most children. Percentiles are the most commonly used indicators to assess individual children’s size and growth patterns in the United States (C.D.C., 2009a). The weight status category of obese is “equal to or greater than the 95th percentile,” and overweight is “85th to less than the 95th percentile.” The percentile shows the relative position of the child’s B.M.I. number among children of the same sex and age. This study divided the children into two age groups: children aged 6-12 and aged 13-17. Various federal and state agencies have addressed and implemented guidelines, strategies, and programs to reduce and prevent obesity in children. This study employed seven obesity-related state programs, as shown in Table 1. Of these seven programs, this study evaluated three obesity-related school standards: the first one is state enforcement of health education; the second one is nutrition standards for school meals and snacks that go beyond existing USDA requirements; and the third one is limitations beyond federal requirements on when and where competitive food products are sold. Competitive foods refer to all foods and beverages available or sold in schools, except for items served through the national school lunch and breakfast programs.
This study examined two obesity-related state program options: one is provisions for strengthening private health insurance coverage for obesity prevention, and another one is treatment and legislation or resolutions to create obesity-related task forces in Table 1; [28]. There is coverage for surgical treatment of obesity and healthcare visits related to obesity treatment by healthcare providers. Children may or may not be covered. Suppose a patient is obese without complications (such as high blood pressure, high cholesterol or lipids, high blood sugar, etc.). In that case, a counseling visit with a provider is reimbursed. Pharmacotherapy and surgery are options for obese patients. Legislation or resolution creates obesity-related task forces, commissions, studies, or other special programs [29]. State legislation holds three major obesity-related task forces with three components. First, nutrition-related topics include nutrition standards in schools and nutrition education. Second, the legislation incorporates physical education or physical activity in schools. Third, the most challenging task is T.V. viewing and video game use.
This study examined two obesity-related state initiatives in Table 1: one is laws that limit liability for obesity and obesityrelated health problems, and another one is whether the state is a Federal STEPS grant recipient. The STEPS programs, called C.D.C.’s Healthy Communities Program, are community-based and prevent and control chronic disease. The C.D.C. supports states, cities, and communities and focuses on reducing the burden of diseases; overweight, obesity, and asthma by addressing three related risk factors: physical inactivity, poor nutrition, and tobacco use. To evaluate the effects of obesity-related state programs on obese children, this study used the concentration index approach. Before the analysis, dimensionality and reliability analyses were performed to assess whether each program could be used for the concentration index. Using the item reduction method, the initial eigenvalue for all seven programs variable is greater than 1, and the eigenvalues drop toward later components and Cronbach’s coefficient alpha, based on standardized items (α=0.699), was also examined [30]. Subsequently, seven items of the obesity-related state programs (listed under Obesity-Related State Program in Table 1) were summed to create a composite scale whose scores ranged from 0 to 7 for the concentration index analysis.
Table 1:Characteristics of obese (BMI≥95th percentile) and overweight (85th percentile< BMI < 95th percentile).

Analysis
Health behavior is a function of the availability of healthcare services, the demand for healthcare services, and the institutional framework that regulates and oversees the healthcare market. The obesity-related school standards, state program options, and state initiatives of healthcare-seeking behaviors are integrated into a structural model. The line of research on health behavior and its program implications originated from the use of an extended PRECEDE-PROCEED model (hereafter referred to as the P.P. model) postulates that health outcomes are attributed to the child’s behavior based on obesity-related state programs [19,31]. The P.P. model accounts for sociodemographic, reinforcing, enabling, and predisposing factors in Figure 1. By applying behavioral theory, those mentioned earlier, seven obesity-related state programs as the reinforcing factors related to child obesity are incorporated with the P.P. model framework. Enabling factors are comprised of access to healthcare facilities, availability of healthcare resources, health insurance, etc. This study employed received needed care variables as availability of health care services, the State Child Health Insurance Program (SCHIP) as health insurance, and residence of metropolitan statistical areas as an accessibility measure of health care services. Predisposing factors of the P.P. model include knowledge, personal attitudes, values, beliefs, and perceptions. This study included sports activities after school or on weekends, exercises, or participation in physical activities, and T.V. and video watching or video game playing. In this study, the P.P. model contains sociodemographic factors: gender of children aged 6-17 years old, two age groups ages 6-12 and 13-17 years old, US-born children, US-born mother, health status, education attainment as health knowledge, and household income level. Table 1 illustrates the characteristics of the variables mentioned above.
This study employed the Concentration Index (CI) to evaluate health and program disparities. The CI evaluates children ranked not only by their health, e.g., obesity but also by their socioeconomic status, beginning with the most disadvantaged [32]. The CI is the most appropriate measure of program influences on childhood obesity and health, i.e., obesity and inequality among children with different racial/ethnic and socioeconomic backgrounds. The CI is used to quantify the degree of obesity program inequality in the obesity of children. This analysis of childhood obesity is focused on horizontal equity and is not concerned with vertical issues [33].
Results
Table 2 shows the results from the logit regression of the factors associated with obesity among children. All of the results reported in Table 2 used heteroskedasticity-robust standard errors, so heteroskedasticity does not threaten the internal validity of the multiple-regression analysis with the definition of variables in Table 1. The Variance Inflation Factors (vif) for the obese and overweight groups’ regressions range from 5.74 to 7.91 in Table 2. All vifs are less than 10. As a rule of thumb, when analyzing standardized data, a vif <10 indicates a non-harmful multicollinearity [34].
Sociodemographic factors and figure 1
In Table 2, for sociodemographic factors, child gender is statistically significant for obese and overweight children regardless of age differences, and male children are more likely to be obese than female children. Taking the antilog of 0.38 of the obese aged 6-12 and 0.83 of the obese aged 13-17, male children tend to have a higher probability of being obese than female children, 46.2% and 129.3%, respectively. The results for US-born children and mothers do not show systematic, clear-cut evidence between being obese or overweight within the two age groups. An increase in household income is more likely to reduce being obese or overweight for both age groups. However, the results for the educational attainment of households as a proxy for the health knowledge of parents do not show a clear-cut influence on childhood obesity.
Figure 1: Extended PRECEDE-PROCEED Model: Health outcomes and child’s behaviors based on obesity-related state programs.
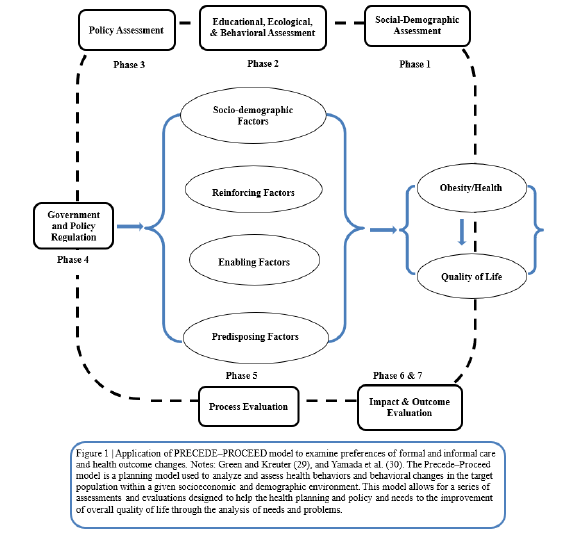
Reinforcing factors: obesity-related state programs and figure 1
In Table 2, this study’s primary parameter of interest is the influence of obesity-related state programs as reinforcing factors on being obese or overweight and their differential impacts on children. Interestingly, all coefficients of the state enforcement of health education are statistically significant in measuring obesityrelated school standards. The influence of the state enforcement of health education on children 13-17 years old is greater than on those 6-12 years old. The effects of a unit increase in the state health education requirement on the decrease in obesity are by 28.4% (-0.25 of the obese aged 6-12 years old) and by 46.2% (-0.38 of the obese aged 13-17 years old) by taking the antilog. Similarly, the impacts of the state health education requirement on the decrease in being overweight are 20.9% for ages 6-12 and 39.1% for ages 13-17. The obesity-related health knowledge administered through school health education is exceptionally powerful for children. The next influential program is also associated with the obesity-related school standards for nutrition of school meals and snacks that go beyond existing USDA requirements. The effects of nutritional standards for school meals are that program implementation decreases the probability of obesity for children aged 13-17 and overweight children aged 6-12. In this study, the limitation on competitive food products sold in obesity-related school standards does not reveal a significant influence on childhood obesity.
Table 2:Factors associated with obesity and overweight among children: Logit regression results. Note. Coef.=coefficient; CI=confidence interval; Ref=reference group. a: p< 0.001; b: p<0.05; c: p<0.01.

For obesity-related state program options, the dominant program is associated with private insurance coverage for obesity treatment and prevention. Health insurance coverage is more likely to reduce obese and overweight children. The state program option is statistically significant for obese and overweight children aged 6-12. It has a comparable influence on reducing obesity. The obesity-related task force does not consistently affect children with obesity and overweight. For obesity-related state initiatives, laws for obesity-related health problems and legal proceedings are more likely to reduce obesity for children aged 6-12 and overweight children aged 6-12. The results of the Federal STEPS programs do not reveal a considerable influence on childhood obesity. However, the C.D.C. supports states, cities, and communities and focuses on reducing the burden of overweight and obesity.
Enabling and predisposing factors and figure 1
In Table 2, interesting results are received needed care and residence within the M.S.A. in the enabling factors. A decrease in unmet needs is more likely to reduce the number of overweight children in both age groups. Children residing within M.S.A.’s have better access to health care than those in rural areas. Obese children in the M.S.A. areas are less obese than children in rural areas, implying that healthcare accessibility is essential for obese children of both age groups. In predisposing factors, sports activities, exercises, and T.V./video watching are statistically significant and prove consistent effects on children with obesity and overweight. The study estimated that a unit increase in sports activity would reduce the probability of obesity by 24.6% (0.22 of the obese aged 6-12 years old) and 40.5% (0.34 of the obese aged 13-17 years old) by using the antilog. The effects of sports activities after school or at weekends on obese and overweight children 6-12 and 13-17 years old are about four times larger than those of unstructured physical exercises. T.V./video watching hours are strongly associated with children being at risk of being over-weight or obese. An increase in one hour per day of watching T.V./video on an average school day would increase obesity in children by 4.1% (0.04 of the obese aged 6-12 years old) and 7.3% (0.07 of the obese aged 13-17 years old). The impacts of T.V./video watching on overweight children are comparable to those for obese children.
Disparity of obesity and obesity-related state program
The Concentration Index (CI) is defined as the Concentration Curve (CC), which is graphed on the horizontal axis as the cumulative percentage of the population ranked by income beginning with the lowest and on the vertical axis as the cumulative percentage of obesity of children by race corresponding to each cumulative percentage of the population of the income in Figure 2. The CI is positive when the CC lies below the diagonal and negative when it lies above. The lowest value of the CI, -1, implies that all the obese children are concentrated in the lowest household income level. The maximum value of the CI, +1, implies that obese children are concentrated in the highest household income level. Figure 2 presents that the CC of African American SCHIP children is lowest among the three measures, and the obesity burden is concentrated more heavily and unevenly amongst African American children relative to Hispanic and white children. All C.I.s are statistically significant, and interestingly, obese African American SCHIP children are more concentrated in high-income households. In contrast, obese white SCHIP children are more evenly concentrated in different income levels. The indices below Figure 2 show the value of the C.I.s measure for the disparity of obese children among racial groups.
Figure 2:Concentration curves: household income and obesity by SCHIP children in different races. Notes: Concentration Index (CI) is the formula/covariance method. The CI of African American children is 0.141a (0.009); the CI of Hispanic children is 0.085a (0.012); and the CI of white children is 0.079a (0.006). Standard error: Standard errors of the concentration index using formula/covariance method. a, b, and c represent statistically significant levels of 99% level (a), 95% level (b), and 90% level (c) for a two-tailed test.

Figure 3:Concentration curves: obesity programs and obesity by different races. Notes: Concentration index (CI) is the formula/covariance method. The CI of African American children is 0.081a (0.005); the CI of Hispanic children is 0.058a (0.004); and the CI of white children is -0.086a (0.004). The program measure is the sum of seven obesity-related state programs that each state implemented in the reinforcing factor of this study. Standard error: Standard errors of the concentration index using formula/covariance method. a, b, and c represent statistically significant levels of 99% level (a), 95% level (b), and 90% level (c) for a two-tailed test.

In Figure 3, the magnitude of a relative disparity depends on the magnitude of the reference point from which the disparity was measured. The CC of African American children lies below the CC of Hispanic children, both below the equality diagonal. The index expresses the size of an ab-solute disparity between races in terms of program influence measured by the shape of the curve. The CI of African American children is 0.081a (0.005); the CI of Hispanic children is 0.058a (0.004); and the CI of white children is -0.086a (0.004). Both CCs are positive, and the value of the CI of African Americans is larger than the Hispanic one. The obesity-related state programs are heavier among African American children than Hispanic children. White children are negative, and the CC lies above the diagonal. The obesity burden is concentrated more heavily in white children who live in states with fewer obesity-related state programs than Hispanic and African American children. Obese white children are also in higher proportion amongst states that have implemented few obesity-related state programs than amongst states with leading obesity programs. The results of each obesity-related state program were distinctly enunciated for obese African Americans.
Discussion and Implications
There is little doubt that the incidence of obesity and overweight in children is increasing in absolute and relative terms. Recent studies provide some opening evidence about racial/ethnic and income differences among children [1]. The effects of physical activity and diet are well-known facts [12]. However, evidence of differential outcomes has been inconclusive. This study attempts to explain the full range of factors and how they contribute to the relationship between obesity-related state programs and obesity disparities among African American, Hispanic, and white children. It also tries to fill in a critical gap within literature. The statistics of this study illustrate that as children age, their average physical activity level declines. In contrast, sedentary activity levels rose; sports activities declined from 64% (6-12 years old) to 60% (13-17 years old); physical exercise per week declined from 4.3 days to 3.6 days; and T.V./video watching rises from 1.4 to 1.6 hours per day. This study’s findings confirm that gradual lifestyle changes would reduce the risk of obesity and becoming overweight among children [15,20]. The adverse effects of risky lifestyle choices concerning childhood obesity can be reduced through obesity-related health education and school-based standards. The healthy eating and physical activity components of a child’s lifestyle can facilitate children’s attaining and maintaining a healthy weight. They may lessen or prevent obesity-related healthcare costs.
This study incorporates obesity-related state programs with sociodemographic and economic factors, health care service accessibility, and child’s lifestyle by integrating regression statistical analysis into the concentration index approach to evaluate obesity and state program disparities. The obesity-related task force of the program option can contribute to change in a child’s lifestyle. The result of the task force variable by the concentration index shows that African American children with obesity enjoy a more advantaged position on the task force program than Hispanic and white children. The regression results show that changes in a child’s lifestyle (sports activities, daily exercise, T.V. watching, and video game playing) are key contributions to the epidemic of obesity. The C.D.C. reported that sixty-five percent of children in grades 9-12 did not get the recommended amount of physical activity, and thirtyfive percent watched T.V. for three or more hours on the average school day [28].
The Federal STEPS program is better targeted towards Hispanic and African American children than white children. The Federal STEPS program emphasizes community-based health pro-grams. It exerts efforts to reduce obesity, diabetes, asthma, and their related factors. The study pro-vides evidence that obesity does not fall evenly across the U.S. because living in low-income households, having less-educated parents, and being African American or Hispanic are characteristic factors of obesity. The actions of school, family, and healthcare providers need to be designed to provide coordination and continuity as children move from school-based activities to community settings where children live. The program of limitation of competitive food products is more unequally distributed to white and Hispanic children than to African American children. The availability of snacks and drinks sold in schools is associated with higher intakes of total energy and lower intakes of key nutrients [7]. Availability is greatest in high and middle schools. However, general accessibility to competitive foods is similar at all school levels through vending machines, snack bars, cafeterias, and student stores [35]. Competitive foods are widely available and generate substantial revenues for schools. The C.D.C. states that over one-third of children (grades 9-12) had a soft drink (not diet) during a week [28]. The effectiveness of state-level obesity-related programs is still in question. As a state-level program, creating a soft drink tax is a viable and possible program to reduce the risk of obesity [35].
A vital contribution to the literature is the finding that state health education enforcement are prime, effective program tools and will provide guidance on the scale and scope of the local obesity epidemic of school children for obesity prevention. The implemented programs will track the health behavioral characteristics of obese children in their respective states. Various innovative obesity-related programs will likely contribute to change in individual, school, and community levels concerning the obesity epidemic. The obesity-related school standards, obesity-related program options, and obesity-related state initiatives are effective and strongly associated with childhood obesity. Obesity-related state programs favor African American and Hispanic children. They are more effective toward African American and Hispanic children than white children. Low-income white children are associated with inequality in obesity-related state programs and portray a rise in obese children. White children of low socioeconomic backgrounds in the SCHIP program illustrate the disparity of obesity outcomes (i.e., health) and program disparity.
Health education and knowledge of obesity are an apparent influence on childhood obesity. The goal of the obesity program is to reduce the childhood obesity epidemic. By evaluating the efficacy of state programs, we link their effects on childhood obesity and make recommendations on the most effective state programs. State child health program implementation effectiveness is paramount to dealing with the childhood obesity epidemic. In turn, preventive health education programs for school children through obesityrelated health education classes benefit children’s health in the long run. This, in turn, impacts the state legislative environment, where a lack of public focus trumps childhood obesity. However, that is not to say that the epidemic is not being addressed; instead, it is not deemed a mission-critical aspect of state-level governments. When state governments address the issue of childhood obesity, they focus on one area in combating the epidemic: the public school system. This is the path of least resistance for most states, as school systems are locally controlled and typically supervised by the state. However, this is also a cost-effective method of reducing obesity, as children spend half their waking hours in school. Managing the school environment to minimize the spread of childhood obesity is a viable choice for controlling childhood obesity. Pro-grams can be tailored to meet the needs of children in the school system, with legislation mandating permissible obesity-related health education in the school setting and the level of physical and healthy diet education required.
The obesity-related state programs are better targeted towards obese Hispanic and African American children than obese white children. In addition, obese children are more unequally distributed to the Hispanic and African American sub-populations than the white population of similar socioeconomic circumstances. Furthermore, obesity disparities among children enrolled in the SCHIP program are more likely to be lower-income whites rather than Hispanic or African Ameri-can children. Children face the greatest long-term risk to overall health earlier in life, as childhood obesity and their associated health risks are likely to persist into adulthood. This study provides evidence to reduce childhood obesity, which is more burdensome on the healthcare system than other patients due to the increased costs of disease management and increased rates of complications due to morbidity in the long run.
Conclusions and Policy Implications
The findings of this study are related to the theory of health behaviors using an extended PRECEDE-PROCEED model. They are consistent with an important contribution to understanding better insight into highly prevalent obesity among children and the youth. This study had three important limitations. The first is the effectiveness of obesity-related state programs on overlapping programs. The interpretation of program assessment requires care in terms of validity. Second, our study used cross-sectional, microlevel data. The program effect is a long-run effect. The effectiveness related to the social benefits of government programs needs to be evaluated by a longitudinal study. Third, limits in this study prevent us from determining whether and to what extent healthcare service providers are decisive determinants of childhood obesity in omitted state-specific factors because it is cross-sectional. Despite these significant limitations, this study confirms the sociodemographic effects on childhood obesity. Furthermore, this study not only contributes to the literature about health outcome disparity concerning different race/ethnic obesity disparities but also provides new evidence of obesity-related program disparity of program effectiveness on race/ethnic differences.
Acknowledgment
We are grateful to Michael Grossman and would like to thank Pooja Patel and Marren Magee for their research assistance at Rutgers University, the State University of New Jersey, U.S.A. Any credits, analyses, interpretations, and views expressed in this paper are those of the authors and do not necessarily reflect those of the institutions. We acknowledge the research support provided by the Research Council of Rutgers University, the State University of New Jersey, U.S.A. (#2-02089 and #2-02243).
References
- Purnell JQ. Definitions, classification, and epidemiology of obesity. In: Feingold KR, Anawalt B, Blackman MR, (Eds.), (2000) Endotext [Internet]. South Dartmouth (M.A.): MDText.com, Inc.
- (2023) Mayo Clinic, Obesity, 1998-2023 Mayo Foundation for Medical Education and Research.
- Yanovski Jack A (2015) Pediatric obesity. An introduction. Appetite 93: 3-12.
- U S Preventive Services Task Force, Grossman DC, Domingo KB, Curry SJ, Barry MJ, Davidson KW, et al. (2017) Screening for obesity in children and adolescents: U.S. preventive services task force recommendation statement. JAMA 317(23): 2417-2426.
- Robinson JC, Lim CS, Hinton E, Pintado I, Gamble A, et al. (2019) School-based obesity prevention programs in rural communities: a scoping review protocol. J B I Database of Systematic Reviews and Implementation Reports 17(7): 1326-1333.
- Cunningham SA, Hardy ST, Jones R, Ng C, Kramer MR, et al. (2022) Changes in the incidence of childhood obesity. Pediatrics (Evanston) 150(2): e2021053708.
- Stierman B, Afful J, Carroll M, Chen TC, Davy O, et al. (2021) National health and nutrition examination survey 2017-March 2020 Pre-pandemic data files – Development of files and prevalence estimates for selected health outcomes. Centers for Disease Control and Prevention 158: 1-20.
- Ling J, Chen S, Zahry NR, Annie Kao TS (2022) Economic burden of childhood overweight and obesity: A systematic review and meta-analysis. Obesity Reviews 24(2): e13535.
- Curry SJ, Grossman DC, Whitlock EP, Cant A (2014) Behavioral counseling interventions: An evidence-based approach. U.S. Preventive Services Task Force. Annals of Internal Medicine, Research and Reporting Methods.
- Whitlock EP, Orleans T, Pender N, Allan J (2019) Behavioral counseling interventions: An evidence-based approach, Methods, and Processes. U.S. Preventive Services Task Force.
- Silverstein M, Kemper AR, Henderson JT, Mabry-Hernandez I (2021) Importance of assessing wellbeing for United States preventive services task force recommendations. Pediatrics 148 (Supplement 1): s37-s39.
- Carlson JA, Shook RP, Davis AM, Papa A, Steel C, et al. (2021) Investigating associations between physical activity-related neighbourhood-built environment features and child weight status to inform local practice. Social Science & Medicine 270: 113694.
- Fertig AR, de Brito JN, Trofholz AC, Berge JM (2022) Maternal employment and child weight-related health. Social Science & Medicine 310: 115303.
- Gago CM, Jurkowski J, Beckerman-Hsu JP, Aftosmes-Tobio A, Figueroa R, et al. (2022) Exploring a theory of change: Are increases in parental empowerment associated with healthier weight-related parenting practices? Social Science & Medicine 296: 114761.
- Iguacel I, Gasch-Gallén Á, Ayala-Marín AM, De Miguel-Etayo P, Moreno LA (2021) Social vulnerabilities as risk factors of childhood obesity development and their role in prevention programs. International Journal of Obesity 45(1): 1-11.
- Krist AH, Davidson KW, Ngo-Metzger Q, Mills J (2019) Social determinants as a preventive service: U.S. Preventive Services Task Force, Methods considerations for research. Research Methods 57(6): S6-S12.
- Brennan LK, Brownson RC, Orleans TC (2014) Childhood obesity policy research and practice evidence for policy and environmental strategies. Am J Prev Med 46(1): e1-e16.
- Healthy People 2020 Midcourse Review, Ch.29, Nutrition and Weight Status Centers for Disease Control and Prevention Food and Drug Administration, National Institutes of Health, Washington, D.C. U.S.A.
- Sanders LM, Perrin EM, Yin HS, Delamater AM, Flower KB, et al. (2021) A health-literacy intervention for early childhood obesity prevention: A cluster-randomized controlled trial. Pediatrics (Evanston) 147(5): e2020049866.
- Boyle MH, Olsho LEW, Mendelson MR, Stidsen CM, Logan CW, et al. (2022) Physical activity opportunities in U S early childcare programs. Pediatrics 149(6): e2020048850.
- Pitsirilos-Boquin S, Medina KM, Squillaro A, Gonzalez JC, Meyer DD, et al. (2017) A community-driven social marketing campaign to reduce childhood obesity. Journal of Community Medicine and Public Health Care 4(033).
- Subica AM (2018) Public health interventions in the era of childhood obesity and other racial health disparities. Am J Public Health 108(9): 1125-1127.
- Webb EJD, Stamp E, Collinson M, Farrin AJ, Stevens J, et al. (2020) Measuring commissioners' willingness-to-pay for community-based childhood obesity prevention programs using a discrete choice experiment. B M C Public Health 20(1): 1535-1535.
- Golden CA, Heelan KA, Hill JL, Bartee RT, Abbey BM, et al. (2022) Qualitative comparative analysis of program and participant factors that explain success in a micropolitan pediatric weight management intervention. Childhood Obesity 18(5): 324-332.
- Martins IJ (2017) Single gene inactivation with implications to diabetes and multiple organ dysfunction syndrome. Journal of Clinical Epigenetics 3(3).
- Martins IJ (2016) Anti-aging genes improve appetite regulation and reverse cell senescence and apoptosis in global populations. Advances in Aging Research 5(1).
- Martins IJ (2015) Unhealthy nutrigenomic diets accelerate NAFLD and adiposity in glob-al communities. J Mol Genet Med 9: 162.
- Division of Nutrition, Physical Activity, and Obesity (DNPAO), State and Local Programs, (2023), Atlanta, GA, U.S.A.: Center for Disease Control and Prevention, Division of Nutrition, Physical Activity and Obesity.
- S. Preventive Services Task Force (U.S. PSTF) (2017) Obesity in children and adolescents: Screening: Recommendation Statement.
- Green LW, Kreuter MW (2005) Health program planning: An educational and ecological approach. (4th edn), New York: McGraw-Hill, USA.
- Yamada T, Chen CC, Murata C, Hirai H, Ojima T, et al. (2015) Access disparity and health inequality of the elderly: unmet needs and delayed healthcare. Int J Environ Res Public Health 12(2): 1745-1772.
- Zhang Q, Wang Y (2007) Using concentration index to study changes in socio-economic inequality of overweight among U.S. adolescents between 1971 and 2002. Int J Epidemiol 36(4): 916-925.
- Lasser KE, Himmelstein DU, Woolhandler S (2006) Access to care, health status, and health disparities in the United States and Canada: Results of a cross-national population-based survey. American Journal of Public Health 96(7): 1300-1307.
- Kennedy P (2013) A Guide to Econometrics. Malden, Massachusetts: Wiley-Blackwell, USA.
- John D (2019) United States Government Accountability Office, Report to Congressional Requesters, childhood obesity research demonstration, Efforts to identify effective strategies for low-income Children, GAO-20-30.
© 2024 Tetsuji Yamada. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






