- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Pott’s Puffy Tumor- A Case Report and Brief Review of Literature
Darwin Kaushal*, Nikhil Rajan, Bikram Choudhury and Kapil Soni
Department of Otorhinolaryngology, AIIMS Jodhpur, India
*Corresponding author: Darwin Kaushal, Department of Otorhinolaryngology, AIIMS Jodhpur, India
Submission: June 06, 2018;Published: September 20, 2018

ISSN 2637-7780 Volume2 Issue3
Abstract
Pott’s puffy tumour is a very rare clinical entity in current rhinology practice. However, the condition is known to have significant rates of complication if not recognised early and treated adequately. We report a rare case of Pott’s puffy tumour in an adult patient and review the relevant medical and surgical management principles.
Keywords: Pott’s puffy tumour; Frontal osteomyelitis; Complication of sinusitis
Introduction
Pott’s puffy tumour is a subperiosteal abscess with associated osteomyelitis arising from the frontal sinus. Aetiology for the same has been reported as post traumatic, sequelae to acute and chronic frontal sinusitis and even insect bites. However, in the post antibiotic era, the incidence of this condition has declined significantly. This condition has a high risk of intracranial complications such as abscess formation and meningitis if not recognised early and appropriately treated. Even though it is more common in the paediatric age group, there are few cases reported in the adult population as well [1]. In this article we report a case of Pott’s puffy tumour in a 30year old man and review the relevant literature regarding the best management principles.
Case Report
A 30-year-old man presented to the outpatient department with complaints of a swelling over the medial canthus and forehead region for 10 days. It was insidious in onset and gradually progressive in nature. There was history of fever for 10 days. However, there was no history suggestive of sinusitis. On examination the patient was found to have a 3x 3cm fluctuant, tender, warm swelling over the nasion and forehead. Nasal endoscopy revealed congested turbinates with mucoid discharge. There was periorbital oedema with mechanical ptosis of the left upper eyelid as well.
The patient was further evaluated with a computed tomography and was found to have a tissue enhancing lesion in the left frontal sinus causing expansion, thickening and sclerosis of frontal bone with erosion of the outer table and secondary sub-galeal soft tissue component which showed a thick enhancing wall. The extra calvarial abscess measured 5x2cm.
Hemogram, viral markers, blood sugars, electrolytes and kidney function tests were normal. A fine needle aspirate was done which showed inflammatory cells, and Ziehl-Neilsen stain was negative. Aerobic culture and sensitivity showed Staphylococcus aureus which was sensitive to penicillins.
Conservative management in the form of IV antibiotics was implemented for 48 hours. However, there was no improvement. In view of the above findings, the patient was taken up for a combined approach fronto- ethmoidectomy under GA. Lynch- Howarth incision was made over the left side and soft tissues dissected and retracted. A defect was identified in the anterior table of the frontal sinus and 20 cc of thick pus was drained. Frontal sinusotomy was done endoscopically and the patency of the fronto-ethmoidal recess was established. Saline irrigation was done, and the wound was closed.
Packs were removed on postoperative day two and the patient was put on antibiotic therapy for 3 weeks. The patient improved symptomatically and is currently asymptomatic at 6 months of follow- up’s cosmetic result is excellent and there are no features suggestive of sinusitis.
Discussion
Review of management options
With the improvement of antibiotic therapy, the incidence of osteomyelitis of the frontal bone is quite rare. Even though the condition is relatively easy to suspect and diagnose, most ENT specialists would not have managed more than a few cases themselves. The diagnosis may be delayed if the patient initially presents to other specialities where this diagnosis may not be thought of [2].
Here we review the published literature regarding the management options and discuss a case managed by a combined approach- external drainage and endoscopic sinus surgery.
The aim of treatment in Pott’s puffy tumor is to remove the infective focus by debridement, antibiotic therapy to prevent intracranial or orbital complications and to maintain the patency of the sinus outflow tract. Historically (Figure1), an external approach with drainage of the pus and removal of the non-vital bone has been the standard management of this condition. Most patients are started on broad spectrum antibiotics and later given culture specific antibiotics for six to eight weeks [3]. However, there are a few concerns such as creation of a fronto-cutaneous fistula or an unsightly scar. Failure to create a patent frontal sinus drainage tract can result in recurrent sinusitis. More recently there have been reports of uncomplicated cases that were managed with a completely endoscopic procedure and long-term antibiotics, although the same author reports a 10% revision surgery rate [4]. It is also to be remembered that endoscopic frontal sinus surgery (Figure 2) in an inflamed and infected condition can be difficult in the best of hands. There are also reports of balloon sinuplasty being successfully used as a treatment modality for the management of Pott’s puffy tumor [5].
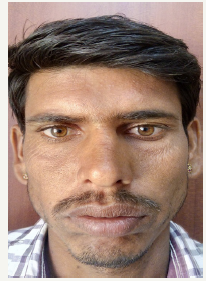
Figure 1:Pre-operative image

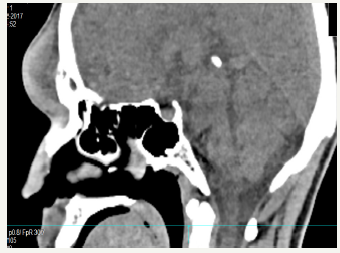
Figure 2:Pre-operative CT scan showing bone erosion and subperiosteal abscess
Another series of four patients underwent a Draf 2a procedure and pus was expressed out through the widened ostium. They also received long term antibiotic therapy. Those patients who had intracranial infection at presentation also underwent neurosurgical intervention in the form of burr holes and pus drainage. They advocate against the use of an external approach or removal of the bone sequestra claiming that infected bone can remodel completely. Even though there were no intra-operative complications reported, it is interesting to note that two of the four patients had to undergo revision surgery for persistent sinusitis [6].
In another review of 32 patients the authors reviewed data from 27 case reports and 5 cases from their own series and concluded that an initial correct clinical diagnosis followed by urgent CT or MR scanning and surgery under the cover of antibiotics is the ideal management strategy. However, they also opine that it may not be necessary to perform surgery immediately if enough initial treatment is performed. They further opine that if ESS is selected as the surgical approach (Figure3), then there may be more complications or inadequate disease removal due to the acute inflammatory state [2].
Figure 3:Post-operative appearance
Conclusion
Since there is no consensus or high-level evidence for the management of Pott’s puffy tumor, and the paucity of published literature in the form of isolated case reports and case series, it is imperative that treatment should be tailored to each case scenario (Figure4). Patients who present with no evidence of intracranial complications shall benefit from drainage of pus and sequestra through an external approach such as the Lynch-Howarth. Patency of the frontal sinus outflow tract must be established either endoscopically or through external fronto-ethmoidectomy as deemed fit in accordance with the surgical teams’ experience and preference. However, any patient with intracranial pus collection should receive neurosurgical care as well. Patients should be serially monitored and would benefit from antibiotic therapy for at least three weeks. More evidence is needed to recommend ESS as the sole surgical intervention due to the high recurrence rates in the reported series.
A combined approach fronto-ethmoidectomygives excellent exposure for thorough debridement, and simultaneously permits the patency of the sinus outflow tract to be established and hence can be considered the best approach. The aesthetic results are excellent in a well-planned incision as exemplified by our case.
References
- Shin JW, Choi IG, Jung SN, Kwon H, Shon WI, et al. (2012) Pott puffy tumor appearing with a frontocutaneous fistula: J Craniofac Surg 23(2): e158-e160.
- Akiyama K, Karaki M, Mori N (2012) Evaluation of adult pott’s puffy tumor: Our five cases and 27 literature cases. The Laryngoscope 122(11): 2382-2388.
- Parida PK, Surianarayanan G, Ganeshan S, Saxena SK (2012) Pott’s puffy tumor in pediatric age group: A retrospective study. Int J Pediatr Otorhinolaryngol 76(9): 1274-1277.
- Leong SC (2017) Minimally invasive surgery for pott’s puffy tumor: is it time for a paradigm shift in managing a 250-year-old problem? Ann Otol Rhinol Laryngol 126(6): 433-437.
- Bozdemir K (2012) Treatment of Pott’s Puffy tumor with balloon sinuplasty: report of three cases. Turk J Ear Nose Throat 22(6): 342-347.
- Van Der Poel NA, Hansen FS, Georgalas C, Fokkens WJ (2016) Minimally invasive treatment of patients with Pott’s puffy tumour with or without endocranial extension a case series of six patients: Our Experience. Clin Otolaryngol 41(5): 596-601.
© 2018 Darwin Kaushal. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






