- Submissions

Full Text
Research in Pediatrics & Neonatology
Holoprosencephaly: A Case Study for Communicative and Swallowing Management
Muzeyyen Ciyiltepe1* and Zafer Unsal Coskun2
1Department of Speech and Language Therapy, Anadolu University Faculty of Health Sciences, Turkey
2Department of Radiology, Giresun Medical University, Turkey
*Corresponding author: Muzeyyen Ciyiltepe, Department of Speech and Language Therapy, Anadolu University Faculty of Health Sciences, Eskisehir, Yunus Emre Campus, Eskisehir, Turkey
Submission: November 07, 2017;Published: August 13, 2018

ISSN: 2576-9200 Volume2 Issue5
Introduction
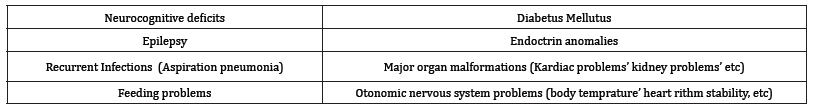
Holoprosencephaly (HP) is a developmental central nervous system defect characterized by advanced facial anomalies resulting from the complete separation of two lobes of the cerebral hemispheres Golden [1]. Prevalence is 1.31 in 10,000 births (Kahyaoglu, 2013). There is a parallel relationship between the combination of different etiological factors in different contributions and the changing clinical picture of the disease. Autosomal dominant and autosomal recessive inherited forms are reported in the literature (Croen LA, Shaw GM, 2000). Considering the studies on holoprosencephaly, developmental, neurological and medical problems were found in children with holoprosencephaly Ersin & Ertuğrul [2]. Table 1 lists the physical findings that can be seen in individuals with HP. Postnatal care of HP is multidisciplinary, symptomatic and long-lasting cognitive and physical supportive therapy. Prognosis depends on the size of the associated medical and neurological disorders (Table 2).
Table 1:Physical characteristics that can be seen in individuals with HP.
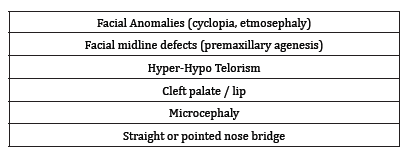
Table 2:some accompanying problems of HP.
There are HP and associated complications in the literature. However, in an HP case, language/speech impairment was not observed without dysphagia and craniofacial anomalies [3]. The purpose of this presentation is to share with you the therapeutic approach and results we have accomplished with this rare combination of severe neurocognitive-linguistic pathologies accompanied by severe dysphagia. We studied the case of a 24 month old girl with holoprosencephaly who was admitted to our hospital with difficulty swallowing. Mother was told about the possible problems prior to give birth as seen through ultrasound yet she and her husband chose not to terminate the pregnancy due to their religious beliefs (even though it was guaranteed by her medical primary care physician.
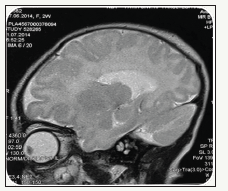
A multidisciplinary study of neurologist, nutritionist and dietician, language and speech therapist was provided during the diagnosis and screening period. Our case was born with a caesarean section at 38 weeks after completing the normal birth process and stayed in the cup for 28 days [4]. It has been learned that she has had long-term jaundice after birth. The birth weight of our case was 2760gr and the neck was 50cm. It was seen that the values of life and weight were close to norms when compared with their peers. But the case was microcephaly and the head circumference was 32cm (n=35cm). There is no consanguineous marriage in the family history. The head control of the child was weak and could not sit without support. When you want to lift the foot, you have flexion and adduction in the hips, shearing in the legs, knee flexion, and an equinovalgus posture in the ankle (Figure 1). It has been reported that the neurological examination is hypotonic and the emanation is weak, standing up. Cranial measurements are below normal. As seen the pictures (BBBB) are compatible with semi lobar holoprosencephaly and have the features of:
figure 1:Free stay of the child when lay on the bed.

A. Cerebral lobes are present but are fused anteriorly and at the thalami and then is partial diverticulation of the brain,
B. Absence of septum pellucidum,
C. Monoventricle with partially developed occipital and temporal horns,
D. Rudimentary falx cerebri: absent anteriorly,
E. Incompletely form interhemispheric fissure,
F. Fusion of thalami,
G. Agenesis of corpus collosum, and incomplete hippocampal formation.
Further, cavum septum pellucidum has not been observed, Lateral ventriculo-posterior horn width is 10mm and choroidal complex increases lateral wall distance. These results were also observed during fetal neurosonography that was also compatible with semi lobar holoprosencephaly. Posterior fossa is normal. At the time of clinical assessment, her eyes were able to follow visual and auditory stimuli. However, Denver Screening Test II Scores in combined with the AGTE (Ankara Developmental Test Inventory) indicated 3 months in general overall development age, 3 months in cognitive-linguistic skills development, 3 months in gross motor skills development in 3 months, and 3 months in social skill and self-care development 1 year and 2 months old. According to the findings of the anamnesis and the clinical evaluation, it was concluded that there was a “delay in cognitive development at a severe level”. It was observed that there was an increase in tonus in the lower extremities. It has been also observed that some reflexes are still present even though they are diminished long before with age matched normally developing peers; DTRs live, moro +/+, clonus+/+, babinski +/+. Tongue-trusting was the primary means of bolus propulsion anterio-posteriorly, in that it takes more time and energy and less success with bolus to reach from oral phase to pharyngeal phase to swallow. Her teeth development was also irregular with enabling her to close for biting and chewing. Her palatal arch was also high which effected her palatal reflex to be triggered on a timely fashion [5].
figure 2:Taping of the facial muscles for lip closure and tongue mobility.

The clinic multidisciplinary team management included 6 weeks of therapy per our policy with severe problems as such and then to refer to related services (child life specialist, physical therapist, special education day care centre and dietitian) for continuity of the rehabilitation process. She was seen three times a week for 2, 5 hours/week to one-to-one therapy. Therapy focused on following directives, produce primary sounds that are toward age appropriate sounds (from vocalizations to start with), stay on focus and keep focus for 5-10 minutes, and decrease meal time with advancing bolus consistencies toward age appropriate level: also with introducing different flavours other then milk, yoghurt and pudding. Implemented taping her face (Figure 2), thermaltactile stimulation of facial pillars and neuro-electro stimulation of cricohyoid area as well as facial musculatures. Below table shows before and after status of 18 visits of intervention (Table 3-5).
Table 3:Changes observed with therapy in the areas of speech/language.
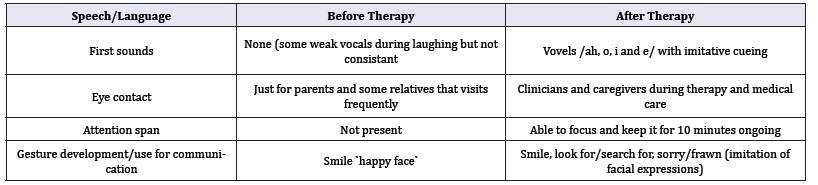
Table 4:Swallowing.
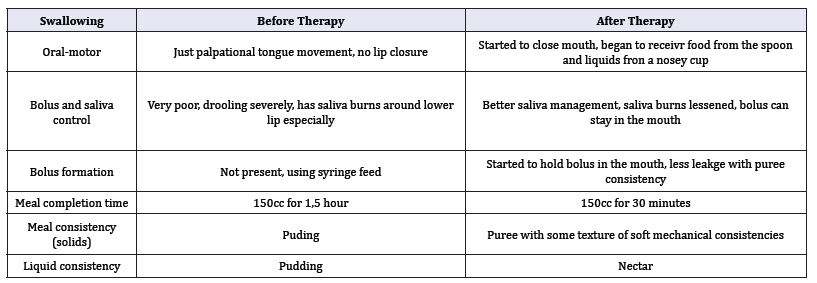
Table 5:Quality of life.
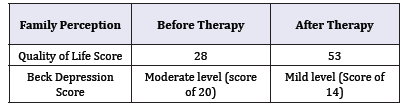
figure 3:Saggital (A), axial (B) and coronal (C) T2 weighted MR images.
To conclude, an intensive therapeutic intervention makes quality of life better for both family and the child’s sake. It is a win-win situation for being able to do things more with their child since feeding time is considerately lessened, the family is learned how to interact with the child (Figure 3) so that her vocalizations could be more productive turning into a communication style (sign plus some sounds and gestures in the future). Further therapeutic arrangements is also made that the family knows seating and positioning is need to be taken care of as well as the early child special education is a must for cognitive development.
References
- Golden JA (1998) Holoprosencephaly: A defect in brain patterning. J Neuropathol Exp Neurol 57: 991-999.
- Ersin N, Ertuğrul F, Saraç A, Aydoğdu S, Olgu BS (2005) Holoprozensefali, Ege Tıp Dergisi.
- Dubourg C, Bendavid C, Pasquier L, Henry C, Odent S, et al. (2007) Holoprosencephaly. Orphanet J Rare Dis 2: 8.
- Cohen MM (1982) An update on the holoprosencephalic disorders. The Journal of Pediatrics 101: 865-869.
- Çalışkan E, Öztürk N, Kaplan M, Dölen İ, Kandemir Ö, et al. (2004) Semilobar holoprozensefali: Olgu sunumu. Kadın Doğum Dergisi 2: 292- 293.
© 2018 Muzeyyen Ciyiltepe. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






