- Submissions

Full Text
Advancements in Bioequivalence & Bioavailability
The Coming Age of Particle Vaccines
Walpita Pramila*
Department of Tropical Medicine, Medical Microbiology and Pharmacology John A. Burns School of Medicine, USA
*Corresponding author: Walpita Pramila, Department of Tropical Medicine, Medical Microbiology and Pharmacology John A, Burns School of Medicine, 651 Ilalo Street, BSB 320, Hawai, USA
Submission: February 12, 2018 Published: April 04, 2018

ISSN 2640-9275 Volume1 Issue1
Introduction
Vaccine technology is needed to combat unexpected uncontrolled viral disease outbreaks rapidly. It is desired to have a vaccine ready if possible within less than three months in such situations. The traditional way of making vaccines such as inactivated or live attenuated viruses in general are highly effective, in some cases they fail to provide adequate immunogenicity, safety or even cause adverse events. In the case of live attenuated vaccines, achieving a stable optimally attenuated virus is often difficult and there is the potential for reversion. Transmission to the immunecompromised individuals is an additional concern. Inactivated vaccines run the risk of inducing enhanced disease. Additionally, it is not feasible for either an inactivated or an attenuated vaccine to be ready in a short time. Subunit vaccines have not been successful to date for human use. Various techniques of engineering the virus and vectored approaches are being also attempted.
Particle technology is rapidly emerging to develop future vaccines. Already Virus-Like-Particle (VLP)-based vaccines such as Gardasil (Merck & Co) and Cervarix (GlaxoSmithKline), are available to prevent human papilloma virus infection. Many other VLP vaccines are under development.
It is natural for the immune response to improve after viral infection. A designed particle vaccine must have the size and the immunogenicity of the virus for immune response to be effective. Such a vaccine particle must be recognized by the pattern recognition receptors (PRRs) and resulting signaling path ways to generate cytokines and chemokines for necessary immune response. In the absence of the viral genome these particles are safe. The ideal such particle is a Virus-Like-Particle (VLP). Such a VLP structure may be generalized by replacing Matrix protein (M) core by a metal, polymer or other (Generalized Structure) as shown in Figure 1 below, but not the immunogenic proteins; here the vaccine efficacy depends on how well these relevant viral proteins are attached to the core, mostly a random event leading to variability in the immune response. Additionally, properties of such a nano-particle is expected to substantially deviate from that of the virus. These are fundamental issues that lead to consistency or inconsistency in vaccine efficacy, in situations where M is replaced by an alternative; safety might be a concern also depending on with what M is replaced.
Figure 1: VLP structure may be generalized by replacing Matrix protein (M) core by a metal, polymer or other (Generalized Structure).
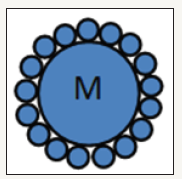
Generalized Structure
Center core
Matrix Protein (M) replaced by
- Metal or
- Polymer or
- Other (e.g. adjuvant)
Center core
Immunogenic proteins
- Protein F
- Protein G
- Protein-3
- Protein-4 etc.
It is natural to have Matrix Protein (M) as the core in the VLPs because it is a part of the virus. In principle those cells (e.g. Mammalian cells) that can reproduce the virus can also generate VLPs when subjected to the relevant proteins (M, F, G etc.), Figure 2. The mammalian cell derived VLPs, batch to batch, are reproducible with consistent protein distribution and show acceptable temperature stability over wide range. As a result, properties of the virus are well reproduced in the VLP lots as observed from vaccine studies that are described below.
Figure 2:
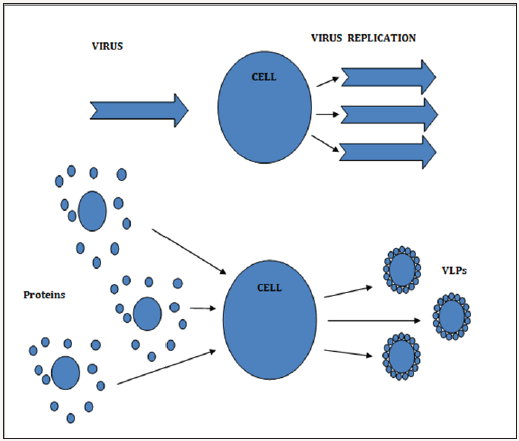
We have shown that Mammalian cell derived Nipah VLPs protect in the hamster model with single and multiple inoculations [1]. The adjuvanted and non adjuvanted NIV VLPs were tested in the hamster model with 7 hamsters in each group. The adjuvants used were MPLA, CpG, CpG/Alum. NiV VLP-immunized hamsters produced high level of neutralizing antibody (NtAb) titers and the hamsters were protected from lethal challenge with Nipah virus.
We have also shown that Mammalian cell derived Respiratory Syncytial VLPs protect the Lower as well as the upper respiratory tract [2]. With two vaccine doses. We expect that in an optimum design, protection with single dose is possible.
Fundamentally, VLPs can be derived for any virus; this is possible in a short time. ZIKA proteins were assembled and VLPs were made in less than 2 months. The technology has the potential to handle unexpected and uncontrolled outbreaks rapidly.
References
- Walpita P, Cong Y, Jahrling PB, Rojas O, Postnikova E, et al. (2017) VLP-based vaccine provides complete protection against nipah virus challenge following multiple-dose or single-dose vaccination schedules in a hamster model. NPJ vaccines (2): 21.
- Walpita P, Johns LM, Tandon R, Moore ML (2015) Mammalian cellderived respiratory syncytial virus-like particles protect the lower as well as the upper respiratory tract. PLOS One 10(7): e0130755.
© 2018 Walpita Pramila. This is an open access article distributed under the terms of the Creative Commons Attribution License , which permits unrestricted use, distribution, and build upon your work non-commercially.
 a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in
a Creative Commons Attribution 4.0 International License. Based on a work at www.crimsonpublishers.com.
Best viewed in 







.jpg)






























 Editorial Board Registrations
Editorial Board Registrations Submit your Article
Submit your Article Refer a Friend
Refer a Friend Advertise With Us
Advertise With Us
.jpg)






.jpg)













.bmp)
.jpg)
.png)
.jpg)














.png)

.png)



.png)






