- Submissions

Full Text
Modern Applications in Pharmacy & Pharmacology
The Health and can Overcome this Infection. The Author Presents Some Data of Covid-19 from the Jan, 2020 till Coronavirus (Sars- Cov-2) with Special Emphasis on Diabetes Mellitus (DM): A Short Communication
Ajmal R Bhat1,2*, Rajendra S Dongre2, Zahoor A Ganie3, Mohammad S Akhter4, Firdoos A Itoo1 and Siraj Yousf parray1
1Department of Science, India
2Department of Chemistry, India
3Faculty of Engineering, India
4Department of Chemistry, Bahrain
*Corresponding author: Ajmal R Bhat, Faculty of Science, India
Submission: May 28, 2021;Published: April 13, 2022
ISSN 2637-7756Volume2 Issue5
Abstract
The recent emergence of the novel, pathogenic SARS-coronavirus 2 (SARS-Cov-2) in China and its rapid national and international spread create a global health crisis. Angiotensin-Converting Enzyme 2 (ACE2) is the cellular receptor for SARS coronavirus (SARS-CoV) and the new coronavirus (SARS-CoV-2) causing the serious epidemic COVID-19. The novel SARS-CoV-2 is a warning for the metabolic disorder patients especially diabetes mellitus due to weak immunity system of the patient’s body and thereby more susceptible to coronavirus infections. The diabetic patients protecting against COVID-19 include social distancing of at least six feet, use of face masks, washing hands often with soap or sanitizer, use of water for at least 20 seconds and making sure you are up to date with vaccinations like the flu and pneumonia shot. The use of powerful antioxidant glutathione and a bioflavonoid quercetin may prevent various infections including COVID-19. The minerals like Magnesium and Zinc, micronutrients, herbs, food rich in vitamins C, D and E, and better life style can promote April 16th, 2020.
Keywords: SARS-CoV-2; Angiotensin-converting enzyme 2; Endocrinological disorder; Immune system; Diabetes mellitus; Prevention
Introduction
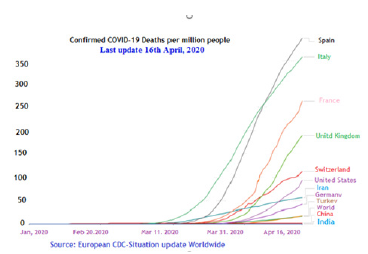
In the 21st century, 2 highly pathogenic HCoVs-severe acute respiratory syndrome coronavirus (SARS-CoV) and middle east respiratory syndrome coronavirus (MERS-CoV)- emerged from animal reservoirs to cause global epidemics with alarming morbidity and mortality. The pathogenic human coronaviruses (HCoVs) called coronavirus (2019-nCoV) or (COVID-19), began in Wuhan, China, in late 2019. By early March 2020, the novel coronavirus now named as SARS-CoV-2, which had spread to 210 Countries and territories around the world. The total globally cases were found 2,056,055 out of which 511,019 cases has recovered and 134,178 has deaths as of April 16, 2020. The ultimate scope and effect of this outbreak is unclear at present as the situation is rapidly evolving and has been officially declared a global pandemic by WHO [1]. The incubation period of (COVID-19), is 2 to 14 days. This means people can be exposed and spread the virus for days or weeks before even developing any symptoms. The mortality rate is 3.4% estimate by the WHO as of March 3, 2020. Coronaviruses are large, enveloped, positive strand RNA viruses that divided into 4 genera: Alpha, Beta, Delta, and Gamma, of which alpha and Beta CoVs are known to infect humans [2]. The SARSCoV- 2 is a positive-strand RNA virus that causes severe respiratory syndrome in human. The genome of SARS-CoV-2 shares about 80% identity with that of SARS-CoV and is about 96% identical to the bat coro-navirus BatCoV RaTG13 [3]. Four HCoVs (HCoV 229E, NL63, OC43, and HKU1) are endemic globally and usually cause mild to moderate upper-respiratory tract illnesses. Coronaviruses are ecologically diverse with the greatest variety seen in bats, suggesting that they are the reservoirs for many of these viruses [4]. Peridomestic mammals may serve as intermediate hosts, facilitating recombination and mutation events with expansion of genetic diversity. The novel coronaviruses, SARS-CoV-2 particles are spherical and have proteins called spikes protruding from their surface. These spikes latch onto human cells, and undergo a structural change that allows the viral membrane to fuse with the cell membrane (Figure 1). Spike protein mediates the fusion of host and viral cell membrane to begin infection and is the major target for neutralizing antibodies and vaccine development [5,6]. Protein modeling suggests that there is a strong interaction between the spike protein receptor-binding domain and its host receptor Angiotensin-Converting Enzyme 2 (ACE2), which regulate both the cross-species and human-to-human transmissions of COVID-19 [7]. Therefore SARS-CoV-2 infection is caused by binding of the viral surface spike protein to the human Angiotensin Converting Enzyme 2(ACE2) receptor following activation of the spike protein by Transmembrane Protease Serine 2 (TMPRSS2) [8]. The spike protein is a large type-I transmembrane protein containing two subunits, S1 (in red below) and S2 (in green below). S1 (red) contains a receptor-binding domain, which is responsible for recognizing the cell surface receptor. S2 (green) contains the transmembrane domain, which anchors the spike protein to the viral envelope and also has the elements needed for membrane fusion to initiate viral entry into the host cell. The viral genes enter the host cell to be copied, producing more viruses. Recent work shows that, SARS-CoV-2 spikes bind to receptors on the human cell surface called Angiotensin Converting Enzyme 2 (ACE2). The Angiotensin Converting Enzyme (ACE2) reduces blood pressure and inflammation and acts like a “door” to the cell for the virus which causes COVID-19. When the virus attaches to ACE2 receptors and makes its way into cells, it “hijacks” cells and makes copies of itself. When the virus is done, it kills the cells and spreads. Once its in, the virus replicates and kills the cells that it enters, causing fever, shortness of breath and other symptoms that can lead to severe illness or death. The SARS-CoV-2 spike 10 to 20 times more likely to bind ACE2 on human cells than the spike from the SARS virus from 2002. This may enable SARS-CoV-2 to spread more easily from person to person than the earlier virus. Further the diseases damages the lungs both by killing cells and by prompting a response from the immune system. The immune system can overreact and cause damage while trying to kill the virus. When infection affects the air sacs in the lungs which facilitate gas exchange, there will be fluid and pus that accumulate, which can cause pneumonia. The lungs become severely inflamed and injured, patients can develop acute respiratory distress syndrome, or ARDS. Fluid begins leaking into the lung, making it incredibly difficult for patients to breathe. SARS-CoV-2 is spread predominantly via respiratory droplets when a person coughs or sneezes (Figure 2). It also spreads when someone touches a contaminated surface such as a door handle. Common symptoms of SARS included fever, cough, dyspnea, and occasionally watery diarrhea. These are associated with the common pneumonia, Severe Acute Respiratory Syndrome (SARS) and can also affect the gut. Transmission may occur from both symptomatic and asymptomatic patients, with secondary infection rates ranging 0.5-5%. [9,10]. SARS-CoV-2 has been demonstrated to remain stable for up to 3 hours in the aerosolized form, up to 24 hours on cardboard, and as many as three days on plastic or stainless steel [11]. For infected patients, 20% to 30% required mechanical ventilation, 10% died and higher fatality rates in older patients and those with medical comorbidities. COVID-19 has higher prevalence of diabetic disease (7.3%), after the cardiovascular disease (10.5%) due to the weak immunity system of the patient’s body and thereby easily attack by Virus. As a transmembrane protein, Angiotensin Converting Enzyme 2 (ACE2) attached to the outer surface of the cells and serves as the entry point for corona virus [12]. The binding of the spike S1 protein of SARS-CoV2 to the enzymatic domain of ACE2 on the surface of cells results in endocytosis and the enzyme into endosomes located within cells [13,14]. The severe and critically ill patients with COVID-19 had higher occurrence of hypokalemia that resulted from renal potassium wasting. This can be explained by downregulation of ACE2 following viral intrusion resulting in decreased degradation of angiotensin-II, increased aldosterone secretion and subsequent increased urinary potassium loss. Thus, ACE2 overexpression, while facilitating entry of SARS-CoV-2, is unable to protect against lung injury as the enzyme gets degraded by the virus. ACE2 expression is reduced in patients with DM due to glycosylation, which increased predisposition to severe lung injury and ARDS with COVID-19. Diabetes mellitus is an endocrinological disorder with an increasing global occurrence and incidence. The person with diabetes is a host of other chronic diseases including cardiovascular diseases, kidney-related conditions, and others. Diabetes is a metabolic disorder that exposes to varied infections due to weakens the immunity system of the patient’s body. The World Health Organization (WHO) warns that the most at-risk populations of COVID-19 are: older persons and persons with preexisting medical conditions shows to develop more serious illness when they contract the virus. People with chronic conditions like diabetes are at greater risk of being hospitalized due to the coronavirus, because glucose levels are fluctuating or elevated consistently. Diabetic ketoacidosis is precipitated or complicated by an infection in 75% of the cases. The mortality rate of patients with an infection and ketoacidosis is high. The question then arises as to which pathogenetic mechanisms are responsible for this high infection rate in patients with DM. Possible causes include defects in immunity, an increased adherence of microorganisms to diabetic cells. In humans, the immune system protects the person from outside invaders (also known as pathogens), such as bacteria or viruses. The diabetes and the immune system are directly connected and patients with diabetes mellitus (DM) have infections more often than those without DM [15]. One of the possible causes of this increased prevalence of infections is defects in immunity. When a healthy individual is invaded by foreign bacteria or a virus, the immune system will work on attacking that virus or bacteria and destroying it. With type 1 diabetes, the immune system will actually misdirect its signals to attack the bacteria and instead will attack the insulin-producing beta cells in the body and occurs in genetically predisposed individuals. Type 2 diabetes also results due to autoimmune disorder, therefore physical activity is recommended for type 2 diabetics to help keep blood sugar under control as well as keeping the immune system strong. Without insulin, the glucose from the food cannot be utilized efficiently and patients experience high blood glucose levels. The high levels of blood glucose often experienced by diabetes patients have also been held responsible for the weak immune system. Besides, in diabetes, the response of the immunity system towards bacteria and viruses also reduces to a great extent, causing infections and other diseases in diabetes patients. Thus hyperglycemia may be a cause of dysfunction of the immune response, which results in failure to control the spread of invading pathogens in diabetic subjects, making diabetics more susceptible to coronavirus infections. Thus patients of diabetes have a lower immune response, so risk of getting sicker quicker. There have also underlying risk of exacerbated illness simply due to having diabetes even if glucose levels are in range. The American Diabetes Association explains, In China, where most cases have occurred so far, people with diabetes had much higher rates of serious complications and death than people without diabetes. The Journal of the American Medical Association (JAMA) reports on a higher case-fatality rate among those with preexising conditions are 10.5 percent for cardiovascular disease, 7.3 percent for diabetes. 6.3 percent for chronic respiratory disease, 6.0 percent for hypertension and 5.6 percent for cancer. The case fatality rate (CFR, number of deaths/number of those diagnosed) vary by location and an individual’s age. According to the China CDC Weekly study, in Hubei Province of China, the epicenter of the outbreak, the death rate reached 2.9%; in other provinces of China, that rate was just 0.4%, In addition, older adults have been hit the hardest. The death rate 14.8% in those 80 and older; among those ages 70 to 79, the COVID-19 death rate in China seems to be about 8%; it’s 3.6% for those ages 60 to 69; 1.3% for 50 to 59; 0.4% for the age group 40 to 49; and just 0.2% for people ages 10 to 39. No deaths in children under 9 have been reported. Based on reported data from April 16th, 2020, the CFR varies significantly by country [16]: Italy (13.11%), Hungary (8.6%), Honduras (8.22%), World (6.72%), Iran (6.25%), Brazil (6.13), United States (4.84%), China (4.01%), Canada (3.56), India (3.34%), Germany (2.74%), South Korea (2.16%), Pakistan (1.91%), Thailand (1.72%), Australia (0.98%), Russia (0.81%), Iceland (0.46%).1 (Figure 3). According to early estimates by China’s National Health Commission (NHC), about 80% of those who died were over the age of 60 and 75% of them had pre-existing health conditions have a significantly increased CFR: 10.5% for cardiovascular disease (CVD); 7.3% for Diabetes Mellitus (DM); 6.3% for COPD; 6% for HTN; and 5.6% for cancer [17]. The confirmed Covid-19 deaths of most affected countries till April 16, 2010 are: Spain 19,130 (Cases 182,816), Italy 22,170 (Cases 168,941), France 17,920 (Cases 147,863), United Kingdom 13,729 (Cases 103,093), Switzerland 1,281 (Cases 26,732), Iran 4,869(Cases77,995), Germany 3,867 (Cases 135,663), Turkey 1,643 (Cases 74,193), China 3,342 (Cases 82,341), India 423(Cases 12,759) and overall world 144,104 (total cases 2,146,390) (Figure 4). As per the biochemical processes, beta-defensins are the compounds that help to build a strong immune system of the body. When glucose in the body is high, it breaks down into a molecule known as dicarbonyls. It is this compound that disrupts the smooth functioning of the beta-defensins. The dicarbonyls, namely methylglyoxal, and glyoxal weaken the ability of the beta-defensins to fight infections..
Figure 1:Structure of novel coronavirus SARS-CoV-2 using host cell.
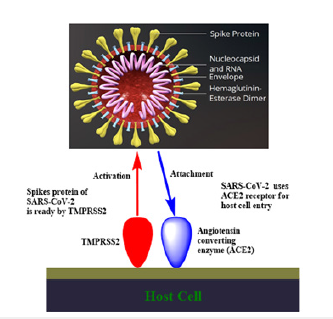
Figure 2:Symptomes of COVID-19 and its mode of spread.
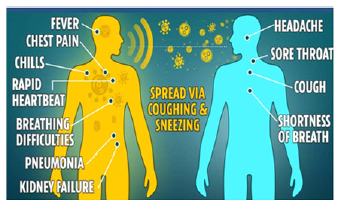
Figure 3: Case Fatality rate (CFR) of COVID-19 of most affected countries.
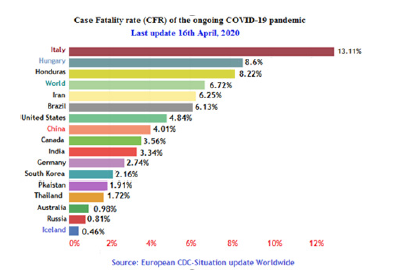
Figure 4: Confirmed deaths of top most affected countries, till April 16th, 2020.
Boost immunity of Diabetes Mellitus (DM)
i. Try to manage weight effectively. Overweight effect the
immune system.
ii. Never skip meals and eat small portions of food at one go.
iii. Eat plant foods like fibers which boost immunity system
of the body.
iv. Regular exercise will boost the immunity and control
body weight.
v. Regularly monitor blood glucose and keep the same under
check.
vi. Use probiotics to boost the immune system. Probiotics
are the good bacteria that are required by the body. Apart from the
probiotic supplements, there are a number of natural food items
that are probiotic by their very nature.
vii. Some of important natural sources that helps boost
immunity system include herbal tea, black tea as they are known to
contain essential flavonoids, polyphenols, that help in maintaining
the levels of blood glucose.
viii. The most important reason for weakened immunity, as
suggested by various experts is stress. The hormones released
when you are stressed out lead to loss of essential immunity in the
body. By practicing meditation, yoga and other physical and mental
activities reduce and eliminate stress from your life.
ix. Sleep well and soundly. Whatever hard work put in to
boost your immunity system, it will all be a waste if do not take
adequate sleep at night.
x. Eliminate smoking and alcohol drinking to a large amount
to boost immunity.
Thus, by applying the above-mentioned simple and easysteps, which boost the immunity system in diabetes and lead to fight any virus especially the Covid-19 and hence live a healthy as well as happy life.
Preventive measures of Diabetes Mellitus (DM) from Coronavirus
Preventive measures are the best strategy for novel coronavirus (SARS-CoV-2) at this time. While vaccines and monoclonal antibodies against SARS-CoV-2 are in development, a number of other investigational therapies, using repurposed clinically approved drugs targeting SARS-CoV-2 cell invasion and replication, may be considered. Based on the information from health authorities including Centers for Disease Control and Prevention (CDC) agency resources, World Health Organization (WHO), and credentialed medical professionals within and beyond the diabetes space. The diabetic patients protecting against COVID-19 include social distancing of at least six feet, use of face masks, washing hands often with soap or sanitizer and water for at least 20 seconds, and making sure you are up to date with vaccinations like the Flu and Pneumonia shot. Further keep hands away from the eyes, nose, and mouth, because that allows germs that cause respiratory infections to enter the body. Keep distance or just try to be very cautious about physical contact with people who have signs of respiratory illnesses who are coughing, sneezing, etc. A humid environment is also beneficial. If the house is dry, especially in the wintertime, use a humidifier. Patients of Diabetes Mellitus (DM) must have plethora of water, as that will keep their mucous membranes moist which can further lower the chances of cold and flu. Further use of plenty of water, minerals like Magnesium and Zinc, micronutrients, herbs, food rich in vitamins C, D and E, and better life style one can promote the health and can overcome this infection. Various studies showed that a powerful antioxidant glutathione and a bioflavonoid quercetin may prevent various infections including COVID-19. The first place where germs can penetrate into the body is the nasal passages and if they dry out due to dry air, keep opening the door and marshaling germs into your system. The most important issue is managing the glucose, which becomes more challenging, but even more important, because when glucose levels are elevated, you are sort of help and assisting the infection of virus (Covid-19), which can easily enter the body. Thus patient feeding the enemy in a way if blood sugar is poorly controlled. Further for high blood sugar patients, the recovery time is extended and cause varied symptoms that is much worse for the whole body. The most important precaution measures for diabetic patients are self quarantining. However using insulin, needs at least the week ahead’s supply, and must needed to know how to adjust your insulin doses to maintain healthy blood sugar levels. Further make sure you have enough medication available to manage your diabetes. In general, it is good idea to have a friend, family member, or trusted neighbor so that they can bring you groceries or call your doctor in case you are not well. They should be someone who understands your history of diabetes and can help you during the pandemic situations.
Conclusion
Covid-19, caused by SARS-CoV-2, is a global pandemic declared by WHO. The ultimate scope and effect of this outbreak is unclear at present as the situation is rapidly evolving. Emergency efforts are underway to find optimum medical products to prevent infection and diagnose and treat patients during the coronavirus disease 2019 (COVID-19) pandemic, but none with proven clinical efficacy to date. Production and supply chains for COVID-19 drugs (such as chloroquine and hydroxychloroquine), and for many other essential medical products, are being impaired by this crisis. Supply chains for vital drugs for other diseases (such as cardiovascular disease, diabetes mellitus, cancer, systemic lupus erythematosus etc) are being disrupted because they are being repurposed to use against COVID-19, without adequate supporting evidence. For diabetes mellitus, self-quarantine and social distancing is the best option to prevent from alarming Covid-19 disease. Use of soap or sanitizers for hand washing can minimises the chances of infection. The plantbased foods play a vital role to enhance the immunity of people to control of COVID-19. Thus prevention is the best option to fight against Covid-19.
Acknowledgement
Special thanks to my colleagues namely Dr. Kursheed Ahmad Wani, Dr. Mohd. Shafia Bhat and Dr. Javed Ahmad Wani for their kind suggestions during the preparation of the manuscript.
References
- (2020) WHO Director generals opening remarks at the media briefing on COVID-19-11 March 2020.
- De Wilde AH, Snijder EJ, Kikkert M, Van Hemert MJ (2018) Host factors in coronavirus replication. Curr Top Microbiol Immunol 419: 1-42.
- Zhou P, Yang XL, Wang XG, Hu B, Zhang L, et al. (2020) A pneumonia outbreak associated with a new coronavirus of probable bat origin. Nature 588(7836).
- Emmie DW, Neeltje VD, Darryl F, Vincent JM (2016) SARS and MERS: recent insights into emerging coronaviruses. Nature Reviews Microbiology 14(8): 523-534.
- Belouzard S, Millet JK, Licitra BN, Whittaker GR (2012) Mechanisms of coronavirus cell entry mediated by the viral spike protein. Viruses 4(6): 1011-33.
- Jong SL, Haryoung P, Dong PH, Seung PH, Kwang K, et al. (2006) Mucosal immunization with surface-displayed severe acute respiratory syndrome coronavirus spike protein on lactobacillus casei induces neutralizing antibodies in mice. J Virol 80(8): 4079-4087.
- Yushun W, Jian S, Rachel G , Ralph SB, Fang Li (2020) Receptor recognition by the novel coronavirus from wuhan: an analysis based on decade-long structural studies of SARS Coronavirus. J Virol 94(7).
- Hoffmann M, Kleine Weber H, Schroeder S, Krüger N, Herrler T, et al. (2020) SARS-CoV-2 Cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell 181(2): 271-280.
- Zou L, Ruan F, Huang M, Liang L, Huang H, et al. (2020) SARS-CoV-2 Viral load in upper respiratory specimens of infected patients. New Eng J Med 382(12): 1177-1179.
- (2020) World Health Organization. Report of the WHO-China joint mission on coronavirus disease 2019 (COVID-19).
- Van DN, Bushmaker T, Morris DH, Holbrook MG, Gamble A, et al. (2020) Aerosol and surface stability of SARS-CoV-2 as compared with SARS-CoV-1. New Eng J Med 382(16): 1564-1567.
- (2020) ACE2 Angiotensin converting enzyme 2. National Center for Biotechnology Information (NCBI), National Library of Medicine, USA.
- Wang H, Yang P, Liu K, Guo F, Zhang Y, et al. (2008) SARS Coronavirus entry into host cells through a novel clathrin- and caveolae-independent endocytic pathway. Cell Research 18(2): 290-301.
- Jean KM, Gary RW (2018) Physiology and molecular triggers for SARA-CoV membrane fusion and entry into host cell. Virology 517: 3-8.
- Deresinski S (1995) Infections in the diabetic patient: Strategies for the clinician. Infect Dis Rep 1: 1-12.
- https://www.worldometers.info/coronavirus/worldwide-graphs/
- Wu Z, McGoogan JM (2020) Characteristics of and important lessons from the Coronavirus Disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the chinese center for disease control and prevention. JAMA 323(13): 1239-1242.
© 2022 Ajmal R Bhat. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






