- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
The Nonsurgical Conservative Treatment of Thrombophlebitis of the Lateral Sinus
Fatogoma Issa K*, Cissé Naouma, Soumaoro Siaka, Diarra Kassim, Konaté N’faly, Guindo Boubacary, Singaré Kadiatou, Samba Karim T and Mohamed Amadou K
Department of Otorhinolaryngology-Head and neck surgery, Teaching hospital of Gabriel Toure, Mali
*Corresponding author: Fatogoma Issa K, Department of Otorhinolaryngology-Head and neck surgery, Teaching hospital of Gabriel Toure, Faculty of Medicine, Mali
Submission: June14, 2018;Published: September 06, 2018

ISSN 2637-7780 Volume2 Issue3
Abstract
Currently mastoidectomy without thrombus evacuation is a therapeutic alternative. A new conservative medical therapeutic approach based on antibiotic therapy without mastoidectomy as a therapeutic alternative. Through a clinical case treated conservatively without mastoidectomy, we report an observation of the TPSL and review the literature. Patient 16-year-old patient admitted for otorrhea due to acute otitis media where we diagnosed lateral sinus thrombophlebitis. We opted for medical treatment without mastoidectomy. The treatment did the effect without detectable complication. Management of thrombophlebitis cases of the lateral sinus requires an evaluation of the clinical and Para clinical parameters of the patient to propose a therapeutic alternative.
Keywords: Acute otitis media; Thrombophlebitis lateral sinus; Conservative nonsurgical treatment
Introduction
Lateral sinus thrombophlebitis (TPSL) is a rare intracranial complication of otitis media [1]. It can be caused by acute otitis media as well as chronic otitis media. With the advent of antibiotics its incidence has evolved into decrescendo and has now reached a rate of 2 to 20% [2]. Despite the decline in incidence and mortality, it continues to be life-threatening [2]. The diagnosis of thrombophlebitis is a challenge for modern otolaryngologists. These diagnostic difficulties arise from the scarcity of cases of TPSL and the absence of a classic sign using antibiotics such as picketfence fever [3]. Early diagnosis requires a high index of suspicion and a good understanding of its various clinical presentations. Traditionally the treatment of TPSL includes mastoidectomy with evacuation of thrombus antibiotic therapy and with or without use of anticoagulants [3].
Currently mastoidectomy without thrombus evacuation is a therapeutic alternative reported by the literature [2-5]. This gesture allows recanalization of the lateral sinus. A new conservative medical therapeutic approach based on antibiotic therapy without mastoidectomy as a therapeutic alternative in recent series [4]. The analysis of these data does not admit any consensus regarding this medical conservative treatment without mastoidectomy of TPSL of otogenic origin. As part of bringing elements that can highlight the rationalization and indication of non-surgical conservative medical treatment of otogenic TPSL. Through a clinical case treated conservatively without mastoidectomy, we report an observation of the TPSL and review the literature.
Case Report
We received a patient 16 years old for a right otalgia developing for four days. This earache occurred in a context of notion of fever. Deafness, slight ipsilateral otorrhea and tinnitus were associated otologic signs. The headache occurred 48 hours before and was associated with rotational vertigo, vomiting, and spontaneous right lateral cervical pain. In these antecedents no notion of right otorrhea was mentioned. In these antecedents a medical treatment based on antibiotic and analgesic.
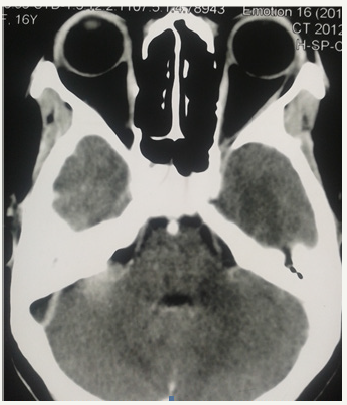
The otoscopic examination found a weak purulent otorrhea. After aspiration, it was found a perforation antero-lower right. The post auricular and right posterior cervical pain were noted. The general examination found a normal neurological state; a general state preserved; a pulse at 141beats/minute; body temperature at 39.9 °C. Chest X-ray has become normal. Computed tomography showed an empty Delta sign after the injection of the contrast medium, evoking thrombophlebitis of the lateral sinus extended to the internal jugular vein (Figure 1). Biology found normochromic normocytic anemia at 5g/dl; leukocytosis at 20500E/mm3, low serum iron and normal ferritinemia, CRP positive at 24mg/L. Blood culture exhibited Enterococcus avium sensitive to Clarythromycin. A general probabilistic antibiotic therapy was initiated based on amoxicillin 1gram+clavulanic acid 125 direct intravenous association every eight hours for ten days, then readapted to the antibiogram: Clarythromycin 500mg every twelve hours by oral route for four weeks. Paracetamol infusion 1 gram every 6 hours. An ear drop based on ciprofloxacin in both ears. Normalization of the blood count was observed after three weeks. Complete remission of clinical and paraclinical signs was obtained after four weeks of treatment. Computed tomography did not detect any defect.
figure 1:CT Scan brain bone window axial cut showing the classic empty delta sign on the right side.
Discussion
The clinical spectrum of thrombophlebitis of the lateral sinus is variable [3]. The circumstances of discovery of the TPSL may be based on otological and extra-otological signs. In addition of otological signs such as purulent otorrhea, earache, hearing loss and retro ear swelling; Persistent headaches with neck pain may be observed. Subsequently hydrocephalus with vomiting and papillary edema, to a septic-pyohemic table [6]. In our patient the predominant signs were otological. Classical signs like picket-fence fevers and the sign of Griesenger [1,2,6]. These signs may be masked by previous antibiotic therapy. The previous antibiotherapy in our patient is the illustration of the absence of these classical signs. The bacteriological profile of otogenic thrombophlebitis of the lateral sinus is various: anaerobes (Fusobacterium necrophorum, anaerobic streptococci, Bacteroides sp.); gram negative bacilli (Proteus and Pseudomonas); staphylococcus, pneumococcus [6]. Fusobacterium necrophorum, a producer of coagulant enzymes, is implicated in the genesis of lateral sinus thrombosis [7]. Bacteriological analysis has highlighted Enterococcus Avium, an unusual anaerobic germ susceptible to clarytromycin as in the Au KJ et al. [2]. Computed tomography can confirm the diagnosis by highlighting the delta sign that is traditional [2,8,9]. It is characterized by opacity of the lateral venous sinus on non-injected images and absence of venous opacification accompanied by enhancement of the contrast of the adjacent hard mother on post-injection images. Indirect signs may also manifest as an increase in caliber of collateral and contralateral vessels by altering blood flow. The main sign found in our patient was the sign of Delta testifying the thrombosis this thrombosis was extended to the internal jugular vein.
Computed tomography can be normal by giving a false positive in 15 to 27%. In a series of 46 patients; we noticed sensitivity in 87% of cases. The sensitivity of the MRI was noticed in 100% in 30 patients [2]. Venous angiography and angio-MRI are much more sensitive exams. On angiography at venous time, there is an image of endoluminal subtraction which corresponds to the thrombus, with no flow. The examination makes it possible to specify the extension of the thrombus and specially to check the integrity of the contralateral sigmoid sinus. MRI shows a T1 and T2 hyper signal in the thrombosed lateral venous sinus and a decrease or absence of flow [6].
The management of the TPSL includes antibiotic therapy; mastoidectomy with or without anticoagulation [2]. It has developed over the years from mastoidectomy with puncture to the fine needle of the lateral sinus to conservative treatment without gesture on the vein. Recent studies have focused on masto-atticotomy without sinus opening with promoter results. The principle is based on the evacuation of bone sequestra with skeletalization of the lateral sinus. The results of this alternative have been successful according to the authors [2,5]. Recently, studies have shown the value of non-surgical conservative treatment [4,8,10]. In the Wong I series, three patients were treated successfully [8]. Tov E treated a case of lateral sinus thrombophlebitis with antibiotic therapy alone without mastoidectomy with recanalization. Our study illustrates the importance of non-surgical conservative treatment. This therapeutic attitude was indicated according to the following criteria: The preserved neurological state. Its occurrence on an acute otitis media treated by Singh G as a factor of good prognosis [5].
The absence of suppurative sign and bone sequestration and bone lysis on computed tomography were key elements of this decision. In addition to the absence of associated intracranial complications. These criteria were shared by Tov & Spandow O [4,10]. Cholesteatomata’s chronic otitis media should not be included in this setting because of the presence of lysis and bone sequestration. The duration of ant biotherapy of four weeks in our case is close to that Tov et al. [4]. According to our analysis, the treatment model does not influence the duration of antibiotic therapy, however for Raja K it is between four to eight weeks [9]. Antibiotic therapy in our patient in broad spectrum intravenous for a week and a relay per so for three weeks allowed a complete remission of clinical and paraclinical signs. The anticoagulant was not used in our patient as in the series of Even unlike the Spandow et al. [10]. The use of the anticoagulant remains subject of controversy [2].
Ella & Spandow et al. [4,10] reported the success of intravenous antibiotic therapy alone without surgery or associated with myringotomy and drainage of pus in the management of otogenic lateral sinus thrombophlebitis. However, in our case the presence of the antero-inferior perforation of the eardrum allowed to drain the contents of the box by letting out pus.
Conclusion
Thrombophlebitis of the lateral sinus is a potentially dangerous and lethal complication. Management of thrombophlebitis cases of the lateral sinus requires an evaluation of the clinical and Para clinical parameters of the patient to propose a therapeutic alternative. Myringotomy with the use of antibiotics without surgery allows recanalization of the lateral sinus. An increased monitoring requires a high index of suspicion in the early detection of signs of thrombus spread, with the concomitant occurrence of intra- and extra-cranial complications
References
- Funamura JL, Nguyen AT, Diaz RC (2014) Otogenic lateral sinus thrombosis : Cases series and controversies. Int J Pediatr Otorhinolaryngol 78(5): 866-870.
- Au J K, Adam SI, Michaelides EM (2013) Contemporary management of pediatric lateral sinus thrombosis : A twenty year review. American journal of otolaryngology head and neck medecine and surgery 34(2): 145-150.
- Viswanatha B, Deepthi P (2018) Lateral sinus thrombosis. Austin ENT Open Access 2(1): 1005.
- Tov EE, Leiberman A, Shelef I, Kaplan DM (2008) Conservative nonsurgical treatment of a child with otogenic lateral sinus thrombosis. American journal of otolaryngology -Head and Neck Medecine and Surgery 29(2): 138-141.
- Singh GB, Arora R, Garg S, Kumar D, Rajan S, et al. (2016) Septic lateral sinus thrombosis : Sinus exploration is unnecessary. Case report in otolaryngology 2016(1): 4.
- Viswanatha B, Thriveni CN, Naseeruddin K (2014) Nonseptic and septic lateral sinus thrombosis: A review. Indian J Otolaryngol Head Neck Surg 66(Suppl 1): S10-S15
- François M (2005) Complications des otites moyennes aigues et chroniques, EMC-Oto-rhino-laryngologie 2(1): 92-106
- Wong I, Kozak FK, Poskitt K, Ludemann JP, Harriman M (1935) Pediatric lateral sinus thrombosis: retrospective case series and literature review. J Otolaryngol 22: 131-142.
- Raja K, Parida PK, Alexander A, Surianayanan G (2017) Otogenic lateral sinus thrombosis : A review of fifteen patients and changing trends in the management. Int Arch otorhinolaryngol 22(3): 208-213.
- Spandow O, Gothefors L, Fagerlund M, Kristensen B, Holm S (2000) Lateral sinus thrombosis after untreated otitis media. Aclinical problem-again? Eur Arch Otorhinolaryngol 257(1): 1-5.
© 2018 Fatogoma Issa K. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)














.bmp)
.jpg)
.png)
.jpg)










.jpg)






.png)

.png)



.png)






