- Submissions

Full Text
COJ Nursing & Healthcare
Sensory Modulation in an Inpatient Adolescent Psychiatry Unit
Jocelyn C Perez*
Director of Nursing for Behavioral Health Metropolitan Hospital NYC Health/Hospitals, USA
*Corresponding author: Jocelyn C Perez, Director of Nursing for Behavioral Health Metropolitan Hospital NYC Health/Hospitals, USA, Email:jocelyn.perez@nychh.org
Submission: April 20, 2018;Published: July23, 2018

ISSN: 2577-2007Volume3 Issue5
Abstract
Introduction: Violence, as a problem that has emerged in the workplace, particularly in areas such as emergency rooms and in psychiatric units, has a traumatizing effect for both patients and staff. Sensory Modulation as a therapeutic modality has high impact on patient and staff safety and also on patient experience. With its introduction to this inpatient adolescent psychiatric unit, the number of violent episodes was reduced, along with use of restraints. As the number of assaults of patient-to-patient and patient-to-staff has gone down, the number of staff compensation claims related to staff injury has also diminished. The initiative aligns with the organizations priorities of enhancing the quality of care and patient and staff safety.
Purpose: This Project provides an essential therapeutic modality for other health care organizations to consider in that it represents a “best practice” as well as a cost-effective method to assist psychiatric patients with self-regulation and self-management tools that they can use both in the units and after discharge. It is an evidence based practice (EBP) used by both patients with mental illness and those with developmental disability.
Study design, material and method: The facility’s method of self-study and needs assessment, a review of relevant literature and existing best practices on alternatives to use of restraints, led staff to come up with this pilot project. Initial results were very positive and the twofold goals of restraints reduction and decrease in assaults and fights were achieved. Since 2016, the results have been mostly consistent and ongoing for all of the adolescent patients. The transformation of a simple empty room to an easy to manage Sensory Room lends itself to opportunities to improve both the quality of service and safety of all the patients and staff. Staff was trained as to the use of the Sensory Room and then the modality introduced to the patients, either individually or in groups. Staff screens patients for voluntary participation. Registered Nurses interview patients for assessment and reassessment and observe them with regards to their responses to the modality.
With the increasing use of the Sensory Room, Activity Therapists and Nursing have also introduced the use of the Sensory Baskets as an enhancement to the Room. The basket contents include simple items such as rolls of bubble wraps, lotion with either lavender or cinnamon scent, markers with different scent of fruits, portable massagers, etc. Using PDSA (Plan, Do, Study, Act) model, we added metrics to the use of this modality, among which are: restraints use and number of assaults that occur in the unit.
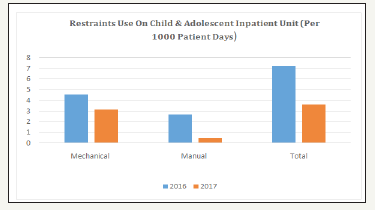
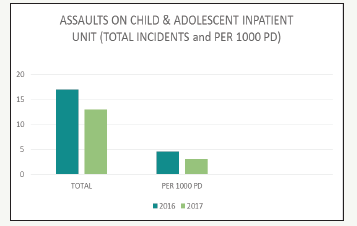
Result: Using data to compare results after the initiation of the Sensory Modulation initiative, the hospital achieved Reduction in the use of restraints from 7.21 per 1000 patient days in 2016 to 3.62 per 1000 patient days in 2017. There is also a reduction in the number of assaults (patient to patient and patient to staff) from 4.54 per 1000 patient days in 2016 to 3.14 per 1000 patient days in 2017.
Conclusion: The program is ongoing and sustainable, utilizing cost effective resources-a room and a small dedicated budget to buy lost cost items for patient use of the Sensory Basket. The project has established a good track record, evidenced by the reductions in overall assaults and use if restraints from 2016 to 2017, in both raw total numbers as well as per 1000 patient days. The initiative has been replicated in the other adult inpatient units and has initial positive results in the reduction of assaults and fights as well as the use of intramuscular injections. Future studies are to be correlated to patients’ ability to apply the stress reduction modality learned from using Sensory Modulation.
Introduction
Workplace violence has been steadily increasing in healthcare facilities. Aside from the traumatizing effect for the patients and staff, it has created crippling costs related to both patient and staff injuries and increased manpower hours consistent with covering for compensation claims because of work-related injuries. This Community Hospital has an 18 adolescent inpatient bed for patients who have mental illness and whose ages range from 10 to 17. The patients mostly come from an urban neighborhood in New York City that suffers from many social issues, such as living below the poverty line, teenage pregnancy, AIDs, drug abuse, homelessness and has the highest concentration of public housing in the United States. As such, incidences of trauma victimization are quite common among the patients treated in this facility. Additionally, these patients present with co-morbid disorders such as substance abuse. These patients come in with diagnosis of mood, anxiety and thought disorders, alcohol and drug addictions, and attention deficit hyperactivity disorder (ADHD), Conduct Disorders and other disruptive behaviors as well as grief and past abuse issues [1].
Patient assaults are the most common behavioral health category in most inpatient psychiatric settings and in large settings of care. It is a priority concern not only for its relative frequency, but for the scope and its effects on the course of treatment, care and safety of all patients and staff, their performance and work satisfaction. For purposes of this study, the term “assaults” as used in this 18 bed adolescent inpatient psychiatric unit, is defined by the New York State Office of Mental Health (SOMH) as “physical attack using force or violence in which a patient is either a victim or aggressor. Manual Restraints, as defined by SOMH, is the use of a manual or physical method to restrict a person’s freedom of movement or normal access to his or her body. The term “manual restraint”, means and includes the term “physical restraint”. This treatment modality of Sensory Modulation provides an essential remedy for other health care organizations in that it represents a “best practice” as well as a cost-effective method to assist psychiatric patients with self-regulation and self-management tools that they can use both in the units and after discharge [2].
The use of Sensory Modulation supports a therapeutic, traumainformed culture of healing and recovery that meets the goals of significantly reducing the use of restrictive interventions such as restraints and seclusion; providing services that promote recovery, trauma- informed and patient-centered care; and determining techniques or strategies that provides positive alternatives to restraints. With the impetus of further reducing the use of coercive interventions such as restraints, the hospital was awarded a small grant to transform an essentially empty room into a state of the art Sensory Modulation Room. The hospital’s primary goal is to provide a calming, relaxing space for patients and serve as an area where they can learn skills to self-regulate to decrease their anxiety and agitation, increase their functioning as well as life-long effective coping skills after discharge [3].
Purpose
A study has shown that therapeutic modalities that incorporate the use of Sensory Modulation have positive effects on patients of all ages, diagnoses and cognitive functioning. Over the past three decades, research has expanded the use of sensory modulations rooms to have positive effects on patients who have mental illness and those with developmental disability. One study showed that 98% of the participants described a reduction in stress levels, with the largest change in those reporting the highest stress levels prior to the intervention [1]. The facility, in its effort to reduce the use of restraints and to decrease assaults among its adolescent patients, embarked on this project in the last quarter of 2015 with the goal in mind of achieving its goals of restraints and assault reduction.
Material and Method
With the impetus of further reducing the use of coercive interventions such as restraints, the hospital applied for a small grant provided by the Health System to transform an essentially empty room into a state of the art Sensory Modulation Room. The primary goal is to provide a calming, relaxing space for patients and serve as an area where they can learn skills to self-regulate to decrease their anxiety and agitation, increase their functioning as well as life-long effective coping skills after discharge. The grant funds have been allocated for painting of the walls with soothing color and furnishing equipment that assist in easing tension through stimulation of the senses of smell, touch, sight, and hearing. Examples of such equipment are the giant bean bag that provides soothing music when a patient is lying down, several multi-colored soft punching bags that provide sound when punched, relaxation CDs, stress balls, weighted blanket, some aromatherapy items such as lavender and cinnamon and ordinary bubble wrap that patients use to keep focus on certain tasks [4].
The creation out of a simple empty room of an easy to manage Sensory Room lends itself to opportunities to improve both the quality of service and safety of all the patients and staff. Staff was trained as to the use of the Sensory Room and then the modality introduced to the patients, either individually or in groups. Patients are screened for voluntary participation [5]. Staff interview patients for assessment and reassessment purposes and observe them as to their responses to the modality.
With the increasing use of the Sensory Room, Activity Therapists and Nursing introduced the use of the Sensory Baskets as an enhancement to the Room. The basket contents include simple items such as rolls of bubble wraps, lotion with either lavender or cinnamon scent, markers with different scent of fruits, portable massagers, etc. Using PDSA (Plan, Do, Study, Act) model, we added metrics to the use of this modality, among which are: restraints use, number of assaults that occur in the unit. All the outcomes in these metrics are reported daily in the Safety Huddles, via occurrence reports and monthly to the Departmental Quality Improvement Committee [6].
Trained staff in the use of the Sensory Room introduces this modality on admission and incorporates report and observation in the patients Individual Crisis Plan. Based on information obtained from the patient or the significant other and staff observation of the patients while in the unit, a Sensory Modulation modality is recommended to address the issue relevant to any particular patient. A staff is assigned to assist the patient during crisis situations. The clinical team discusses with the patient the effect and effectiveness of the modality in reducing agitated states. Patients are observed in a continuous, uninterrupted manner during the whole process and then the benefits included in the patient’s treatment plan.
This initiative has greatly impacted the use of restraints among this population and decreases the violent episodes of assaults between patients to patients and patients to staff. With 2 years of positive outcomes in this unit, 4 other adult units have now started to utilize sensory baskets designed with patient and staff safety in mind [7].
Result
Initial results were very positive and the twofold goals of restraints reduction and decrease in assaults and fights were achieved. The results have been mostly consistent and ongoing for all of the adolescent patients since 2016. Staff has gained the comfort and competence in the use of the modality. Patients have continued to use the Room and the basket gaining the skills for self-regulation. Figure 1 provides information on the number of restraints use in 2016 and 2017. Both graphs indicate the comparison of total raw number of restraint episodes/incidents between these two years. Figure 2 demonstrates the restraint use comparing 2016 and 2017 using per 1000 patient days.
Figure 1:Total number of restraint incidents between 2016 and 2017.
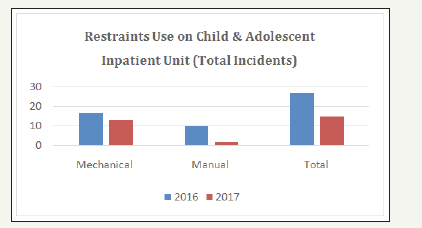
Figure 2:Total number of incidents per 1000 patient days.
The unit staff has also noted positive results since they started using Sensory Modulation as a strategy to decrease violent incidents. These positive results are:
A. Strengthened relationships among interdisciplinary staff resulting from enhancing communication among the staff and the patients
B. Feeling of pride in using an evidence based practice that works
C. Feeling of safety related to hardwiring the culture of “No Harm” among patients and staff.
Discussion
While the unit has achieved positive results in reduction of the use of coercive interventions such as restraints and the number of violent assaults in the unit, they find it very significant to include lessons learned during the transition from beginning of the initiative to the current practice that has been hardwired in the unit’s culture. These lessons learned include:
A. Patient empowerment with regards to treatment choices is key to treatment adherence
B. Discovering the patients’ fear and supporting them counts more than offering medication and indicating “you need this”
C. There is a person in every patient.
D. Patient participation provides opportunities to know them more and remove boundaries between staff and patients
E. Proactive approaches are important to identify deescalation strategies
F. Small cost can make significant changes
G. Data is key to support changes
H. Senior Leadership buy-in is critical
I. Active patient and family engagement is an important tool to ensure safety
J. Creating and carrying out a vision of an environment that is free of coercion Figure 3.
Figure 3:Shows the comparison of the number of assault incidents between 2016 and 2017.
Conclusion
Implementation of an evidence-based patient centered-care clinical practice has contributed to positive outcomes related to patient and staff safety as well as a finding an alternative solution to use of highly restrictive interventions such as restraints [6]. Understanding that the patient is a person who can make choices, it has also enlightened the staff that empowering the patients and providing them the voice in their treatment adds significant value to patient adherence. Sensory modulation has now been replicated in the adult units and the department is beginning to see a decline in our violent episodes. Additionally, there is mutual learning that occurs between patients and staff- patients sharing with staff what happens to them when they are upset, what triggers them and what helps them; and staff teaching them new skills using sensory modulation or re-enforcing previously learned skills the patients can use while in the hospital and after discharge [7].
References
- Melvin M, McNamara G, West M, Gordon M (2017) An evaluation of the use and efficacy of a sensory room within anadolescent psychiatric inpatient units. Aust Occup Ther J 64(3): 253-263.
- Andersen C, Kolmos A, Volkmar S Sippel V, Stenager E (2017) Applying sensory modulation to mental health inpatient care to reduce seclusion and restraint. A Case Control Study 71(7): 525-528.
- Barton E, Reichow B, Schnitz IC, Smith IC, Sherlock D (2015) A systematic review of sensory-based treatments for children with disabilities. Res Dev Disabil 37: 64-80.
- Champagne T (2011) Sensory modulation and environment: Essential elements of occupation (3rd edn), Melbourne, Australia.
- Champagne T, Stromberg N (2004) Sensory approaches in inpatient psychiatric settings: Innovative alternatives to seclusion and restraint. Journal of Psychosocial Nursing and Mental Health Service 42(9): 34-44.
- Smith SA, Press B, Koenig KP, Kinnealy M (2005) Effects of sensory integration intervention on self-stimulating and self-injurious behaviors. American Journal of Occupational Therapy 59: 418-425.
- Stagg VS (2015) Injurious assault rates on inpatient psychiatric units: Associations with staffing by registered nurses and other nursing personnel. Psychiatric Services 66(11): 1162-1166.
© 2018 Jocelyn C Perez. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)





























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






