- Submissions

Full Text
Gerontology & Geriatrics Studies
Evaluation of Dementia Day Care Programmes by Caregivers: A New Zealand Case Study
Annie Weir*
University of Auckland, New Zealand
*Corresponding author: Annie Weir, Director, Impact Research NZ and Honorary Academic, School of Critical Studies, Faculty of Education, University of Auckland to Impact Research New Zealand, New Zealand
Submission: February 28, 2018; Published: March 13, 2018

ISSN : 2578-0093Volume2 Issue3
Abstract
This article reports on the benefits to caregivers of having their family member living with dementia attend a day programme. This study was part of a larger investigation undertaken in New Zealand that identified the elements that make up an effective community-based day programmes. One of the key elements identified was benefits of day programmes to caregivers. Telephone interviews and a questionnaire elicited the views of caregivers on the benefits to them of day programmes. The research revealed that caregivers appreciated respite from having to provide 24/7 care and identified three main benefits:
A. Reduction in stress;
B. Freedom to do activities alone and with others; and
C. Ability to keep working.
Having routine personal time when their family member was attending a day programme was particularly important for catching up on household chores, maintaining relationships with family and friends and keeping up with hobbies, clubs and sport. Other benefits included peace of mind that their loved one was safe, cared for and that they participated in a wide range of activities based on cognitive stimulation and social interaction. Although these findings are from a specific context, it raises the importance of not only research into the perceived benefits of day programmes for caregivers but also wider implications of impacts on their health and well-being.
Keywords: Dementia; Caregiver; Respite; Day programmes
Introduction
Dementia is a worldwide health issue. Improved health care and living standards has resulted in people living longer and significantly increasing numbers of older people being diagnosed with dementia that need to access a range of dementia-related services [1,2]. Dementia describes a collection of progressive and incurable symptoms experienced by an individual. These include memory loss, disorientation, wandering, problems with reasoning and communication skills, a reduced ability to carry out daily activities, and also depression, anxiety or loss of personhood [1,2].
It is estimated that 46.8 million people worldwide are living with dementia and that this number is likely to increase to 131.5 million in 2050 [3]. Internationally it is recognised that dementia is a costly condition from its social, economic and health dimension [4]. Consequently, an increasing number of governments around the world including New Zealand have developed policies designed to support people living with dementia to remain longer at home in their communities [2].
Day programmes appear to provide an important service as part of the care continuum for both people living with dementia at home and their caregivers [5]. These day programmes typically offer a range of therapeutic activities designed to improve cognitive functioning. Additionally, social services are provided including for example, transport to and from the day programme, activities, events, outings, meals and refreshments [6,7].
Research undertaken in New Zealand [8] noted that through specifically recognising that every client has different interests and needs, the day programme staff were able to support attendees to strive to achieve their individual goals related to maximising their cognitive and physical functioning and socialising. This was done through having individualised support plans which built on the original District Health Board (DHB) government funded Needs Assessment and Service Coordination Service (NASC) assessments and subsequently offering a variety of activities that were based on the client's interests and hobbies on a day-to-day or weekly basis. While some activities are carried out with support workers on a one-to-one basis, other activities are provided to clients as a group. The day programmes offer a wide range of activities across each week, depending on client interests and their individualised support plans.
A range of psychosocial benefits through client participation in the programme were identified by caregivers and day programme staff for example: making friends, helping others, doing exercise, enjoying music and art, utilizing cooking and gardening skills, as well as positive interactions with children and animals. All clients participated in daily routines and these activities appeared to provide a sense of security. In addition to client benefits, caregiver benefits were also identified [8].
Caregiver Benefits of Day Programmes
This article focuses on the benefits of day programmes to caregivers. While the term 'caregiver' has multiple meanings and uses in the social services sector (including as paid employees in a caregiving role), for the purposes of this study, the term 'caregiver' refers to spouses or family members of people living with dementia who attend a day programme.
Caregiver respite for spouses or family members seems to be an important feature associated with community-based day programmes for people living with dementia. Caregivers are given an opportunity to have a break from the challenges that come with looking after a family member who has been diagnosed with dementia 24/7. Caregivers are also provided with peace of mind knowing their family member is safe and looked after.
While families continue to be the greatest resource in helping frail older adults to live longer at home, providing care to frail older adults can be stressful and result in a range of well-documented negative consequences, including clinical depression, health problems, social isolation, financial difficulties, and mortality [5,6]. This is particularly the case for family caregivers of individuals with dementia, who experience greater distress in comparison to individuals caring for non-demented older adults, and who tend to be the most frequent users of adult day services [7]. In a study of 173 family caregivers that explored the effects of the use of adult day services, results indicated that those who availed themselves of the service had lower exposure to care-related stressors on those days, had more positive experiences, lower anger and reduced impact of noncore stressors [8].
A systematic review was undertaken in 2008 of studies addressing the effectiveness of interventions that assist caregivers to provide support for people living with dementia in the community [9]. From this review there is evidence to support the use of well-designed psycho-educational or multi-component interventions for caregivers of people with dementia who live in the community. Factors that appear to positively contribute to effective interventions are those which:
A. Provide opportunities within the intervention for the person with dementia as well as the caregiver to be involved
B. Encourage active participation in educational interventions for caregivers
C. Offer individualised programmes rather than group sessions
D. Provide information on an on-going basis, with specific information about services and coaching regarding their new role
E. Target the care recipient particularly by reduction in behaviours
Factors which do not appear to have benefit in interventions are those which:
1. Simply refer caregivers to support groups
2. Only provide self-help materials
3. Only offer peer support [9].
A systematic review of the benefits of day services for people living with dementia published in 2017 identified seven themes that emerged from the review:
A. Reduction of role overload
B. Lower care related stressors
C. Mood - minor decreased depressive symptoms
D. Importance to caregiver's mental and physical health
E. Relationships of the caregiver with others in their lives
F. Cost - able to work and
G. Symptoms management - the amount of time caregivers spent on managing the person with dementia was reduced [10].
With acknowledgement of mixed results in terms of the type of intervention, number of sessions, the setting, care receiver age, caregiver age, gender, type of caregiver-care receiver relationship (spouse vs adult child), initial burden, and study characteristics etc., it can on the whole be accepted that one of the core elements of day programmes is the benefit to caregivers.
Caregiver Benefits of Dementia Day Programmes: A New Zealand Case Study
Context
In recognition of burgeoning numbers of older people diagnosed with dementia, the New Zealand Ministry of Health (MOH) released in 2013 the 'New Zealand Dementia Care Framework’ [11]. District Health Boards (DHB's) funded by the MOH were required to develop dementia care pathways for those people with the diagnoses and purchase services in the community from providers along the care continuum. The Framework actively promotes community-based services that support those individuals living with dementia to remain living at home and day programmes are a key component of this approach [11].
This article reports on the perceived benefits for caregivers whose family member attends a day programme for people living with dementia. The data and findings reported on caregiver benefits are part of a larger research project that aimed to explore:
1. What are the elements that make up an effective client-focused day programme for people living with dementia?
2. What are the methods employed by organisations to measure the quality of outcomes of their day programmes?
The original research was commissioned by Presbyterian Support Northern and undertaken by Impact Research New Zealand was reported in Dementia in 2015 [12]. The research revealed that effective day programmes comprised five core elements including: activities aimed at improving client functioning; caregiver benefits; workforce capability; cultural responsiveness; and service processes [12]. This article focuses on the core element of caregiver benefits.
Methodology
In order to explore the benefits to caregivers of day programmes for people living with dementia, two methods were selected:
1) Semi-structured telephone interviews and
2) A paper-based questionnaire.
Study setting
Through its Enliven services, Presbyterian Support Northern (PSN) has been providing community-based support and care for older New Zealanders since 2002. As part of their service offering, PSN Enliven has been contracted by various DHBs to run day programmes in five upper North Island locations. The research sites selected were one in Hamilton with mainly European and Maori populations and one in South Auckland with mainly Pasifika, Maori and European populations. Only clients with dementia and their caregivers were included in the study. The original research focused on day programmes regarded as a non-residential day service utilising a social care model and although based in the community, excluded home-based services.
Sampling and recruitment of participants
Participant selection: Area managers and team leaders in the respective day programmes identified and contacted caregivers to obtain permission to forward their names and contact details to the research team and to inform them that a researcher from Impact Research NZ might be in contact with them about the research, if they consented. A list of potential participants was forwarded to the research team who identified two categories of caregiver participants: 'Group A' who were invited to participate in a telephone interview and complete a questionnaire, and 'Group B' were only invited to complete a questionnaire.
Group A: Telephone interview and questionnaire: Group A consisted of four caregivers from each of the two sites (eight in total) who were invited to participate in a semi-structured telephone interview and also invited to complete the questionnaire. Caregivers received an information sheet outlining the purpose of the evaluation, right to withdraw up to the time of data analysis, also an outline on data security and how the information would be used. These semi-structured interviews were approximately 30 minutes in length, and with the verbal and written consent of participants obtained, audio recorded and later transcribed. A list of questions was emailed at least a day prior to their interviews to help them with their interview preparation. The consent form and participant information sheet were also sent electronically
Group B: Questionnaire only: Group B consisted of a total of 29 caregivers were sent a paper copy of the questionnaire in the post, an invitation letter and instructions on how to participate, a participant information sheet, a consent form, and a postage-paid envelope to return the completed questionnaire to the Impact Research NZ.
Telephone interviews: Telephones interviews provide anonymity for participants who do not meet directly with the researcher. A service provider can identify participants who agree to a telephone interview and then pass contact details onto the researcher providing they agree. Participants are typically provided with information on the project objectives, their rights as participants, anonymity and how data is stored and reported.
The semi-structured telephone interviews explored the following areas:
A. How well they thought the day programme was meeting the needs of their family member?
B. What were the benefits to themselves as primary caregiver other of having their loved one attend a day programme?
C. What aspects of the day programme worked well for them, for example not having to provide transport to and from the day programme, not having to prepare and cook meals during the day for their loved one.
D. Caregivers were asked to comment on any particular issues with the day programme that they thought had been challenging in any way
E. Caregivers were also asked to comment on any ways in which Enliven could potentially improve its day programme service?
Caregiver questionnaire
Paper-based questionnaires are a cost effective method of eliciting data from a large geographic area and provide for efficient data analysis. Paper-based questionnaires are familiar to most older people. Nearly everyone has had some experience completing questionnaires and they generally do not make older people apprehensive. When a respondent receives a questionnaire in the mail, he or she is free to complete the questionnaire on their own time. Questionnaires reduce bias as there is no direct contact with the researcher.
Key questionnaire areas for investigation included demographics such as age, gender, ethnicity, geographic location and how many days per week a family member attended the day programme. A five point likert scale from strongly agree to disagree and additionally not applicable was used, as well as areas for comment under statements and open ended questions to gain caregiver's views on the following areas:
A. What were the benefits of the day programme to them?
B. Whether they thought day programme staff communicated effectively with them.
C. Caregivers were asked to rank a series of 15 day programme activities such as physical activities, events. Outings to using a computer, from the most effective to the least effective for their family member.
D. Caregivers were asked about what they thought of the overall quality of the day programme.
E. Caregivers were asked about what they thought were the best parts of the day programme for their family member.
F. Caregivers were asked to suggest areas for improvement for the day programme.
Analysis
The data from the recorded telephone interviews and qualitative comments from the caregiver survey were analysed using inductive thematic analysis. This involved reading the transcripts and comments to establish keywords and emerging themes, and repeat readings to check and refine established themes. Themes were organised into broad categories and selected quotes from respondents' accounts were used to illustrate the themes. Analysis of this data using constant comparison between cases provided a distillation of participants' experiential knowledge. Quantitative data from the surveys were entered into Excel and used to generate descriptive statistics.
Result
This section presents quantitative data gathered from 23 questionnaires completed by caregivers, followed by qualitative data from eight semi-structured interviews with caregivers. A total of 31 caregivers participated in the research.
A. Questionnaire result
Unsurprisingly the majority of the caregivers were female (87%), in keeping with national trends, with the remainder being male (13%). Ten of the 23 caregivers lived in Auckland while the other 13 resided in Hamilton. The majority of caregivers were European, with a few being Maori and Pasifika.
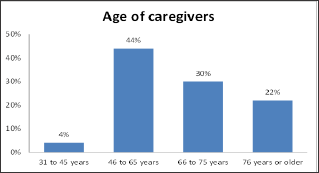
B. Age of caregivers
The age distribution of the 23 caregivers (see Figure 1 below) highlighted that slightly more than 50% of the caregivers were older than 65 years of age themselves (retirement age in New Zealand). 22% of the caregivers were older than 76 years of age, and potentially having health issues of their own. Almost half the caregivers were of working age with 44% aged between 46 to 65 years and a small percentage (4%) of the caregivers were between 31 to 45 years of age.
Figure 1: Age distribution of caregivers.
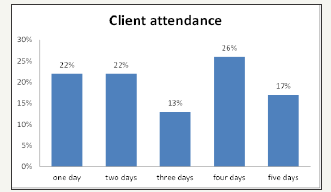
C. Client Attendance
Clients' attendance at the day programme ranged for a few months to five years. Weekly attendance at the day programme (see Figure 2 below) varied according to the needs of the clients as well as their caregivers. Over half of the attendees participated in the day programme three days or more a week (54%) and just under half attended one or two days
Figure 2: Programme attendance distribution of clients.
D. Positive difference for clients
The majority of the caregivers (74%) agreed that the day programme made a positive difference to their family member with the remainder either having a neutral response or disagreed (see Figure 3 below). Positive differences included loved ones looking forward to going to the day programme, making friends, taking part in a wide range of activities tailored to maximising functioning. Caregivers were asked to rank a series of 15 day programme activities such as physical activities, events, outings, to using a computer, from the most effective to the least effective for their family member. The most effective activities enjoyed by clients were group events and outings, activities involving music and art, cooking and gardening. Caregivers were asked about what they thought were the best parts of the day programme for their family member. While responses varied the the majority agreed that having the routine of going to the day programme and being with other people was the best part and that transport is provided, the meals and refreshments are provided and the activities were varied.
Figure 3: Caregivers' perception on the positive difference for the clients.
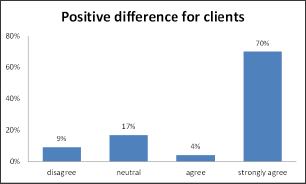
The remainder of caregivers were either neutral or disagreed stating that their family members' experiences at the day programme varied and as did the mood of their family member - good days and not so good days.
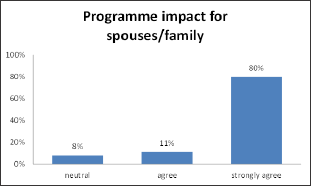
E. Positive impact on caregivers
91% of the caregivers agreed or strongly agreed that the programme had a positive impact for spouses or family members (see Figure 4 below). Positive impact included: reduction in stress, having free time to pursue daily activities (chores, shopping, catch up with friends and other family members, go to clubs, and play sport. For over half the caregivers, freedom to work knowing that their family is safe and being cared for was important to them. A few respondents noted the day programme allowed them to keep their family member at home - effectively delaying entry into a nursing home. The respondents regarded the impact as neutral was less than 10%.
Figure 4: Caregivers' perception on the impact of the programme for spouses/family members.
F. Communication with staff
The majority of caregivers agreed that they had ease of communication with day programme staff, particularly with developing the individual plan for their family member (see5 below). Additional suggestions on activities to better meet the needs of caregivers included developing a newsletter to increase caregivers' knowledge of the programme at a more general level and also possibly help them feel that they have a better idea of how the day programme changes throughout the year. Some of the caregivers also expressed an interest in having an opportunity to spend a bit more time at the day programme itself. Special 'family days' that may involve family members other than the primary caregiver were offered as a suggestion.
Figure 5: Caregivers' perception on ease of communication with programme staff.

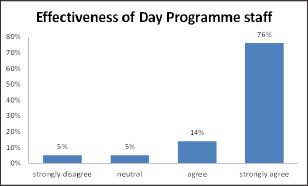
G. Effectiveness of day programme staff
The majority of caregivers (90%) either agreed or strongly agreed that the programme staff were effective in meeting the needs of their family member attending the programme (see Figure 6 below). They commented that the staff were friendly, welcoming, related well to their family member and got them involved in a wide range of activities.
Figure 6: Caregivers' perception on effectiveness of Day Programme staff.
In summary the caregivers who took part in the questionnaire explicitly acknowledged how they enjoyed a variety of benefits as a result of their family member attending the Enliven day programmes. This is of particular significance given that these individuals are the designated primary caregiver of a person living with dementia and in most cases, live with and are responsible for their spouse or family member for 24 hours of every day. The majority of caregivers agreed that from their perspective the overall quality of the programme was very good - it provided a safe environment for their family member and offered individualised programmes designed to meet their needs while providing a much needed break for them as caregivers to pursue their work and activities.
H. Results from the telephone interviews
The telephone interviewees were grateful for the day programme service and felt that staff treated their family member with respect and tailored their activities to meet their needs as identified in their plan. Interviewees commented that the day programme provided a range of interesting activities with music, art, outings and events being popular. The interviewees noted how important it was for their family member to socialise and get involved in doing activities outside their home. Interviewees commented that their family member liked the routine of going to the day programme and some would get ready very early and eagerly await for the van to pick them up. Having meals and refreshments provided during the day was identified as a helpful part of the day programme.
Interviewees highlighted that it would be helpful to be told in advance on the daily activities so when their family member came home they could remind them what they had done and talk more about their day.
I. Key benefits for caregivers
All of the interviewees identified not having to provide transport to and from the day programme was a great help to them. They liked that once the family member had left the house they were free to go to work and get on with their own activities. Interviewees liked the fact they did not have to provide packed lunches, snacks and drinks for their family member as this was catered for at the day programme.
Three main themes that emerged from the interview data on perceived benefits to the caregivers themselves by having their spouse or family member attend a day programme. These are:
1) Reduction in stress,
2) Freedom to do activities alone and with others.
3) Ability to keep working. These findings are similar to the main benefits identified in the questionnaire findings.
J. Reduction in stress
The day programmes alleviate caregiver stress and helps them to stop worrying about their spouse or family member when they are not with them. On the days they attend the programme, the caregivers know precisely where they are and that they are also in a safe space where they are being looked after as the following quotations demonstrate:
"I know my nana feels a sense of belonging and that s important to me that she has that. That's a benefit for me as well because I can go away and know she’s safe and looked after. She's cared for emotionally and mentally and that helps me emotionally and mentally as well." "In terms of benefit to me personally, one thing that comes to mind is instead of sitting at work wondering what mum's doing at home, is she trying to cook or is she sitting at home vegetating wondering what to do or has she gone for a walk and will she be able to find her way back, I know that she is in the day programme four days a week and there is peace of mind." "Knowing the ladies that are there [at the day programme]. I know that she is in safe hands. I know that I don't have to worry, if I call in during the day, whether she's going to be off somewhere and losing her way, not being able to find her way back."
K. Freedom to do activities alone and with others
The caregivers also benefit from the opportunity to be able to do leisure activities with their friends like meeting for lunch or practical tasks that might be too difficult to do when their spouse or family member is at home with them.
The quotations below shed more light on this third important benefit to caregivers:
"For us, when she's gone, we get to clean up the house, move some things around, which she finds distracts her from her TV.... We do gardening, we go to the gym, we do walking. We do shopping." "It’s the freedom to just do what you want to do. Sometimes on a Thursday after I've dropped him at the blokes club, I might come home and just sit down on my own. And just enjoy being on my own without having to repeat myself all the time, telling him the same thing over and over that he thinks I haven't told him. I suppose I just relax a bit." The main benefit for me is that I have some times during the day to do a few jobs that need to be done. Like my computer crashed and it's taken me most of yesterday and today to get it sorted. It would have been very difficult if he was here.. For me it's good. I can do the supermarket shopping or things like that without having to take him with me."
L. Ability to keep working
Almost half the caregivers were of working age (31 to 65 years old). The day programmes allow caregivers to be able to continue working full-time or on a part-time basis, while looking after their family member at home or supporting them to live on their own instead of being in residential care. Comments about this benefit included the following statements:
"It allows me to work, to still have an income. I can meet all my family's needs." "It works for me in terms of being able to go to work and still have her." "It means that I can work, because I don't think that, if she was at home all day every day that I would have to be close by all day. She doesn't actually live with us, she lives on her own, so it would just mean that I would have to be there most of the day." "It allows me to work full time. I live on the road with my work. I'm quite a busy person in my work."
The caregivers unequivocally agreed it was vital that they were able to have a regular break from their caregiving role in the home environment. In addition to the three main benefits identified by caregivers:
1. Reduction in stress;
2. Freedom to do activities alone
3. Ability to keep working and with others, several participants also identified the following benefits:
A. They felt supported by the day programme staff as they shared the burden of care, and it helped them to go on longer caring for their loved one at home, effectively delaying entry into a nursing home.
B. Being able to talk to day programme staff about the best kind of support for their loved one as their condition worsened.
Discussion
In greater numbers than ever before, caregiver family members face a dilemma between creating and maintaining a healthy life balance of work, family and recreational activities for themselves and care for their elderly family member living with dementia. For many caregivers, finding the balance between competing needs is extremely challenging. Caregivers can become overwhelmed by the sheer burden of work they face when caring 24/7 for their family member living with dementia and this in turn can affect their own health and well-being. Between specialist visits, medicine routines and sometimes the lack of proper care knowledge to meet their loved one's needs, caregivers look for respite beyond that offered by family and friends. Day programmes for people living with dementia provide professional respite that caregivers trust. Caregivers also value routine of knowing when their family member will be cared for at the day programme, and also that they are safe, which provides them with peace of mind. In addition to knowing their family member is involved a wide range of activities in a day programme, it helps them to feel they are doing their best to care for their loved one while not having to be there with them.
This caregiver study did not directly address the issue of whether or not day programmes do allow their family member to remain longer at home, however, several participants did note that as a benefit to them. It is interesting to note that past evaluation studies have not been able to consistently document the effect of day programmes on the ability of the programme to delay nursing home placement [13,14]. However, a meta-analytical review conducted in 2003 indicated that some caregiver interventions can reduce caregiver psychological morbidity and help people with dementia stay at home longer. Programmes that involve the patients and their families and are more intensive and modified to caregivers' needs seem to be more successful [15].
The age distribution of the caregivers is noteworthy with just under half of working age and approximately half the caregivers were over 66 years old and of that group almost half of them were 76 years or older. Potentially this raises questions not covered in this study for example around what are the similarities and differences in the different age groups needs and abilities to sustain having their family member with dementia remain at home. Does the working age cohort access day programme support at a similar or different level to the 66 year and older cohort? For the oldest cohort of caregivers 76 years and older how does the day programme meet their needs? This may have implications for the design of future day programmes as more cognisance is taken of the differing needs of the caregivers at different stages of their lives.
Conclusion
In conclusion, the day programmes under study demonstrated that they are an important part of the care continuum for people living with dementia and their caregivers. For those individuals who bear the burden of being the primary caregiver for their family member, having them attend a day programme brought welcome respite and a sense of shared burden. In order to support their family member to remain at home longer and delay entry into a nursing home, a caregiver needs help to maintain their own health and wellbeing, participate in social activities that keep themselves engaged with other family, friends and the community. The relationship and communication between the caregiver and day programme staff is important in supporting the care and functioning of the loved one.
Government policy and funding supports people living with dementia to remain at home in the community for as long as possible, citing a number of social and health benefits to the person living with dementia and their families. Fiscally it is seen as the best option to delay entry to more costly residential facilities. There is appears to be some tension between competing needs of the person with a dementia diagnosis, the needs of the primary caregiver and how able and willing they are to have their loved remain at home for as long as possible, and with the government policy aimed at delaying entry into a nursing home.
References
- Kirkman A (2011) Caring from duty and the heart: Gendered work and Alzheimer's disease. Women's Studies Journal 25(1): 2-16.
- Fitzgerald and Associates (2007) WDHB Dementia and Delirium Service Provision. An Issues Paper. Waitemata District Health Board, Auckland, New Zealand.
- (2017) World Health Organization.
- (2016) Alzheimers Disease International. World Alzheimer.
- Schulz R, Beach S (1999) Caregiving as a risk factor for mortality: The Caregiver Health Effects study. JAMA 282(23): 2215-2219.
- Schulz R, O Brien A, Czaja S, Ory M, Norris R, et al. (2002) Dementia caregiver intervention research: In search of clinical significance. Gerontologist 42(5): 589-602.
- Ory MG, Hoffman RR, Yee JL, Tennstedt S, Schulz R (1999) Prevalence and impact of caregiving: A detailed comparison between dementia and non-dementia caregivers. The Gerontologist 39(2): 177-186.
- Zarit SH, Kim K, Femia EE, Almeida DM, Klein LC (2013) The Effects of Adult Day Services on Family Caregivers' Daily Stress, Affect, and Health: Outcomes From the Daily Stress and Health' (DaSH) Study. Gerontologist 54(4): 570-579.
- Parker D, Mills S, Abbey J (2008) Effectiveness of interventions that assist caregivers to support people with dementia living in the community: a systematic review. Int J Evid Based Healthc 6(2): 137-172.
- Sorvaag MJ (2017) Benefits of Adult Day Services for Dementia Caregivers: A Systematic Review. Master of Social Work Clinical Research Papers. 799.
- Ministry of Health (2013) New Zealand Framework for Dementia Care. Ministry of Health, Wellington, New Zealand.
- Weir A, Fouche C (2015) Community-based dementia day programmes: Common elements and outcomes measures. Dementia (London) 16(3):
- Gaugler JE, Zarit SH (2001) The effectiveness of adult day services for disabled older people. J Aging Soc Policy 12(2): 23-47.
- Weissert WG, Hedrick SC (1994) Lessons learned from research on effects of community-based long-term care. J Am Geriatr Soc 42(3): 348- 353.
- Brodaty H, Green A, Koschera A (2003) Meta-Analysis of Psychosocial Interventions for Caregivers of People with Dementia. J Am Geriatr Soc 51(5): 657-664.
© 2018 Annie Weir. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






