- Submissions

Full Text
Modern Applications in Pharmacy & Pharmacology
Outcome of Pharmacists’ Counseling Infusion Center Patients on Chemotherapy
Sonia Amin Thomas* and Haley Ethridge
Philadelphia College of Osteopathic Medicine, USA
*Corresponding author: ASonia Amin Thomas, Philadelphia College of Osteopathic Medicine, Assistant Professor of Pharmacy Practice, Clinical Oncology Specialist/Clinical Pharmacist, Wellstar North Fulton Hospital: 3000 Hospital Blvd Roswell, GA 30076, USA
Submission: August 05, 2017; Published: September 08, 2017
ISSN 2637-7756Volume1 Issue1
Background
Cancer is increasing worldwide and more and more people have received chemotherapy treatment. Chemotherapy agents are cytotoxic drugs that kill cancer cells. Due to the increase in cancer, there has also been in an increase in research for cancer medications. This leads to new cancer drugs and new chemotherapy combination regimens for various cancers. For most people, the diagnosis of cancer causes many psychological and emotional effects which make it difficult to accept the ramifications of disease and treatment process. There are several support groups that patients can attend, but studies have shown that educating patients about cancer and chemotherapy in general can increase the patient’s compliance and satisfaction as well as decrease side effects and hospitalizations.
Physicians and nurses may not have the time or knowledge it requires to counsel these patients about each medication separately; so a clinical pharmacist can help play a huge role in this. It is estimated that by 2020, there will be a shortage of qualified oncology healthcare professionals including pharmacists. Clinical pharmacists can provide direct patient care and focus on drug management and toxicities. An infusion center is normally located inside of a hospital or close to a physician’s office where most patients receive chemotherapy treatment. Pharmacists can offer teaching and education to these patients and their families to help decrease anxiety and complications.
North Fulton Hospital has a very small infusion center with the capacity of about 5 patients at once. The infusion center is mainly filled with patients from a surgical and medical oncologist who is specialized in gynecologic oncology. Currently, the nurses hand patients a packet and explain some possible side effects and counsel the patient, but many patients still experience side effects and hospitalizations that could have been prevented with more education. There is an oncology specialist pharmacist who is an adjunct faculty member with a pharmacy school, so her time is limited between the school and the hospital. When she is at the hospital, she or her students have thoroughly counseled the patients in the infusion center; however, there has not been consistency. The purpose of this study is to determine patient satisfaction after being counseled by a pharmacist as well as to see if education decreased any hospitalizations while the patient was receiving treatment.
Objectives
To determine patient satisfaction after being counseled by a pharmacist and if hospitalizations were prevented after education by a pharmacist.
Methods
This was a single center, prospective, survey-based study at a small community hospital infusion center that consists of approximately five chairs. An oncology pharmacy specialist was available to provide counseling and education to patients while in the infusion center three days of the week. When the oncology specialist was unavailable, counseling was performed by other clinical specialists on staff. A standard chemotherapy handout was developed and one website (www.chemocare.com) was used to print drug handouts for patients. All clinical specialists at the hospital received training on the use of these handouts. The study consisted of 15 patients, over the course of six months (April- October 2016). Counseling and education was completed at the beginning and middle of each patient’s chemotherapy cycle. At the end of the cycle, a Likert-scale and short answer survey was administered to determine patient satisfaction and whether any hospitalizations occurred. All patients participating in the study were asked for permission to be counseled and whether they would want to fill out the survey at the end of their cycle. To be included in the study, patients only had to receive chemotherapy in the infusion center being studied.
The survey questionnaire consisted of 4 Likert-scale questions and 2 short answer questions. Patients were excluded if they did not consent to receive counseling or if they did not complete the survey. Data was recorded without any identifiers that can be linked to the subject and was stored on computer files with passwords only accessible to study personnel.
Results
Eight patients completed the survey from the fifteen total patients enrolled. The results of their questionnaires can be found in (Table 1). The questions were answered on a Likert-scale of 1-5 with 1 being strongly disagree and 5 being strongly agree. Additional questions included if they experienced side effects; if so, which ones; if knowledge was attainted as to what to do when the side effects were experienced; if hospitalization occurred, and if so, what required hospitalization and when was it. Of the five patients who mentioned experiencing side effects, three said they knew what to do to treat the side effects and prevent hospitalizations. Two patients had no side effects and no hospitalizations. All patients ranked their experiences with the pharmacist/counseling at neutral or greater, meaning no negative interactions or disagreeing with the prompts.
Table1:Survey Results.
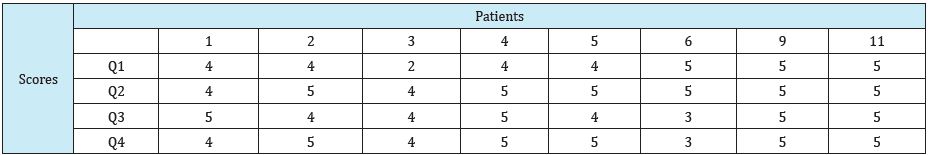
Q1: I felt very knowledgeable about my chemotherapy regimen before the pharmacist counseled me.
Q2: I felt very knowledgeable about my chemotherapy regimen after the pharmacist counseled me.
Q3: I knew exactly what to do if/when I had any side effects.
Q4: The pharmacist helped me understand exactly why & how the drug(s) worked
Nine patients were analyzed for Emergency Department (ED) admissions. A “good admission” was considered an admission to the ED in which patients had followed counseling to remain at home up to the point of admission being required based on pharmacist’s previous recommendations. Patients 5, 6, and 7 did not require ED admissions related to their chemotherapy regimens. Of the nine, three had no ED admission and the three patients who had been admitted were based on pharmacist counseling. The three patients who had a “bad admission” were due to improper patient response to counseling, improper evaluation of antiemetic therapy and counseling, and admissions prior to pharmacy counseling (Table 2).
Table2:Emergency Department Admissions.
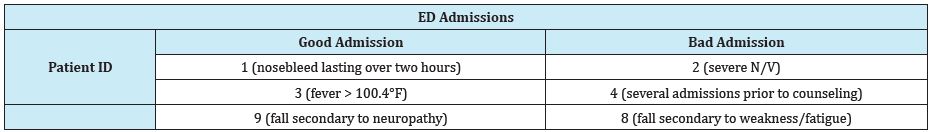
1: Patient was counseled if nosebleed lasts greater than several hours on Avastin, to go to the ED.
2: Patient had severe N/V on Gemzar which could have been prevented by counseling technique or follow up to make sure antiemetic regimen was appropriate and treating patient symptoms.
3: Patient had a fever of 100.9°F at home on Topotecan, was instructed to come to ED if fever is > 100.4°F but was not neutropenic and cultures came back negative..
4: Patient had prior admissions on chemotherapy before pharmacist counseling, pharmacy initiated counseling in the middle of patient treatment.
8: Patient admitted for head injury upon falling out of bed due to weakness/fatigue from carboplatin and paclitaxel which could have been prevented by patient following their pharmacists’ counseling and staying hydrated.
9: Patient admitted due to fall secondary to neutropenia from chemotherapy, unfortunately something that cannot be prevented through counseling.
Conclusion
With the increase in cancer in worldwide populations and the need for chemotherapy in more patient populations, high quality educators such as oncology pharmacists are in great demand. New and complicated chemotherapy regimens require educated physicians, nurses, and pharmacists for patient counseling. Oncology pharmacists’ counseling is a key role in patient education. Based on the results of the survey, patients at North Fulton Hospital felt confident in their knowledge of the chemotherapy regimen, of what to do in the occurrence of side effects, and how/why their drugs work. In regards to Emergency Department admissions, half of them were “good admissions” based on pharmacists’ recommendations; and the other half were before counseling, due to patient no adherence to recommendations or uncontrolled antiemetic therapy.
Some limitations of this study include the small population, various pharmacists giving counseling information, and not every pharmacist who counseled was trained in oncology. Even though the pharmacists and training varied, they were all given standardized counseling packets for each chemotherapy agent to present to the patients. Time was also a limitation for many pharmacists due to their other clinical responsibilities, so some patients we not counseled until the 2nd or 3rd cycle of chemotherapy. If oncology patients were admitted to any other ED than North Fulton without relaying this information, these admissions may not have been included in the study for lack of knowledge. If patients reported side effects to their oncologists only, there was no direct communication between pharmacy and oncologists, so these side effects may be missed in reporting. Future studies should include larger patient populations, multiple centers, and collaboration between oncologists and pharmacists to help strengthen our recommendation of the importance of pharmacist counseling in oncology patients.
© 2017 Sonia Amin Thomas, et al. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






