- Submissions

Full Text
Open Journal of Cardiology & Heart Diseases
Short Term Outcomes after Use of Intracardiac Bone Stem Cell Transplantation for Management of Heart Failure: A Meta-Analysis
Saurabh A1, Rohit SL2*, Imtiaz I1, Navdeep G2, Anushree A1, Rohit RA3 and Roberto B4
1Creighton University, USA
2Medical College of Wisconsin, USA
3Chicago Medical School, USA
4Institute of Molecular Cardiology, USA
*Corresponding author: Rohit SL, Medical College of Wisconsin, USA
Submission: October 25, 2017; Published: December 05, 2017

ISSN: 2578-0204 Volume1 Issue1
Abstract
Introduction: The role of Bone marrow stem cell transplant in ischemic heart failure is being increasingly recognized. Multiple studies have been published their experience, demonstrating varying results. We aimed to perform a meta-analysis of the published literature.
Methods: We searched Pubmed, EBSCO and Cochrane databases for terms "bone marrow transplant”, "stem cell transplant”, "heart failure”, "cardiac failure” and their combinations. Only studies comparing Bone marrow stem cell transplantation via intracoronary route to placebo, and those with 6 month follow up data were included. Studies in languages other than English were excluded.
Results: Ejection fraction was significantly increased with the use of Bone marrow stem cell transplant compared to placebo (mean difference 6.16% 95%CI 4.16 to 8.16, p < 0.00001). No significant differences were observed in left ventricular (LV) end-systolic volume (mean difference -1.58 ml 95%CI -4.98 to 1.82, p = 0.36), LV end-diastolic volume (mean difference -0.77 ml 95%CI -3.75 to 2.22, p = 0.61) and mortality (odds ratio 1.08 95%CI 0.26 to 4.56, p = 0.92). Results of heterogeneity analysis showed significant heterogeneity only in the analysis of left ventricular ejection fraction (p = 0.01).
Conclusion: As compared to placebo, intracoronary Bone marrow stem cell transplant is associated with a 6% improvement left ventricular ejection fraction in ischemic heart failure patients at 6 month follow up.
Keywords: Bone marrow transplant; Heart failure; Intracoronary; Intramyocardial; Transepicardial
Introduction
Heart failure is a common, increasingly prevalent disorder in industrialized nations. The prevalence of HF has been projected to increase 46% from 2012 with anestimated8 million people over 18 years of expected to be living with heart failure in 2030 [1]. Though survival has improved with time, mortality still remains high, with more than 50% of people diagnosed with heart failure dying within 5 years [2]. Heart failure imposes a large cost burden on the healthcare system, with costs with projected total cost of $70 billion by 2030 [3].
Even though multiple drugs have been developed for the treatment of heart failure and have been shown to improve symptoms and/or survival, they do not address the underlying problem of loss of cardiac tissue in most cases. Stem cell transplant is an attractive therapeutic approach for heart failure since it has this potential. Various stem cell therapies have been studied for the treatment of heart failure. Bone marrow transplantation (BMT) is one of the modalities which has been attempted. Most of the preclinical and clinical studies have utilized bone marrow derived cells due to the ease in their procurement and a relatively greater concentration of stem cells in bone marrow [4]. Till date, there is inconclusive evidence regarding the short-term effectiveness of BMT in the treatment of HF. We aimed to perform a meta-analysis of published literature in this regard.
Methods
A systematic review of the literature was performed to identify manuscripts studying short-term outcomes after bone marrow transplantation for heart failure. The endpoints studied included left ventricular parameters and mortality. A review protocol was not available for the current study. The review was conducted using the PRISMA checklist.
Manuscript search and identification strategy
Electronic databases including PubMed, EMBASE, and Ovid were queried using the following search terms: "bone marrow transplant", "stem cell transplant”, "heart failure", "left ventricular ejection fraction” and "mortality”, and their various combinations. No specific restriction on year of publication was used. Resulting studies were then screened by title and abstract with manuscripts describing outcomes after bone marrow transplant being retrieved in their entirety. References of these were hand searched for additional relevant manuscripts. Inclusion criteria were studies comparing intra-cardiac route of bone marrow transplant with placebo and those reporting 6 month follow up data. Studies assessing effect of BMT in the setting of myocardial infarction and those in a language other than English were excluded.
These full text manuscripts were then reviewed for quality. Any disparities in scoring of manuscripts were then independently reviewed by another author. The Newcastle-Ottawa scale and Critical Appraisal Skills Program me (CASP) checklist were used to assess the quality of cohort studies. Published manuscripts available in full text were included in this review if they presented data from retrospective or prospective cohort studies or randomized controlled trials investigating the left ventricular parameters and mortality after 6 month follow up data. Left ventricular parameters studied included left ventricular ejection fraction (LVEF), left ventricular end systolic volume (LVESV) and left ventricular end diastolic volume (LVEDV). Studies were included in this analysis if they included at least one of the factors identified above.
Data extraction
Data regarding baseline patient characteristics and outcomes were extracted from the manuscripts identified for inclusion. Study level data were independently collected with use of a data collection tool. The data extraction was then reviewed to ensure integrity of the resulting data. If no information was available about a particular outcome this was designated separately. Authors of included studies were not contacted for additional data.
Bias analysis
Bias was assessed using the physiotherapy evidence database (PEDro) scale. Specifically, patient eligibility, randomization and concealment of allocation, blinding, completeness of outcome data, and statistical integrity were assessed using this scale.
Data analysis
Numeric data are presented as means with standard deviations or medians with ranges. Categorical data are presented as frequencies with absolute numbers as well as percentages. Results are presented as pooled odds ratios (OR) with 95% confidence intervals (CI) or as mean difference (MD) where appropriate. Heterogeneity between studies was identified using chi-square and I2 tests. For outcomes with no significant heterogeneity present, a fixed effects model was used. A random effects model was used if either the p-value was significant or the I2 statistics was greater than 50%. P-values of ≤ 0.05 were considered statistically significant. This analysis was done using SPSS statistical software, version 20.0 (Chicago, IL). Meta-analysis and forest plot creation were done using Rev Man 5.0 (Cochrane Collaboration, Oxford, UK).
Results
Study selection
Figure 1: Initial search using the methodology outlined above yielded 26,739 manuscripts.
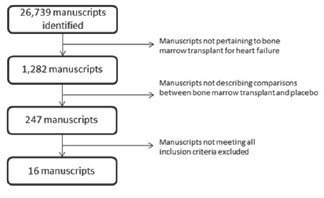
Initial search using the methodology outlined above yielded 26,739 manuscripts (Figure 1). After reviewing these studies using title and abstract, full text manuscripts were obtained for 247 of these studies. Of these studies, 16 were identified for inclusion in the analysis. There were a total of 699 patients across the studies.
Left ventricular ejection fraction
Data from 14 studies was pooled for analysis of left ventricular ejection fraction with 323 patients in the bone marrow group and 238 in the control group for a total of 561 patients (Table 1). A significant difference was noted in left ventricular ejection fraction with ejection fraction being higher in those undergoing bone marrow transplant. The mean difference noted was 6.16% with a 95 percent confidence interval of 4.16 to 8.16. A random effects model was utilized as heterogeneity was present as demonstrated by a chi-squared value of 21.21 (p=0.01) and an I2 of 52%.
Left ventricular end systolic volume
Data from 8 studies was pooled for analysis of left ventricular end systolic volume with 152 patients in the bone marrow group and 114 in the control group for a total of 266 patients (Table 2). No significant difference was noted in left ventricular end systolic volume with end systolic volume being lower in those undergoing bone marrow transplant. The mean difference noted was -1.58ml with a 95 percent confidence interval of -4.98 to 1.82. A fixed effects model was utilized as heterogeneity was not present as demonstrated by a chi-squared value of 9.42 (p=0.22) and an I2 of 26%.
Left ventricular end diastolic volume
Data from 10 studies was pooled for analysis of left ventricular end diastolic volume with 197 patients in the bone marrow group and 144 in the control group for a total of 341 patients (Table 3). No significant difference was noted in left ventricular end diastolic volume with ejection fraction being lower in those undergoing bone marrow transplant. The mean difference noted was -0.77ml with a 95 percent confidence interval of -3.75 to 2.22. A fixed effects model was utilized as heterogeneity was not present as demonstrated by a chi-squared value of 2.35 (p=0.90) and an I2 of 0%.
Table 1: Heterogeneity: Tau2=6.39; Chi2= 27.21, df= 13 (P = 0.01); I2= 52%.
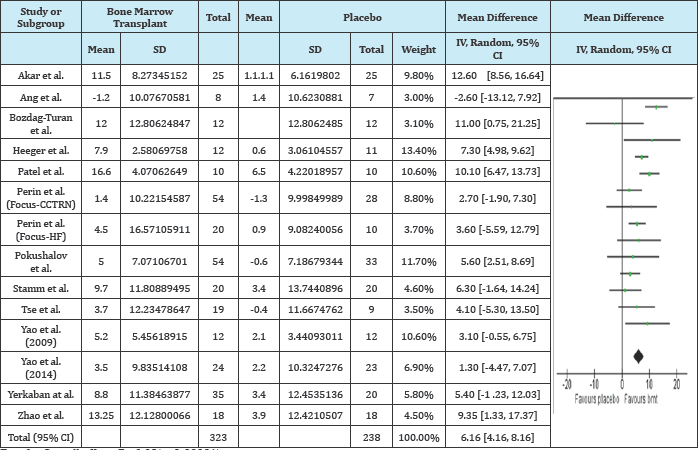
Test for Overall effect: Z= 6.03(p<0.00001).
Table 2: Heterogeneity: Chi2= 9.49, df= 13 (P = 0.22); I2= 26%.
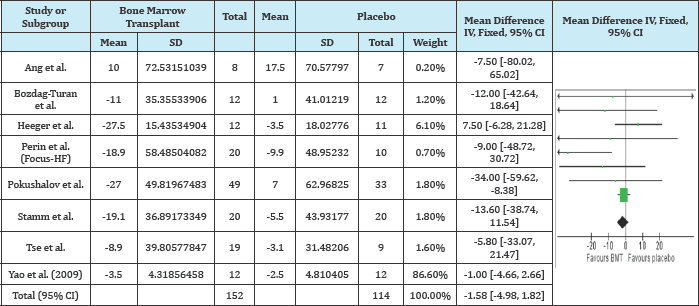
Test for Overall effect: Z= 0.91(p=0.36).
Table 3: Heterogeneity: Chi2= 2.35, df= 9 (P = 0.98); I2= 0%.
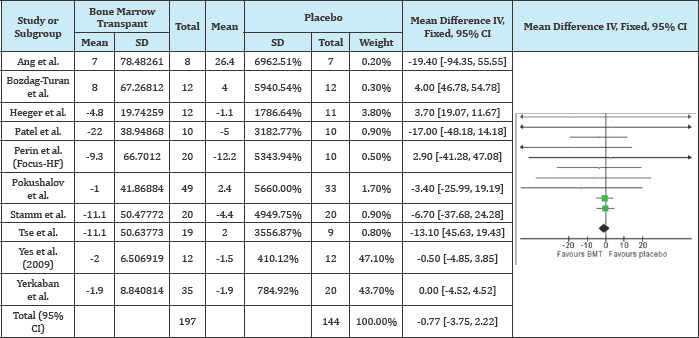
Test for Overall effect: Z= 0.50(p=0.61).
Mortality
Data from 16 studies was pooled for analysis of left ventricular end diastolic volume with 388 patients in the bone marrow group and 311 in the control group for a total of 699 patients (Table 4). No significant difference was noted in left ventricular end diastolic volume with an odds ratio of 1.08 with a 95 percent confidence interval 0.26 to 4.56. A fixed effects model was utilized as heterogeneity was not present.
Table 4: Heterogeneity: Chi2= 1.03, df= 3(P = 0.79); I2= 0%.
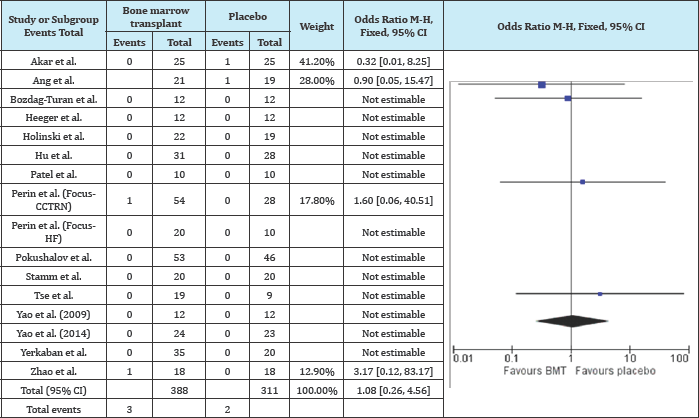
Test for Overall effect: Z= 0.10(p=0.92).
Discussion
Our study demonstrates that BMT leads to modest improvement in LVEF at 6 months with no effect on short term mortality when compared to placebo. LVESV and LVEDV did differ significantly between the BMT and placebo groups. To our knowledge, this is the first pooled analysis evaluating the short-term effects of BMT in patients with heart failure.
The term bone marrow mononuclear cells (BMMNCs) encompasses mesenchymal stem cells (MSCs), hematopoietic stem cells (HSCs), endothelial progenitor cells (EPCs) and other cell lines. They can be easily procured by density gradient centrifugation and do not require special techniques for culture [4]. In experimental models, BMT has been associated with conflicting results with studies showing benefit in dogs [5] and rats [6] and no benefit in sheep [7] and pigs [8]. The studies showing benefits have reported improvements in myocardial function, induction of angiogenesis and decrease in biomarkers like N-terminal pro brain natriuretic peptide levels. MSCs are multi potent stem cells that have also been reported to differentiate into cardio myocytes and endothelial cells [9,10]. Improvement in myocardial function9 and decrease in myocardial fibrosis10 has been reported with the use of MSCs in rats with both ischemic and non is chemiccardiomyopathy. HSCs differentiate into cells of both lymphoid and myeloid lineages while EPCs promote neovascularization by differentiating into endothelial cells [4].
Various hypotheses have been proposed for the mechanisms of beneficial effects with Bone Stem Cell s in patients with heart failure [4]. Trans-differentiation of Bone Stem Cell s into cardiac cells has been suggested as one mechanism though evidence has been conflicting [11,12]. Another possibility that has been suggested is the fusion of Bone Stem Cell s with recipient cardiomyocytes [13,14]. The major critique of trans-differentiation being the major or only mechanism is that the magnitude of functional benefits seen in the studies is disproportionate to the relatively small number of new differentiated cardiac cells. Angiogenesis has also been proposed as a possible mechanism for improvement in patients with ischemic heart failure but it cannot explain the improvement seen in those with non-ischemic cardiomyopathy or those with already infarcted myocardium [15,16]. Another mechanism called the paracrine hypothesis has been suggested which involves the concept of myocardial repair by release of cytokines, chemokines and growth factors [17]. Inhibition of apoptosis [17] and hypertrophy9may additionally result in improved LVEF and myocardial repair. Only one experimental study till date has compared Paracrine effects of different cell types in a heart failure model and found noticeable differences between cell types in terms of mediators, signal transductions and consequent effects [18].
Studies of stem cells in heart failure models have reported follow up periods ranging from 3 months to 5 years. Various methods have been employed to date for the delivery of stem cells including transendocardial, direct epicardial or intracoronary route. We pooled all studies using bone marrow derived stem cells irrespective of the route of administration. Cells are directly delivered into the LV wall using an injection catheter in the transendcardial approach while cells can be directly implanted in the scarred regions at the time of coronary artery bypass graft surgery in the transepicardial route. Intracoronary route employs delivery of cells using a catheter into a coronary artery and subsequent brief occlusion of the artery by catheter-tip balloon inflation to prevent washout of the transplanted cells. Only few studies have compared the route of administration of cells in heart failure model with widely varying results [19]. Studies involving the use of other type of stem cells like embryonic stem cells, skeletal myoblasts, cardiac stem cells and adipose derived MSCs were excluded from the study. The most effective cell type for cardiac regeneration is still unknown and it is unclear if a combination of cells will fare any better than individual cell types.
Our results suggest improvement in LVEF by 6% with BMT at 6 months when compared to placebo. This is likely to translate into significant improvement in patient's clinical status in some cases. Decisions like implantation of an implantable-cardioverter defibrillator or cardiac resynchronization therapy devices in a patient with heart failure may also be influenced with such improvement. However, compared to placebo, we did not find any improvement in mortality at 6 months with the use of BMT. This may be related to the short follow up when improvement in LVEF may not result in immediate difference in mortality. Interestingly, even though LVEF improved, there were no significant differences noted in LVESV and LVEDV. This may be related to fewer studies being pooled for LVESV and LVEDV endpoints compared to those pooled for LVEF. Larger prospective studies are needed to bridge such gaps in knowledge.
There are several limitations of this study. Firstly, we did not have access to patient-level data which predisposes our study to potential bias from unmeasured confounders. Secondly, we studied left ventricular parameters which may not be true surrogates of clinical status of the patient like NYHA class or future use of device therapy due to lack of enough data on such endpoints in studies. However, we did analyze short-term mortality as an endpoint. Thirdly, we pooled all studies irrespective of route of administration as long as they utilized bone marrow derived cells. As mentioned before, choice of route can influence outcomes in this setting. The strengths of the study include clear specifications of the follow up period without pooling widely varying follow up periods. Also, we pooled only studies using bone-marrow derived cells and excluded studies using other type of stem cells which may have different onset or duration of action. Also, only studies evaluating the effect of BMT on chronic heart failure were included and those in the setting of myocardial infarction were excluded.
Conclusion
Bone marrow transplantation appears to be promising in short term for treatment of heart failure. At 6 months, the use of bone marrow transplantation was associated with improvement in left ventricular ejection fraction, though no significant difference was seen for mortality. Until results of larger studies designed to study clinical endpoints are available, it remains unclear whether the improvement in ejection fraction is associated with any clinical benefit or not.
References
- Mozaffarian D, Benjamin EJ, Go AS (2014) Heart disease and stroke statistics-2015 update: a report from the american heart association. Circulation 131(4): e29-322.
- Roger VL, Weston SA, Redfield MM, Hellermann HJP, Killian J, et al. (2004) Trends in heart failure incidence and survival in a community- based population. JAMA 292(3): 344-350.
- Heidenreich PA, Albert NM, Allen LA, Konstam MA, Nichol G, et al. (2013) Forecasting the impact of heart failure in the United States: a policy statement from the American Heart Association. Circ Heart Fail 6(3): 606-619.
- Sanganalmath SK, Bolli R (2013) Cell therapy for heart failure: a comprehensive overview of experimental and clinical studies, current challenges, and future directions. Circ Res 113(6): 810-834.
- Mathieu M, Bartunek J, Oumeiri B (2009) Cell therapy with autologous bone marrow mononuclear stem cells is associated with superior cardiac recovery compared with use of nonmodified mesenchymal stem cells in a canine model of chronic myocardial infarction. J Thorac Cardiovasc Surg 138(3): 646-653.
- Tomita S, Li RK, Weisel RD, Mickle DA, Kim EJ, et al. (1999) Autologous transplantation of Bone Stem Cell s improves damaged heart function. Circulation 100(19): II247-256.
- Bel A, Messas E, Agbulut O, Richard P, Bruneval Pet al. (2003) Transplantation of autologous fresh bone marrow into infarcted myocardium: a word of caution. Circulation 108(1): II247-252.
- Waksman R, Fournadjiev J, Baffour R, Pakala R, Leborgne L, et al. (2004) Transepicardial autologous bone marrow-derived mononuclear cell therapy in a porcine model of chronically infarcted myocardium. Cardiovasc Radiat Med 5(3): 125-131.
- Liu JF, Wang BW, Hung HF, Chang H, Shyu KG, et al. (2008) Human mesenchymal stem cells improve myocardial performance in a splenectomized rat model of chronic myocardial infarction. J Formos Med Assoc 107(2): 165-174.
- Nagaya N, Kangawa K, Itoh T, Iwase T, Fujii T, et al. (2005) Transplantation of mesenchymal stem cells improves cardiac function in a rat model of dilated cardiomyopathy. Circulation 112(8): 1128-1135.
- Orlic D, Kajstura J, Chimenti S, Anderson SM, Li B, et al. (2001) Bone Stem Cell s regenerate infarcted myocardium. Nature 410(6829): 701705.
- Balsam LB, Wagers AJ, Christensen JL, Kofidis T, Weissman IL, et al. (2004) Haematopoietic stem cells adopt mature haematopoietic fates in ischaemic myocardium. Nature 428(6983): 668-673.
- Nygren JM, Jovinge S, Breitbach M (2004) Bone marrow-derived hematopoietic cells generate cardiomyocytes at a low frequency through cell fusion, but not trans differentiation. Nat Med 10(5): 494-501.
- Rota M, Kajstura J, Hosoda T, Vitale S, Esposito G, et al. (2007) Bone Stem Cell s adopt the cardiomyogenic fate in vivo. Proc Natl Acad Sci U S A 104(45): 17783-17788.
- Linke A, Muller P, Nurzynska D, Casarsa C, Torella D, et al. (2005) Stem cells in the dog heart are self-renewing, clonogenic, and multipotent and regenerate infarcted myocardium, improving cardiac function. Proc Natl Acad Sci U S A 102(25): 8966-8971.
- Bolli R, Tang XL, Sanganalmath SK, Rimoldi O, Mosna F, et al. (2013) Intracoronary delivery of autologous cardiac stem cells improves cardiac function in a porcine model of chronic ischemic cardiomyopathy. Circulation 128(2): 122-131.
- Gnecchi M, Zhang Z, Ni A, Dzau VJ (2008) Paracrine mechanisms in adult stem cell signaling and therapy. Circ Res 103(11): 1204-1219.
- Shintani Y, Fukushima S, Varela-Carver A, Lee J, Coppen SR, et al. (2009) Donor cell-type specific paracrine effects of cell transplantation for post-infarction heart failure. J Mol Cell Cardiol 47(2): 288-295.
- Ang KL, Chin D, Leyva F, Foley P, Kubal C, et al. (2008) Randomized, controlled trial of intramuscular or intracoronary injection of autologous Bone Stem Cell s into scarred myocardium during CABG versus CABG alone. Nat Clin Pract Cardiovasc Med 5(10): 663-670.
© 2017 Saurabh A, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)





























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






