- Submissions

Full Text
Experiments in Rhinology & Otolaryngology
Metastatic Atypical Fibroxanthoma: Case Report of an Uncommon Pathology in the Head and Neck
Luis Boccalatte*, Alejandro Yanzón De la Torre, Pedro Picco and Natalia Gómez
Head and Neck Section, Hospital Italiano De Buenos Aires, Argentina
*Corresponding author: Luis A Boccalatte, Head and Neck Section, Hospital Italiano De Buenos Aires, Paraguay 40922A, Buenos Aires, Argentina
Submission: March 26, 2018; Published: June 08, 2018

ISSN 2637-7780 Volume1 Issue5
Abstract
Atypical fibroxanthoma (AFX) is an uncommon skin neoplasm developed mainly in the head and neck region in older senior patients. Prolonged sun exposure, actinic damaged, history of previous neoplasms and immunosuppressant are considered the most important risks factors. Subcutaneous extension of these tumors is related to a more aggressive biology. Metastatic extension is extremely rare but might lead to a fatal outcome. Differential diagnosis might be a challenge for pathologist due to its uncharacteristic features. We report the case of an elder patient who presented a recurrent AFX and who developed lung and lymph node metastasis. Even though treatment with chemotherapy and radiation was proposed, the patient final passed away due to a worsening of his condition.
Keywords: Atypical fibroxanthoma; Metastases; Skin neoplasm
Introduction
Atypical fibroxanthoma (AFX) is a rare skin malignancy generally developed in elderly male patients with actinic damage. Due to its low rate of metastasis, it is considered a benign neoplasm [1,2]. Metastatic AFXs occur in fewer than 6% of patients. Although many risks factors have been described, older age and deep tissue invasion are the most important. We present a case of an elderly patient with metastatic disease; due to its uncommon presentation we made a small review of the most outstanding features of this challenging pathology.
Case Report
Figure 1: 1A. CT scans showing a nodular mass in the left occipital region of the scalp (yellow arrow). 1B.Low density changes in the external table of the cranium are evidenced (yellow arrow); these ariations are suggestive of metastatic disease. 1C. Pulmonary secundarism. A speculated mass is shown in the upper right lobe; bilateral nodules with irregular borders and ground-glass attenuation are also seen
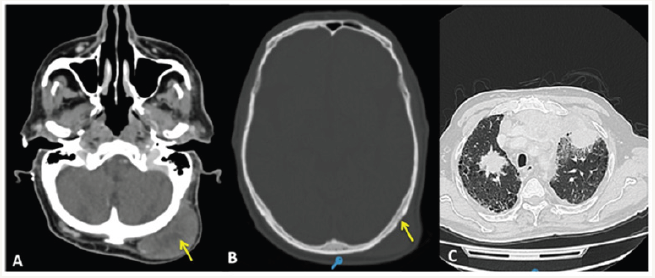
We present the case of a 77-year-old male patient who was referred to the head and neck surgery service for a skin lesion on the scalp. He complained of a painless, ulcerated, elevated nodule, with 1-year progression. A full thickness resection with a 1cm margin was performed, and AFX was diagnosed after final immunohistochemistry (IHC) analysis. The AFX recurred after 2years, with an ulcerated, firm, erythematous scalp nodule associated with an enlarged neck and supraclavicular lymph nodes. A CT scan showed bone and lung secundarism as well as cervical, supraclavicular, and mediastinal adenopathies Figure 1. A fine-needle aspiration (FNA) biopsy confirmed both primary and secondary lesions Figure 2. The oncological board committee recommended surgical and adjuvant treatment; however, the patient’s condition worsened, and the family and attending team ultimately decided to submit to palliative care.
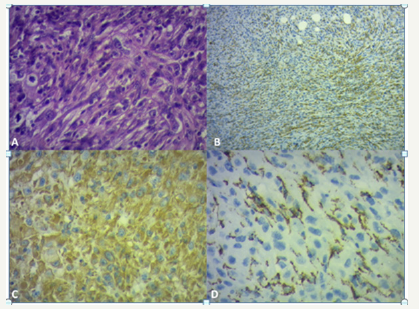
Figure 2: 2A. Histological examination that shows atypical pleomorphic cells with multiple mitotic figures (H&E, ×400). 2B and C. Positive immunostaining with CD68 (×400). 2D. Positive immunostaining with vimentin (×400)
Discussion
AFX is an uncommon mesenchymal tumor that represents 0.2% of all skin tumors. Regarded as a benign skin tumor, is usually seen in sun-damaged skin, mainly in senior patients, with an average age of 71 years, with a male-to-female ratio of 4:1 [1-5]. It most often arises in sun-exposed areas, predominantly in the head and neck region. Less frequently appears in trunk and extremities, usually in young people. Other risk factors described are traumas, ionizing radiation, and history of previous skin neoplasms. Immunosuppressant may also be considered a relevant factor [1,3].
AFX usually presents as an elevated, reddish, painless solid nodule limited to the dermis; it rarely exceeds 2cm in diameter, and the center might be ulcerated. Its histological description includes atypical spindled and pleomorphic cells with numerous bizarre mitotic figures and hyper chromatic multilobulated nuclei; no established pattern of distribution is recognized. They are generally restricted to the reticular dermis, but some lesions may extend into the upper one-third of the sub cutis [1,2,6,7].
Some researchers consider AFX a superficial variant of malignant fibrous histiocytoma (MFH) or undifferentiated pleomorphic sarcoma (UPS), which is both histological and immunohistochemically indistinguishable from AFX [3,6] However, AFX is generally limited to the dermis, with minimal subcutaneous tissue involvement .
According to the latest classification which replaces MFH and UPS [8,9], if the tumor invades the subcutaneous tissue should be reclassified as a pleomorphic dermal sarcoma (PDS). Other differential diagnoses include melanoma, derma to fibroses coma, and sarcomas. The IHC analysis might determine the final diagnosis; it is usually negative for S100, CD23, epithelial membrane antigen (EMA), MELAN A, cytokeratin, and desmin. However, there are no specific stains to identify AFX, which generally return positive results for vimentin, CD 10, CD 99, and CD 68. Surgery has been described as the therapy of choice [1, 3-8]. A 1 cm has been the average margin used, but some authors have proposed a 2cm margin [1,4,7]. Both wide local excision (WLE) and Mohs micrographic surgery (MMS) have shown excellent results, although there many reports with some contradicting results in terms of recurrence with MMS vs. WLE. However, in a recent review, MMS has proved to have a lower rate of recurrence [9]. The rate of recurrence for WLE and MMS is 8 and 0-4,6% respectively. However, surgery (in general) with oncological safety margins remains to be the best option as there is still no clear evidence of the best option of surgical treatment. It is important to mention that the whole management should be directed towards the prevention of local recurrences.
AFX has poor metastatic potential (1%) 7. However, even cases with minimal subcutaneous involvement can lead to death. The reported rate of recurrence and metastasis is around 2-20% and less than 6%, respectively [1,3,6,7]. Multiple local recurrences are also described but they are extremely rare, and they are usually associated with immunosuppressant. The median time reported for these events to arise is between 6 to 24 months. Metastases are generally recognized as cervical lymph nodes or in parotid, lungs and peritoneum. Even though the main mechanism for metastases still puzzles researchers, transit metastases have been investigated.
Vascular and perineural invasion, older age, insufficient margins of resection, necrosis, and deep tissue invasion have been described as risk factors for both recurrence and distal metastases. Earlier recurrences are associated with worse outcomes due to a more aggressive biology of the tumor. Metastatic disease, as well as in other oncologic pathologies, gives the patient a poor prognosis. Recurrences or incomplete margins might be treated with a new surgery or local radiotherapy [6,9]. Hence, no specific treatment has improved overall survival; in general, these treatments are used as palliative treatment with no intention to cure. On the other hand, molecular targeted therapies are yet to proven, being a promising shield of treatment [9].
Conclusion
AFX remains to be a challenging and unusual dermal pathology. Long distance metastases are extremely rare due to its benign biological behavior. However, in those cases with deeper invasion might lead to a fatal outcome associated with a more aggressive biology. Some of these tumors are considered to be a dermal pleomorphic sarcoma. Surgical management in all its forms continues to be the chosen treatment.
Acknowledgement
The authors thank Ana Morandi for her expertise and help in the histological figures. None of the authors has any direct or indirect commercial or financial support associated with the publication of this paper.
References
- Koch M, Freundl AJ, Agaimy A, Kiesewetter F, Künzel J, et al. (2015) Atypical fibroxanthoma-histological diagnosis, immunohistochemical markers and concepts of therapy. Anticancer Res 35(11): 5717-5735.
- Wang WL, Torres Cabala C, Curry JL, Ivan D, McLemore M, et al. (2015) Metastatic atypical fibroxanthoma: a series of 11 cases including with minimal and no subcutaneous involvement. Am J Dermatopathol 37(6): 455-461.
- Davidson JS, Demsey D (2012) Atypical fibroxanthoma: clinicopathologic determinants for recurrence and implications for surgical management. J Surg Oncol 105(6): 559-562.
- Zogbi L, Juliano C, Neutzling A (2015) Atypical fibroxanthoma. J Surg Case Rep 2015(3).
- Lee SS, Lewis JM, Liaw K, Bushkell LL , Young YD, et al. (2015) Recurrent atypical fibroxanthoma with satellite metastasis. J Cutan Pathol 42(1): 56-60.
- Kim JP, Ko GH, Kim JY, Woo SH (2014) Atypical Fibroxanthoma in Head and Neck. Clin Exp Otorhinolaryngol 7(1): 73-75.
- Hussein MR (2014) Atypical fibroxanthoma: new insights. Expert Rev Anticancer Ther 14(9): 1075-1088.
- Polcz MM, Sebaratnam DF, Fernández Peñas P (2017) Atypical fibroxanthoma management: Recurrence, metastasis and diseasespecific death. Australas J Dermatol 59(1): 10-25.
- Soleymani T, Tyler Hollmig S (2017) Conception and management of a poorly understood spectrum of dermatologic neoplasms: atypical fibroxanthoma, pleomorphic dermal sarcoma, and undifferentiated pleomorphic sarcoma. Curr Treat Options Oncol 18(8): 50.
© 2018 Luis Boccalatte. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






