- Submissions

Full Text
Research in Medical & Engineering Sciences
Assessing Pain Using Morbid Motion Monitor System in the Pain Management of Nurse Practitioner
Mohammad Reza Dawoudi*
*Corresponding author:Mohammad Reza Dawoudi, International Degree programme in Nursing (Salo), Turku University of applied sciences, Turku, Finland
Submission: July 13, 2017; Published: August 21, 2017

ISSN : 2576-8816Volume1 Issue2
Introduction
Pain is an unpleasant sensory and emotional experience arising from actual or potential tissue damage [1]. Pain can be categorized into three primary types: somatic, visceral and neuropathic categories. Understanding the nature and patho physiological mechanism responsible is important since treatment approaches vary depending upon the type of pain a patient is experiencing [2]. Applying pharmacologic protocols for pain management requires proper evaluation, implementation, and monitoring [3]. To assist in this challenge, several types of biomedical technology have supported the development of tools to help the clinician with the assessment of pain and implementation of pain treatment regimens. Doctors who treat chronic pain often use a form like the Patient Comfort Assessment Guide to help them create a complete “picture” of a chronic pain problem [4]. This Patient Comfort Assessment Guide encompasses pain status, pain relief, other symptoms and side effects, as well as the impact of pain on the patient’s functional status. For clinical purposes, these components have proven helpful in monitoring and documenting the status of patients and their response to treatment interventions [5]. There are several tools available to reliably assess pain. The visual analog scale (VAS) is a common method for the quantification of pain severity. It is a continuous outcome measure consisting of a 100mm scale from 0 to 100 with low and high end points of no pain and worst pain [6]. The Faces Pain Scale-Revised (FPS-R) is (also) a self-report measure of pain intensity developed for children. It is adapted from the Faces Pain Scale to make it possible to score the sensation of pain on the widely accepted 0-to-10 metric [7]. Chronic pain may be classified as cancer pain or benign [8]. The Brief Pain Inventory (BPI) is a short, self-administered questionnaire that was developed for use in cancer patients. While most empirical research with the BPI has been in pain of that etiology, the questionnaire is increasingly evident in published studies of patients with non-cancer pain. All of these methods are based on self-report, observational (behavioral), or physiological data. However, quantifying and standardizing pain intensity in patients in an acute setting is a difficult task. Self- Report technique, which includes interview and questionnaire, have problem in applying direct behavioral observation to observe behaviors that happened during patient sessions. In these methods exaggerate symptoms provide inaccurate choice, especially if the answer must be taken from a predetermined list. To tackle these problems, we propose a new evaluation method based on morbid motion. The present study evaluated the motion of morbid which has been defined as the rate of pine and it is linked with various comorbid conditions. Furthermore, we have developed a novel tool for the assessment of chronic pain by standardized motion rate of morbid on bedside.
Methods and Materials
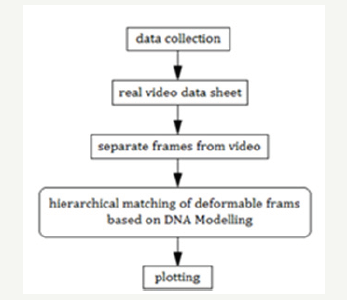
In this system Direct Behavioral Observation are used predominantly to collect quantitative and qualitative behavioral data in the domains of real morbid motion and interactive computer monitoring. The characteristics observations are included measuring the frequency, duration and topology of morbid motion, in a natural setting in the bedside. This information is collected from direct observations of a morbid behavior. Primaryinformation is collected to provide data regarding storing, analysis and presentation. These data generated by the hospital on the basis of Real Time Video Streaming for the period of bedside. Then this data is separated frame by frame. In the second step data matching technique describes efforts to compare two sets of collected frames. The matching score between two images is the Pain Scale (PS) between interval times of two images, and is determined by the union of corresponding points obtained from each region toimage match. We are also developed a matching technique solution to efficiently identify corresponding points for each region called DNA Modeling. The method is based on the linear mapping and the one-to-one correspondences between point features extracted from the frames and on calculating similarities in pixel values. This correspondence is determined by comparing two strings constructed from pixel values of the frames. The method uses a table called the Quarter Code table, which is the set of characters and numbers. In this table every number between 0 and 255 is translated into a unique string of four letter alphabet. Letters A, C, G, and T are chosen, since they are the same as used in DNA sequences. In this way it possible to utilize tools originally programmed to DNA sequences analysis. When all pixel values of frames (images) are converted to virtual DNA sequences, one can show the differences between two virtual DNA sequences. The comparison between two virtual DNA sequences is done by Chi-squared test, DNA Sequence Alignment Algorithms (Needleman Winch and Smith Waterman), Markov Chain and glm plot. The rate of similarity between frames is plotted as a graph and it’s appearing in Monitor. A general framework for document Morbid Motion Monitor is presented in Figure 1.
Figure 1: General framework for document morbid motion monitors (3M).
Conclusion
The system is used to show and describe the displacement of the morbid on the bedside. The amount of ill transmitted to the morbid increase the motion ratio. In this manner Motion Ration is the ratio of the displacement of the morbid. The matching score between two images which is called Pain Scale (PS) assist nurses and doctors in assessing the severity and quality of pain experienced by patients.
References
- (1979) Subcommittee on Taxonomy. Pain Terms: A List with Definitions and Notes on Usage Pain. International Association for the Study of Pain 6: 249-252.
- Schneider C, Yale SH, Larson M (2003) Principles of Pain Management. Clinical Medicine and Research 1(4): 337-340.
- Elizabeth JN (1978) Patient Comfort Assessment Guide. Partners against pain, Inc. H 5375 PAP023 05 /13 1(5): 373-378.
- http://www.nbcwashington.com/news/health/Patient_Comfort_ Assessment_Guide.html.
- Gregory G, Adam JS, Breena RT, Jasmin C, Hiran C, et al. (2010) Validation of the Wong-Baker FACES Pain Rating Scale in pediatric emergency department patients. Acad Emerg Med 17(1): 50-54.
- (2014) Faces Pain Scale-Revised Home, IASP.
- Thienhaus O, Cole BE (2002) Classification of pain. In: Weiner R (Ed.), Pain management: a practical guide for clinicians. Boca Raton: CRC Press, USA, p. 28.
- Keller S, Bann CM, Dodd SL, Schein J, Mendoza TR, et al. (2004) Validity of the brief pain inventory for use in documenting the outcomes of patients with noncancer pain. Clin J Pain 20(5): 309-318.
© 2017 Mohammad Reza Dawoudi. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






