- Submissions

Full Text
Techniques in Neurosurgery & Neurology
Complex Neurological Decision
Ghassan Haddad*
Serhal Hospital, Lebanon
*Corresponding author: Ghassan Haddad, Serhal Hospital, Lebanon
Submission: May 15, 2018; Published: May 22, 2018

ISSN 2637-7748
Volume1 Issue4
Editorial
Neurologists are faced with one great challenge when facing patients with atrial fibrillation who developed an acute ischemic stroke. One question arises.
When to initiate or resume anticoagulation to prevent a recurrent stroke or embolization?
Review of the literature reveals 2 views
1. The first view was a Cochrane reviews done in 2008 that showed that early anticoagulation within two weeks of stroke onset was associated with fewer recurrent strokes compared to no anticoagulation but at the costs of increased symptomatic intracranial hemorrhages. The conclusion was that early anticoagulation did not improve outcomes [1].
Another studies done by Italians scientist showed that early anticoagulations within 48 hours of stroke had no benefit compared to aspirin or placebo [2].
2. The second view was outlined in 2 major studies:
a. The first study is The Virtual International Stroke Trials Archive (VISTA), a cohort analysis of data from more than 10,000 patients with ischemic strokes and atrial fibrillation at 2 days after a stroke had a better outcome and associated with lower recurrent stroke and death [3].
b. The second study is The Early Recurrence and Cerebral Bleeding in Acute Ischemic Stroke and AF (RAF) that showed that antocoagulations started between 4 and 14 days after stroke had a better outcome with reduced stroke, systemic embolisation, major extracranial bleeding and symptomatic intracranial bleeding [4].
Factors that might influence the Neurologist decision on which view to adopt include the CHA2DS2VAS tool. This tool created by Dr Lips and colleagues from the University of Birmingham may be helpful [5].
A. CHA2DS2VAS tool
In this tool, every letter refers to a condition that patients with stroke have as described in the table above and each condition is assigned a score.
For example the letter C in the tool stands for Congestive heart failure (CHF) and patients with CHF are assigned a score of 1. A stands for Age and is assigned a score of 2.
Totals are them calculated for each patient and review of the percentage of ischemic event is obtained from Table 1. For patients with low risk i.e. no associated medical conditions listed from table one, these patients are at a zero risk of having a recurrent Thromboembolic Events (TE) and hence a delay in anticoagulation to 7 days or more may be justified.
Table 1.
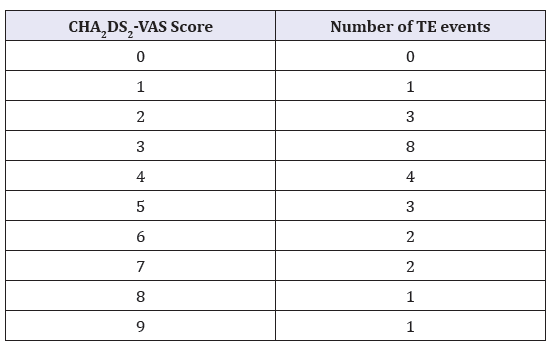
Table 2.
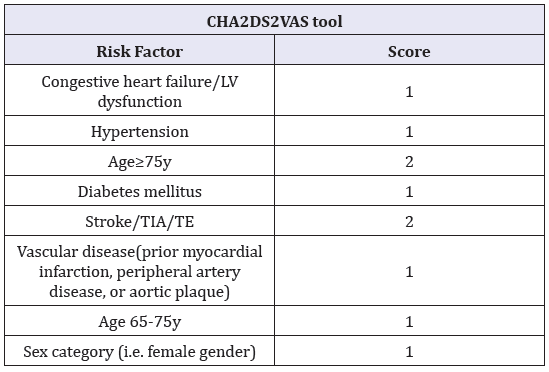
For patients with intermediate risk, i.e. a total score of 1-2 are at a moderate risk of having a recurrent Thromboembolic Events (TE) and hence a delay in anticoagulation to 4 days or more may be justified. For patients with multiple medical conditions listed in Table 2 i.e. a total score of 3 or more, are at a high rate of recurrence of ischemic event and hence early anticoagulation with 2 days delay may be justified.
References
- Sandercock PA, Counsell C, Kamal AK (2008) Cochrane Database Syst Rev (4): CD000024.
- Paciaroni M, Agnelli G, Micheli S, Caso V (2007) Stroke. 38(2): 423-430.
- Abdul-Rahim AH, Fulton RL, Frank B, Tatlisumak T, Paciaroni M, et al. (2015) Eur J Neurol 22(7): 1048-1055. doi: 10.1111/ene.12577.
- Paciaroni M, Agnelli G, Falocci N, Caso V, Becattini C, et al. (2015) Stroke. 46(8): 2175-2182.
- Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ (2010) Chest. 137(2): 263-272.
© 2018 Ghassan Haddad. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)





























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






